Practice Essentials
Ultrasonography for the detection of abdominal aortic aneurysm (AAA) has been shown to be sensitive, specific, and relatively simple to perform. [1, 2, 3, 4] Plummer et al demonstrated its utility as a point-of-care test in the emergency department (ED) by showing faster time to diagnosis and higher rate of survival of ruptured AAA. [5] Point-of-care ultrasonography (POCUS), which is performed at the bedside by physicians who are not specialists in imaging, has become possible thanks to technological advances that have led to use of a device with greater portability while maintaining image quality. Increasing use of POCUS in different specialties has made possible expanded physical examinations, timely decisions about patient care, and performance of safer medical procedures. [6] Further validation studies have shown that emergency medicine (EM) residents and, by extension, appropriately trained EM physicians are able to quickly and accurately identify AAA using ultrasound at the bedside. [7]
The most commonly used definition of an AAA is a maximum infrarenal abdominal aortic diameter greater than 3 cm on ultrasound or CT. [8, 9, 10]
POCUS performed by a physician at the bedside is standard practice in obstetric, emergency, and musculoskeletal medicine. When compared with formal sonography, POCUS is equivalent to screening for AAA and is as accurate in diagnosing deep venous thrombosis. [11]
It is important to remember, however, that while bedside ultrasonography can be especially useful in an unstable patient who cannot leave the ED or other acute care patient setting for computed tomography (CT) of the abdomen, it should never delay potentially lifesaving abdominal surgery when such surgery is immediately available and the diagnosis is strongly suspected. [12] In outpatient clinics, urgent care centers, and EDs, where ultrasound imaging may be delayed by hours or even days, POCUS can prove very helpful. POCUS can facilitate patient triage and allow diagnostic information to be gathered quickly. [13]
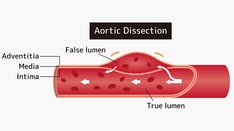
Rupture of an AAA often results in death, with a mortality of 85-90%. The risk of rupture of AAAs less than 4 cm diameter is negligible, but the risk increases dramatically once the diameter reaches 5 cm, with the risk of rupture increasting to 30-50% for diameters greater than 8 cm. Although CT is considered the modality of choice for a ruptured AAA, ultrasound is better than CT at identifying intraluminal fissures, inhomogeneities, and dissections. The presence and characteristics of an intraluminal thrombus on ultrasound may help identify the risk of rupture. [8, 9, 10]
A leaking or ruptured AAA classically presents in patients who are older than 60 years who have a history of hypertension and atherosclerosis and who experience severe abdominal, back, or flank pain after an episode of syncope. [14] Although AAA is more common in men than in women, the incidence of rupture is greater in women because the growth rate of AAA is significantly greater in women than in men. [15]
Unfortunately, less than 50% of patients with ruptured AAA present with the classic triad of syncope followed by back, flank, or abdominal pain and a pulsatile abdominal mass. [16] Up to 30-60% of patients with AAA are initially misdiagnosed. [17, 18, 19, 20] Be careful not to confuse AAA with more benign diagnoses such as renal colic, mechanical back pain, or diverticulitis.
Maintain a high index of suspicion in patients older than 60 years who present with pain in the abdomen, back, flank, or groin. Other risk factors include family history of AAA, male sex, and history of hypertension, smoking, coronary artery disease, diabetes mellitus, hyperlipidemia, or peripheral arterial disease. [8]
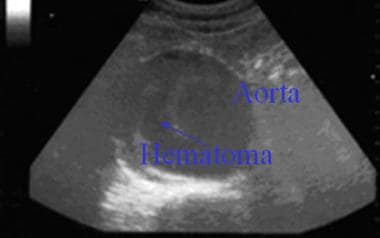
Additionally, in at-risk patients who may present with an unrelated chief complaint, emergency ultrasonography can be a fast and accurate method for identifying patients with AAA who may benefit from follow-up or intervention. [21] The main disadvantage of bedside ultrasonography is that a leaking or ruptured aneurysm can be difficult to distinguish from an enlarged but nonruptured aneurysm. The aorta can also be difficult to visualize when the patient is obese or bowel gas is present. [22]
Gupta et al studied the variability of aortic measurements performed by a non-physician using POCUS versus standard of care (SOC) by a registered vascular technologist or performance of abdominal/pelvic CT. Overall average aortic diameter measurements obtained were 4.1 ± 0.9 cm for POCUS and 4.0 ± 0.9 cm for SOC; the average difference in aortic measurements between POCUS and SOC was -0.1 ± 0.3 cm. [23]
The abdominal aorta is said to have an aneurysm when the distal aorta is dilated to a diameter larger than 3 cm. [24] An AAA typically enlarges at a rate of 2-8 mm/yr. Because enlargement results in an increasing incidence of rupture [25] (eg, a 7-cm AAA has a 19-32% rate of rupture per year) and because the mortality rate is much lower with elective repair than with emergency repair (3-5% vs 50%), the general recommendation is that AAAs larger than 5.0-5.5 cm should be electively repaired. [24, 26]
Indications
Indications for bedside ultrasonography include the following [27] :
-
Suspicion of AAA
-
As a diagnostic aid in the evaluation of patients older than 60 years who present with nonspecific pain in the back, flank, abdomen, or groin
-
For rapid evaluation of an unstable patient in the ED or other acute care patient setting while the surgical team is assembling and resuscitation is ongoing
The U.S. Preventive Services Task Force (USPSTF) recommends the following [28, 29] :
-
One-time screening for AAA with ultrasonography in men aged 65-75 years who have ever smoked.
