Overview of Osteoarthritis Rehabilitation
Osteoarthritis (OA) is a chronic disease process affecting synovial joints, particularly large weight-bearing joints. OA is particularly common in older patients but can occur in younger patients either through a genetic mechanism or, more commonly, because of previous joint trauma. (See the images below.)
 This radiograph demonstrates osteoarthritis of the right hip, including the finding of sclerosis at the superior aspect of the acetabulum. Frequently, osteoarthritis at the hip is a bilateral finding, but it may occur unilaterally in an individual who has a previous history of hip trauma that was confined to that one side.
This radiograph demonstrates osteoarthritis of the right hip, including the finding of sclerosis at the superior aspect of the acetabulum. Frequently, osteoarthritis at the hip is a bilateral finding, but it may occur unilaterally in an individual who has a previous history of hip trauma that was confined to that one side.
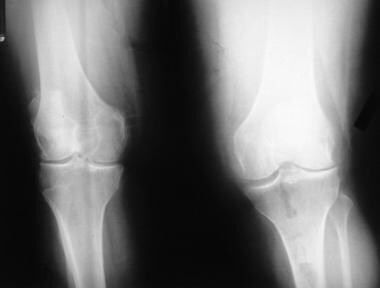 This radiograph demonstrates osteoarthritis of bilateral knees. Radiographic findings of osteoarthritis are often graded using the Kellgren-Lawrence Grading System. These knees would be classified as Kellgren-Lawrence grade 3.
This radiograph demonstrates osteoarthritis of bilateral knees. Radiographic findings of osteoarthritis are often graded using the Kellgren-Lawrence Grading System. These knees would be classified as Kellgren-Lawrence grade 3.
OA rehabilitation is aimed at bringing about pain reduction, function optimization, and the advantageous modification of the joint damage process. [1] To help achieve these goals, the overall rehabilitation strategy for patients with OA can include various components, including the following [2] :
-
Patient education about the disease process, as well as joint-protection and energy-conservation techniques
-
Therapeutic exercise as part of a formal physical therapy program and/or a home exercise program
-
Modalities (eg, heat, cold, electrical stimulation) for home use and/or as part of a physical therapy and/or an occupational therapy program
-
Occupational therapy, with an emphasis on optimizing activities of daily living (ADLs), with or without provision of adaptive equipment
-
Orthotic intervention
-
Medication - Oral and/or topical
-
Intra-articular injections
-
Nerve ablation procedures
-
Surgery
For other discussions on OA, see Osteoarthritis, Wrist Arthritis, Surgical Treatment of Patellofemoral Arthritis, and Glenohumeral Arthritis, as well as Injection of the Acromioclavicular Joint, Total Knee Arthroplasty, Unicompartmental Knee Arthroplasty, Shoulder Arthrocentesis, Surgical Treatment of Interphalangeal Joint Arthritis, Medial Compartment Arthritis, Surgical Treatment of Lateral Compartment Arthritis, Imaging of Osteoarthritis, and Progression of Osteoarthritis.
