Overview
Mechanism of action
Local anesthetics reversibly block nerve conduction near their site of administration, thereby producing temporary loss of sensation in a limited area. Nerve impulse conduction is blocked by inhibition of sodium channels at the nerve endings and along the axon. This causes a decrease in nerve cell membrane permeability to sodium ions, possibly by competing with calcium-binding sites that control sodium permeability. This change in permeability results in decreased depolarization and an increased excitability threshold that ultimately prevents the nerve action potential from forming. [1, 2, 3]
Indications
Local anesthetics are used for infiltration and nerve block anesthesia. Because of variation in systemic absorption and toxicity, the ideal choice of local anesthetic and concentration depends on the intended procedure. Infiltration anesthesia is often used for minor surgical and dental procedures. Nerve block anesthesia is used for surgical, dental, and diagnostic procedures and for pain management. [4, 5]
Uses for infiltrative anesthetics are as follows:
-
Subcutaneous infiltration (IV placement, superficial/shave biopsy, suturing)
-
Submucosal infiltration (dental procedures, laceration repairs)
-
Wound infiltration (postoperative pain control at incision site)
-
Intraarticular injections (postsurgical pain control, arthritic joint pain control)
Infiltrative Local Anesthetic Agents
Dosage and administration guidelines
Lower concentrations of local anesthetics are typically used for infiltration anesthesia.
Variation in local anesthetic dose depends on the procedure, the degree of anesthesia required, and the individual patient's circumstances.
Reduced dosage is indicated in patients who are debilitated or acutely ill, in patients who are very young or very old, and in patients with liver disease, arteriosclerosis, or occlusive arterial disease.
Administrative techniques
Patient comfort is essential during administration of local anesthetic agents. Warming the local anesthetic solution prior to administration to 25-40o C has been recommended. [8, 9]
Infiltration anesthesia is accomplished with administration of the local anesthetic solution intradermally (ID), subcutaneously (SC), or submucosally across the nerve path that supplies the area of the body that requires anesthesia. [4, 3] See the image below.
A common administrative technique is to inject the local anesthetic subcutaneously in a circular pattern around the operative site; this administration is often referred to as field block technique. [1, 3]
Deciphering drug concentrations and dilutions
Concentrations: Drug concentration is expressed as a percentage (eg, bupivacaine 0.25%, lidocaine 1%).
-
Percentage is measured in grams per 100 mL (ie, 1% is 1 g/100 mL [1000 mg/100 mL], or 10 mg/mL).
-
Calculate the mg/mL concentration quickly from the percentage by moving the decimal point 1 place to the right, as follows:
Bupivacaine 0.25% = 2.5 mg/mL
Tetracaine 0.5% = 5 mg/mL
Lidocaine 1% = 10 mg/mL
Viscous lidocaine 2% = 20 mg/mL
Benzocaine 20% = 200 mg/mL
Dilutions: When epinephrine is combined in an anesthetic solution, the result is expressed as a dilution (eg, 1:100,000).
-
1:1,000 means 1 mg per 1 mL (ie, 0.1%)
-
1:10,000 means 1 mg per 10 mL (ie, 0.01%)
-
1:2,000 means 1 mg per 2 mL (ie, 0.05%)
-
1:20,000 means 1 mg per 20 mL (ie, 0.005%)
-
0.1 mL of 1:1000 epinephrine added to 10 mL of anesthetic solution = 1:100,000 dilution, or 0.01 mg/mL
Epinephrine content examples: From the information provided in Table 1 below, 50 mL of 1% lidocaine with epinephrine 1:100,000 contains 500 mg of lidocaine and 0.5 mg of epinephrine. [10]
Table 1. Epinephrine content in solution (Open Table in a new window)
Solution Volume |
1:100,000 (1 mg/100 mL) |
1:200,000 (1 mg/200 mL) |
1 mL |
0.01 mg |
0.005 mg |
5 mL |
0.05 mg |
0.025 mg |
10 mL |
0.1 mg |
0.05 mg |
20 mL |
0.2 mg |
0.1 mg |
Adverse effects
Adverse effects are usually caused by high plasma concentrations of a local anesthetic drug that result from inadvertent intravascular injection, excessive dose or rate of injection, delayed drug clearance, or administration into tissues with high rates of clearance. [1, 2, 11, 12] Possible adverse effects include the following:
-
CNS: High plasma concentration initially produces CNS stimulation (including seizures), followed by CNS depression (including respiratory arrest). The CNS stimulatory effect may be absent in some patients, particularly when amides are administered. Solutions that contain epinephrine may add to the CNS stimulatory effect. [1, 4, 5, 11, 12]
-
Cardiovascular: High plasma levels typically depress the heart and may result in bradycardia, arrhythmias, hypotension, cardiovascular collapse, and cardiac arrest. Local anesthetics that contain epinephrine may cause opposite effects, including hypertension, tachycardia, and angina. [1, 2, 4, 11, 12]
-
Other body systems can also experience adverse effects. [4, 5]
Transient burning sensation
Skin discoloration
Swelling
Neuritis
Tissue necrosis and sloughing
Methemoglobinemia (with prilocaine)
Allergic reaction to local anesthetics
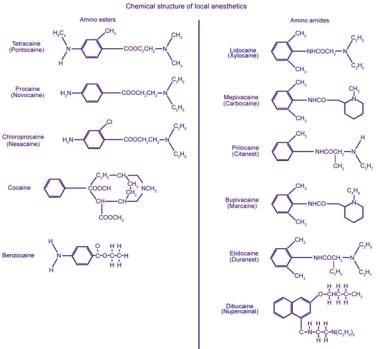
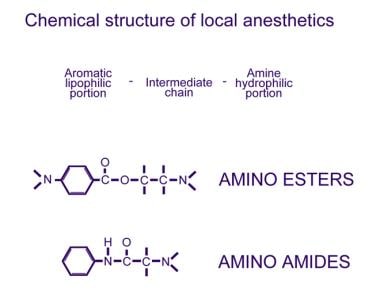
Most local anesthetic agents share the same basic chemical structure consisting of an aromatic ring, an intermediate chain, and a hydrophilic amine. The chemical structure of the intermediate chain consists of either an ester or amide, and is the link between the aromatic and hydrophilic segments. Local anesthetic agents are further classified by their intermediate chain into the amide group or the ester group (see the images below). This structural difference determines the pathway by which the agent is metabolized and its allergic potential. For example, amino amides undergo hepatic metabolism, whereas amino esters are metabolized in the plasma via plasma cholinesterases. Hydrolysis of amino ester compounds yields para -aminobenzoic acid (PABA), a well-known allergen, as an intermediate metabolite. Thus, amino esters are significantly more likely than amino amides to cause true allergic reactions. [13]
Dose, physiochemical variables, and pharmacokinetic properties of local anesthetics used for infiltrative injection (nondental use) are portrayed in the table below. A simple way to help remember which class a local anesthetic belongs to is to remember that the letter “i” appears twice in the spelling of an amide.
Actual hypersensitivity is rare and accounts for less than 1% of all reactions to local anesthetics. Allergic reactions may be attributed to other factors such as acute toxicity (eg, inadvertent intravascular injection that causes high plasma levels), psychomotor reactions (eg, patient is anxious or apprehensive), pharmacologic properties of local anesthetics, concurrent drug therapy (eg, tachycardia caused by epinephrine), or preservatives such as paraben or sulfites, which may be present in multidose vials. [2, 4]
Local anesthetics with a PABA ester-type structure seem to cause most anesthesia-related allergic reactions. Documented cross-sensitivity has been exhibited within the ester-based local anesthetics and structurally related compounds (eg, paraben preservatives). Hypersensitivity to the amide local anesthetics is rare.
Patients who claim to be allergic to lidocaine may actually be allergic to the preservative methylparaben. Preservative-free lidocaine may be obtained from individual ampules of lidocaine or from preservative-free lidocaine used by cardiologists and anesthesiologists.
Physiochemical variables
Onset of action, potency, and duration of action are determined by the pKa level, pH level, lipid solubility, protein binding, and vasodilatory effects of the specific local anesthetic. Increasing the dose by administering a high concentration shortens onset but increases potency and duration of action. Other factors that affect onset, potency, and duration are listed below. [2, 3, 13]
-
Onset of action
pKa level is the primary factor that determines onset of action.
A lower pKa level increases tissue penetration and shortens onset of action; this is because of the more lipid-soluble nonionized particles.
A pKa level that is lower than the pH level optimizes penetration.
Inflammation in the extracellular space may decrease the pH level and may slow onset of action.
The site of administration influences onset (ie, onset is prolonged in areas with increased tissue or nerve sheath size).