-
Selective screening for AAA in men aged 65-75 years who have never smoked.
-
Current evidence is insufficient to assess the balance of benefits and harms of screening for AAA in women aged 65-75 years who have ever smoked.
-
Recommendation against routine screening for AAA in women who have never smoked.
Contraindications
Abdominal ultrasonography should not be performed if it would delay definitive care by means of abdominal surgery. A study of rural emergency departments in the province of Quebec found that the most common reason for not using point-of-care ultrasonography was limited access to training programs. [27]
Preparation
Anesthesia
Anesthesia is generally not necessary for sonographic evaluation, because the procedure is not usually painful. The patient should be warned, however, that a considerable amount of pressure is sometimes necessary to obtain quality images. This pressure may be unanticipated and mildly uncomfortable.
Equipment
Equipment includes the following:
-
Ultrasonograph with an abdominal transducer (the standard probe used for this examination is a 3.5- to 5-MHz transducer)
-
Gloves
-
Acoustic gel for application on the patient’s upper abdomen, the transducer, or both
Positioning
The procedure should be done with the patient in the supine recumbent position.
Technique
Overview
Although abdominal ultrasonography in the emergency department (ED) or other acute care patient setting is a good test for suspected abdominal aortic aneurysm (AAA), do not delay operative care to obtain images in an unstable patient.
Explain the procedure, benefits, risks, and complications to the patient and/or the patient’s representative. Ask if he or she would like others to be present for the procedure.
Disrobe the abdomen from xiphoid to pubis. Apply a generous amount of acoustic gel to the patient’s upper abdomen (from xiphoid to umbilicus), the transducer, or both.
Scan the upper abdomen in the transverse plane while holding the probe perpendicular to the patient’s long axis. Identify the aorta and trace it to its bifurcation with the iliac vessels (see the videos below).
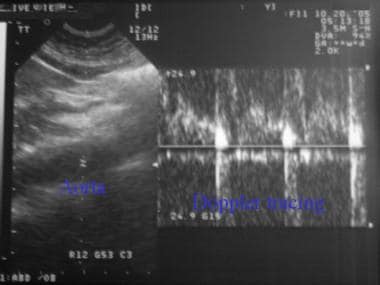
The abdominal aorta can be distinguished from the vena cava (see the image below) by its thicker wall, pulsations, noncompressible nature, and ability to detect pulsatile Doppler flow.
 Transverse view of vertebral body, inferior vena cava (IVC), portal vein, and aorta (clockwise from bottom middle).
Transverse view of vertebral body, inferior vena cava (IVC), portal vein, and aorta (clockwise from bottom middle).
Acquire pictures in the transverse plane, and use the external diameter (outer wall to outer wall) to measure the diameter of the aorta at its widest point (see the image and the video below). An accurate measurement of the aorta’s size is important because the risk of rupture is related to the overall size of the aorta.
Scan the upper abdomen in the longitudinal plane, holding the probe parallel to the long axis of the patient’s body. Acquire pictures in the longitudinal plane, and measure the diameter at the widest point (see the images and video below). Remember that a diameter larger than 3 cm is considered to represent abnormal dilatation.