Therapeutic Exercise for Osteoarthritis
General principles
Lifestyle modification, particularly exercise and weight reduction, is a core component of the management of OA, [3, 4, 5] with the aim of such efforts being provision of pain relief, enhancement of physical function, and improvement of quality of life. Therapeutic exercise programs have been shown to be a successful nonpharmacologic method of achieving these goals. Among the wide range of existing OA exercise programs, stress is placed on various types of exercises; exercise intensity, duration, and supervision; and different types of resistance equipment. [6]
Mechanism of action of therapeutic exercise
The 2017 Ottawa Panel guidelines for the management of knee OA describe the physiologic effects of therapeutic exercise. Resistance exercise, resulting in antinociception via endogenous analgesia, may relieve osteoarthritic pain. [6] A literature review by Runhaar et al indicated that the mechanisms by which exercise reduces pain and improves function in cases of OA may include the development of increased upper leg strength, the reduction of extension impairments, and the improvement of proprioception. The review involved 94 studies, most of which assessed patients with OA only in the knee. [7]
Types of exercise programs
Therapeutic exercise programs can include resistance, functional, or mixed (resistance, balance, coordination) exercises, with muscle-strengthening strategies encompassing the following categories [6] :
-
Concentric - Shortening muscle length via constant tension
-
Eccentric - Lengthening the muscle via constant tension
-
Isometric - Muscle contraction without length change
-
Isokinetic - Change in muscle length at constant speed with constant tension
A systematic review and meta-regression analysis by Juhl et al found that optimal therapeutic exercise programs focus on a single type of exercise, such as aerobic or muscle strengthening (of the quadriceps). The notion that it is preferable to perform either aerobic or resistance exercise, rather than both types, in a single session is related to the molecular response to exercise. The molecular response to resistance training involves an increase in myofibril proteins, whereas in aerobic training, mitochondrial activity is increased. When an individual performs aerobic and resistance exercises within the same session, the molecular response to both appears to decrease. The study also found that for best results in pain reduction, the exercise program should be supervised and consist of three sessions per week. [8]
Resistance training is a major recommendation as part of a nonsurgical treatment option for knee OA. In terms of mechanism of action, it is thought that eccentric resistance training reduces corticospinal inhibition of muscle and that, theoretically, an eccentric program leads to a superior improvement in stair ascent and ambulation, compared with concentric strength training. However, a study by Vincent and Vincent comparing the two types of resistance programs found them to be comparable, though with concentric training being slightly superior in pain reduction while walking. The investigators concluded that eccentric and concentric focused resistance training have both been shown to improve pain and function but that more research is needed to explore the protocols and mechanisms involved in these forms of exercise. [9]
Most research focuses on quadriceps strengthening in knee OA. Also important are stretching exercises, which increase range of motion. The importance of aerobic conditioning, particularly low-impact exercises (if OA affects weight-bearing joints), should be stressed. Swimming, especially aerobic aquatic programs through the Arthritis Foundation, can be helpful. Certain studies also indicate that a home exercise program for patients with OA of the knee provides an important benefit. [7]
A study by Farrokhi et al of patients with unilateral, symptomatic knee OA found that walking exercise of 30 continuous minutes or more may result in undesirable knee joint loading and increased pain, while the same amount of exercise broken into separate intervals with rest periods in between may produce no pain increase. Patients in the study underwent two different exercise sessions, including one continuous 45-minute walk on a treadmill and three 15-minute treadmill walks separated by hour-long rest periods. [10]
In a study of patients with knee OA, Jan et al found that, in most respects, non–weight-bearing exercise was as therapeutically effective as weight-bearing exercise. [11] After an 8-week program, weight-bearing and non–weight-bearing exercise produced equally significant improvements in function, walking speed, and muscle torque. However, patients in the weight-bearing group demonstrated greater improvement in position sense, which may help with complex walking tasks, such as walking on a spongy surface.
A systematic review by Fransen et al found that land-based exercises reduced pain and improved physical function in patients with knee OA. Furthermore, the study determined that there was no difference in outcomes between weight-bearing and non–weight-bearing exercises that targeted the quadriceps. There was also no difference found between quadriceps exercises that were performed eccentrically/concentrically versus those that were performed isometrically. [12]
Chaipinyo and Karoonsupcharoen found no significant difference in the reduction of OA-related knee pain between home-based strength training and home-based balance training. [13] However, more improvement in knee-related quality of life was noted in the strength-training group than in the balance-training group.
Results from a study by Wang et al suggested that tai chi is a potentially effective treatment for pain associated with OA of the knee. [14] In a prospective, single-blind, randomized, controlled trial, 40 patients with symptomatic tibiofemoral OA who performed 60 minutes of tai chi twice weekly for 12 weeks experienced significantly greater pain reduction than did control subjects who underwent 12 weeks of wellness education and stretching. The tai chi cohort also had significantly better Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) physical function scores, patient and physician global visual analog scale scores, chair stand time, Center for Epidemiologic Studies Depression Scale scores, self-efficacy scores, and Short Form 36 physical component summaries.