-
Potency
Anesthetics with high partition coefficients that increase lipophilic properties pass easily into the lipid nerve membrane.
The higher degree of vasodilation promotes vascular absorption, thereby reducing the locally available drug and decreasing potency.
The addition of epinephrine or sodium bicarbonate increases the pH level, thereby increasing nonionized particles, which are more lipid-soluble.
Generally, anesthetic solutions that contain premixed epinephrine contain preservatives; these solutions have the pH level adjusted lower to maintain stability of the epinephrine and antioxidants.
-
Duration of action
The addition of epinephrine to some local anesthetic solutions prolongs duration of action by causing vasoconstriction and decreasing systemic absorption.
The degree of protein binding primarily determines the duration of action; high protein binding increases the duration of action.
Increasing pH level (by addition of epinephrine or sodium bicarbonate) prolongs duration of action.
The table below summarizes amides for infiltrative injection.
Table 2. Amides for infiltrative injection (nondental use) [4, 3, 5] (Open Table in a new window)
Common Local Anesthetics Generic Name (Trade Name) |
Concentration(s) |
Maximum Total Adult Dose per Procedure* |
Volume of Maximum Total Adult Dose |
pH, pKa, Lipid Solubility (Partition Coeffecient [K]) |
Onset, Protein Binding, Duration |
Lidocaine (Xylocaine) |
1-2% |
4.5-5 mg/kg, not to exceed 300 mg |
30 mL of 1%; 15 mL of 2% |
pH: 5-7 pKa: 7.9 K: 2.9 |
Onset: < 2 min Protein binding: 64.3% Duration: 0.5-1 h |
Lidocaine with epinephrine |
1-2% lidocaine with epinephrine 1:100,000 or 1:200,000 |
7 mg/kg, not to exceed 500 mg |
50 mL of 1%; 25 mL of 2% |
pH: 3.3-5.5 pKa: -- K: -- |
Onset: < 2 min Protein binding: -- Duration: 2-6 h |
Bupivacaine (Marcaine, Sensorcaine) |
0.25% |
2.5 mg/kg, not to exceed 175 mg |
70 mL |
pH: 4-6.5 pKa: 8.2 K: 27.5 / 1565 (different buffer results) |
Onset: 5 min Protein binding: 95.6% Duration: 2-4 h |
Bupivacaine with epinephrine |
0.25% bupivacaine with epinephrine 1:200,000 |
Not to exceed 225 mg |
90 mL |
pH: 3.3-5.5 pK: -- K: -- |
Onset: 5 min Protein binding: -- Duration: 3-7 h |
Mepivacaine (Carbocaine, Polocaine) |
1% |
Not to exceed 400 mg |
40 mL of 1% |
pH: 4.5-6.8 pKa: 7.6-7.8 K: 0.8 |
Onset: 3-5 min Protein binding: 77.5% Duration: 0.75-1.5 h (with epinephrine: 2-6 h) |
*Administer by small incremental doses with frequent aspirations to prevent intravascular injection; administer the smallest dose and concentration required to achieve desired effect; avoid rapid injection |
|||||
Table 3. Esters for infiltrative injection (nondental use) [4, 3, 5] (Open Table in a new window)
Common Local Anesthetics Generic Name (Trade Name) |
Concentration(s) |
Maximum Total Adult Dose per Procedure* |
Volume of Maximum Total Adult Dose |
pH, pKa, Lipid Solubility (Partition Coefficient [K]) |
Onset, Protein Binding, Duration |
Procaine (Novocain) |
0.25-0.5% (via dilution) |
350-600 mg |
140-240 mL of 0.25%; 70-120 mL of 0.5% |
pH: 3.5-5 pKa: 9.1 K: 0.02 |
Onset: 2-5 min Protein binding: 5.8% Duration: 0.25-1 h |
Chloroprocaine (Nesacaine) |
1-2% |
Not to exceed 800 mg |
80 mL of 1%; 40 mL of 2% |
pH: 4.5 pKa: 9 K: 0.14 |
Onset: 6-12 min Protein binding: -- Duration: 0.5 h |
*Administer by small incremental doses with frequent aspirations to prevent intravascular injection; administer the smallest dose and concentration required to achieve desired effect; avoid rapid injection |
|||||
-
Infiltration of a local anesthetic.
-
Chemical structure of the 2 classes of local anesthetics, amino esters and amino amides.
-
Chemical structure of commonly used local anesthetics.