Once images have been acquired in both transverse and longitudinal planes and the aorta’s diameter has been measured, emergency bedside ultrasonographic imaging for AAA is complete. Wipe the gel from the patient and transducer, cover the patient, and place him or her in a position of comfort.
Visualizing an enlarged (>3 cm) abdominal aorta is diagnostic of AAA, though rupture cannot be definitively diagnosed with ultrasonography alone. The first 2 videos below depict AAA, while the third depicts normal aortic anatomy.
In the appropriate clinical context, ultrasonography alone can rule in the diagnosis of rupture when rupture appears to be present. However, if adequate images cannot be obtained (eg, because of patient obesity or bowel gas), the diagnosis of aortic rupture cannot be excluded.
Common pitfalls in performing bedside ultrasonography to evaluate AAA include the following:
-
Failing to compress the overlying bowel adequately with probe pressure
-
Mistaking the vena cava for the aorta because of transmitted pulsations
-
Overestimating the aneurysmal width because of the lack of a true transverse measurement (cross-section)
-
Confusing an imaging artifact with thrombus
-
Failing to measure the external diameter (outer wall to outer wall)
-
Failing to move the transducer off the sagittal plane while following a tortuous aorta
-
Misinterpreting acoustic enhancement distal to the aorta as evidence of leakage. (Remember that ultrasonography is not good at detecting rupture or leakage. Contrast abdominal computed tomography [CT] is the criterion standard. However, contrast-enhanced ultrasonography may be a reasonable alternative to CT, if CT is unavailable). [30]
-
Being reluctant to move the transducer far laterally in an attempt to visualize an aorta that is obscured by overlying bowel gas
Post-Procedure
Complications
Bedside ultrasonography for evaluation of abdominal aortic aneurysm (AAA) has no major complications, aside from the potential complications that could ensue if immediately available surgical repair is delayed for the purpose of obtaining imaging studies.Limitations include body habitus, bowel gas, and operator experience. In lieu of a limited evaluation of the abdominal aorta, consider advanced imaging based on the patient's hemodynamic status. [8]
Although no data suggest that palpation of an AAA by physical examination or with the probe increases the rate of rupture or worsens an already rupturing AAA, repeated examinations for teaching purposes are not advised.
-
Scanning of upper abdomen from xiphoid to umbilicus in transverse plane to follow abdominal aorta to its iliac bifurcation.
-
Transverse view of vertebral body, inferior vena cava (IVC), portal vein, and aorta (clockwise from bottom middle).
-
Transverse view of 7-cm abdominal aortic aneurysm.
-
Scanning upper abdomen in longitudinal plane to visualize abdominal aorta.
-
Longitudinal view of abdominal aorta (black stripe in middle of image).
-
Using Doppler mode to confirm that visualized structure is aorta (see pulsatile waveforms).
-
Probe starts in transverse plane at level of proximal aorta, where "seagull sign" (bifurcation of celiac trunk) can be appreciated. Probe is then rocked caudally, whereby 3.5-cm abdominal aortic aneurysm is revealed.
-
Aorta is visualized first in short axis and then in long axis. Large (>7 cm) abdominal aortic aneurysm with mural thrombus and hypoechoic areas is appreciated outside aorta, which may represent rupture. Color-flow Doppler illustrates turbulent flow within lumen.
-
Transverse view of 7-cm abdominal aortic aneurysm with echogenic mural thrombus.
-
A demonstration of ultrasonographic aortic evaluation. Video courtesy of Meghan Kelly Herbst, MD, and Department of Emergency Medicine, Yale School of Medicine.
-
Color cine loop depicting abdominal aortic aneurysm (AAA). Video courtesy of Meghan Kelly Herbst, MD, and Department of Emergency Medicine, Yale School of Medicine.
-
Cine loop of abdominal aortic aneurysm (AAA). Video courtesy of Meghan Kelly Herbst, MD, and Department of Emergency Medicine, Yale School of Medicine.
-
Cine loop depicting normal aorta anatomy. Video courtesy of Meghan Kelly Herbst, MD, and Department of Emergency Medicine, Yale School of Medicine.
-
Probe starts in transverse plane at level of proximal aorta, where "seagull sign" (bifurcation of celiac trunk) can be appreciated. Probe is then rocked caudally, whereby 3.5-cm abdominal aortic aneurysm is revealed.