Another study, a meta-analysis by Chang et al, found that an 8- to 24-week program of tai chi improves quadriceps muscle strength in knee OA, allowing elderly patients to prevent or reduce deterioration and loss of daily function. Furthermore, the study indicated that a program consisting of 10 movements of tai chi is ideal for these patients, since it appears that the geriatric population would be less compliant with the program if more than 10 movements were involved. [15]
However, unlike for knee or hip OA, there is no clear consensus on the benefits of exercise therapy for hand OA in terms of pain reduction and function improvement. A review by Magni et al looking at the potential benefits of resistance training for hand OA found no evidence supporting resistance training for function improvement and reported that there was a clinically insignificant benefit in pain reduction. [16] Another review study of hand OA, by Østerås et al, found only mild benefit in terms of pain reduction and function improvement. Both reports agreed that the lack of consensus on the efficacy of exercise therapy in hand OA is due to the relatively limited amount of research on the subject. [17]
Home exercise programs versus formal physical therapy
There is conflicting evidence with regard to the benefits of supervised versus nonsupervised exercise programs. [18] A randomized, controlled study by Kuru Çolak et al found that in knee OA, supervised exercises were more effective at reducing pain and increasing quadriceps and hamstring strength than were nonsupervised exercises. The report determined that the best therapeutic results were derived from low-intensity exercises, due to the ease with which geriatric patients could perform them, and from performance of the exercises at least three times a week. The study also found that the total program should be composed of at least 12 sessions. The investigators noted that although a previous study acknowledged that both supervised and nonsupervised exercises would reduce pain from knee OA, the degree of pain relief was not assessed. [19]
A systematic review by Brosseau et al reported that in 10 high-quality studies of therapeutic exercise programs with a home-based/nonsupervised component, at least one program goal was reached. In contrast, the same results were found in 19 studies of programs with a clinic-based or supervised-session component. [6]
Exercise compliance
A literature review by Marks and Allegrante indicated that in order to encourage people with OA to adhere to an exercise regimen, “interventions to enhance self-efficacy, social support, and skills in long-term monitoring of progress are necessary." [20]
Occupational Therapy for Osteoarthritis
Occupational therapy for OA aims to improve quality of life by modifying the environment to maximize the function of affected joints. Although there are different ways to accomplishes this, two common methods are the use of assistive devices and joint protection. Assistive devices, such as spoons with a large grip/handle, alleviate joint strain and improve function. Joint protection involves means of reducing the use of and strain on affected joints, such as by cradling objects with two arms rather than holding them with the affected joint/limb.
Two common types of nonspecific assistive devices are prefabricated neoprene splints and custom-made thermoplastic splints. However, although assistive devices may be an effective alternative to other nonpharmacologic treatments with regard to reducing pain and improving quality of life, research is lacking on the effectiveness of splint use. [21] .
Although quality of life may be improved by occupational therapy alone, the use of multiple concurrent therapeutic regimens seem to have a greater impact than does single-modality therapy. [22]
Medication for Osteoarthritis
The American College of Rheumatology (ACR) 2012 pharmacologic guidelines for the treatment of hip and knee OA include the following [23] :
-
Up to 4 g/d of acetaminophen can be administered; this is the preferred initial treatment for patients with OA; cases that are unresponsive to acetaminophen at full dosage can be treated with analgesic-dose nonsteroidal anti-inflammatory drugs (NSAIDs) (topical or oral), nonacetylated salicylates, or intra-articular corticosteroid injections
-
Healthcare providers should avoid using nutritional supplements or topical capsaicin for knee OA
-
Topical NSAIDs should be used instead of oral NSAIDs in patients aged 75 years or older and in patients with stage IV or V chronic kidney disease (CKD)
-
For a patient on low-dose aspirin for cardioprotection/stroke prevention, a nonselective NSAID other than ibuprofen should be chosen and used in combination with a proton-pump inhibitor (PPI); the recommendation to avoid ibuprofen is based on a known pharmacodynamic interaction that may render aspirin less effective when used concurrently with ibuprofen.
-
Patients who fail both nonpharmacologic and pharmacologic measures should be considered for total joint arthroplasty; if the patient is not a candidate, further options include opioid analgesics (strong recommendation) and duloxetine (conditional recommendation)
The following ACR recommendations apply to patients with a history of symptomatic or complicated upper gastrointestinal (GI) bleed:
-
If there have been no instances of GI bleed over the past year, the patient may be treated with an oral cyclooxygenase-2 (COX-2) selective NSAID or with the combination of an oral nonselective NSAID and a PPI
-
If an upper GI bleed has occurred over the past year, the patient should be treated with the combination of a COX-2 selective NSAID and a PPI.
For hand OA, the ACR 2012 guidelines recommend topical or oral NSAIDs, topical capsaicin, and tramadol as options for pharmacotherapy. [23]
In a randomized, controlled study by Petersen et al of patients with knee OA, neither ibuprofen nor glucosamine improved muscle mass gain during a 12-week strength-training program. However, patients on these medications achieved improved maximal muscle strength gain in comparison with patients on placebo treatment, but the benefits were not significant enough to advocate taking NSAIDs or glucosamine. [24]
Disease-modifying therapies that may slow or reverse joint structural destruction in OA are under investigation. Glucosamine and chondroitin sulfate are in current use due to their demonstrated association with chondrocyte anabolism and catabolism [25] . A 2011 review by the Agency for Healthcare Research and Quality found that in knee OA, chondroitin sulfate shows medium-term benefits, but no long-term benefits, either individually (on pain alone) or in combination with glucosamine (on pain and function). [26] Therapies targeting the inflammation processes (ie, interleukin-1β [IL-1β] and tumor necrosis factor-ɑ [TNF-ɑ] inhibitors, granulocyte-macrophage colony-stimulating factor [GM-CSF] antibody) and subchondral bone remodeling (ie, bisphosphonates, calcitonin) are also being investigated. [25]
In a randomized, double-blind, multicenter study, etodolac plus acetaminophen was significantly more effective than etodolac alone for osteoarthritic flare-ups. Measurements of reduced pain intensity, achievement of pain relief, and symptom resolution (eg, decreased morning stiffness, inflammation) showed significantly greater improvement with the combination compared with etodolac by itself. [27]
Intra-Articular Injections
Steroid injections
Intra-articular steroid injections may provide pain relief and have an anti-inflammatory effect on osteoarthritic joints. Such injections are generally believed to result in a clinically and statistically significant reduction in osteoarthritic knee pain, often beginning as soon as a couple of days after injection. The effect may last, on average, anywhere from 4-6 weeks per injection, but this benefit is unlikely to continue beyond that time frame. [28] One randomized, placebo-controlled study confirmed the effectiveness of corticosteroid injection in the treatment of osteoarthritic hip pain, with benefits often lasting up to 3 months. [29]
An extended-release intra-articular therapy option, Zilretta (triamcinolone acetonide), was approved by the US Food and Drug Administration (FDA) in October 2017 to manage osteoarthritic knee pain. Phase 3 trial results published in April 2018 found that Zilretta provided approximately 50% reduction in pain from baseline over weeks 1 through 12, with benefit occurring as late as week 18. Zilretta was also found to improve stiffness and function. The most commonly reported side effects were joint pain, headache, and back pain. [30]
However, there is also some evidence of detrimental effects from corticosteroid injections. For example, in a randomized clinical trial of knee OA patients, those who received intra-articular triamcinolone injections over 2 years, compared with intra-articular saline over the same period of time, had significantly greater cartilage volume loss but no significant difference in knee pain. Such treatment for patients with symptomatic knee OA is not supported by these findings. [31]
Viscosupplementation
Intra-articular injection of sodium hyaluronate (i.e., hyaluronic acid [HA], hyaluronan), also referred to as viscosupplementation, has been available in the United States since 1997. The largest meta-analysis of intra-articular HA injection, involving 76 controlled clinical studies (and subsequently updated by the Cochrane Collaboration), concluded that this therapy is safe and effective in patients with knee OA. [32]
The FDA has approved multiple intra-articular HAs for the treatment of pain associated with knee OA. These include naturally extracted, non–cross-linked products, chemically cross-linked agents, and bacterially fermented viscosupplements. Although some of these agents differ with respect to molecular weight, molecular weight per se has not been found to correlate with efficacy. Interestingly, the duration of residence of an intra-articular injection (days) cannot explain the prolonged clinical benefit (months), and accordingly, biologic mechanisms have been proposed that may play an important role in HA's efficacy.
Generally, the safety profile of the HA class has been shown to be very favorable for osteoarthritic knee pain management. Injection-site pain is the most frequent adverse event. Severe acute inflammatory reaction [SAIR], or HA-associated intra-articular pseudosepsis, is a clinically distinct side effect related to the cross-linked hylan G-F 20 product. An immunologic mechanism of action may be the cause. [33]
In the United States, HAs are classified as medical devices rather than medications. Although the exact mechanisms of action through which they provide symptomatic relief are unknown, several possibilities exist, including direct binding to receptors (CD44 in particular) in the synovium and cartilage that can lead to several biologic activation pathways. Other possible mechanisms of action include the increased endogenous production of hyaluronate and aggrecan by the joint, a mechanical barrier to the activation of nociceptors, the inhibition of pain mediators (eg, prostaglandin E [PGE], bradykinin), an anti-inflammatory effect (eg, inhibition of proinflammatory cytokine activity, inhibition of inflammatory cell function), a beneficial effect on immune cells, an antioxidant effect, and the restoration of the synovial fluid's physical characteristics (viscoelasticity). Viscosity can help to facilitate the cushioning and lubricating characteristics of the joint during slow movements, while elasticity blunts deforming forces (compression and resistance to shear forces) during rapid motions. A study by Waddell and colleagues hypothesized that hyaluronan inhibits IL-1β–induced metalloproteinase production from osteoarthritic synovial tissue. [34]
Intra-articular HAs may possibly be chondroprotective especially in early OA. As reviewed by Goldberg and Buckwalter, preclinical support is available for most of the HAs, as well as clinical evidence (particularly for Hyalgan) using arthroscopy, microscopy, and blinded morphologic assessments and weight-bearing radiographs for assessing joint space narrowing. [35] However, additional studies are warranted to further explore the ability of HAs to intervene in the disease processes associated with OA. Certainly, a single product with symptomatic and disease-modifying characteristics, even if only in some patient populations, would be a valuable option in the management of knee OA.
There is some data on the effectiveness of HA injections with respect to OA severity. Specifically, these injections were found to be most beneficial in earlier grades of knee OA; following infection, 91% and 80% of patients with radiographic grade I and II knee OA, respectively, reported improvement in their condition, as did 76% and 58% of patients with grades III and IV, respectively. HA injections may help to delay the need for total knee arthroplasty (TKA). According to 2015 data published by the Osteoarthritis Research Society International, treatment with HA injections can delay the need for TKA by up to 3.6 years. [36]
Studies have found HA injections to be a cost-effective treatment in comparison with conventional care modalities, such as analgesics, corticosteroids, NSAIDs, assistive devices, and TKA. Moreover, while HA injections have been reported to be as effective as corticosteroid injections in the short-term, evidence indicates that HA injections provide longer duration of pain relief. In addition, owing to the risks of weight gain and hyperglycemia associated with corticosteroids, HA injections may be a better alternative for patients with comorbidities, particularly obesity and diabetes. [36] Quadriceps strengthening combined with HAs may synergistically affect pain. [33]
Ultrasonographically guided HA injections can enhance accuracy and improve patient-reported clinical outcomes and cost-effectiveness. [36]
Platelet-rich plasma (PRP) injections
PRP injections are becoming more commonly performed as a treatment option for patients with OA. PRP, which is derived from the patient’s own blood, delivers a concentration of growth factors to the site of pathology. In a randomized, controlled trial on knee OA patients conducted by Spaková et al, it was found that patients had decreased pain and stiffness and improved physical function at 3 and 6 months after the injection. [37]
A study that compared the efficacy of PRP and HA intra-articular injections for primary knee OA found that although at 3- and 6-month follow-up, all outcome measures improved in association with both treatments, the PRP group achieved significantly better results. Synovial hypertrophy and vascularity scores improved and, in comparison with patients who underwent HA injections, effusion was lower, in patients treated with PRP injections. [38]
By enhancing the expression of NF-kappa-beta inhibitor, resulting in a decrease in nuclear factor-κβ (NF-κβ) signaling and a dampening of its downstream inflammatory cytokine activation, PRP can reduce osteoarthritic joint inflammation. PRP is capable of switching off type II collagen inhibition and aggrecan gene expression in IL-1β–activated NF-κβ in chondrocytes. Thus far, PRP has been mainly employed in the treatment of musculoskeletal conditions, especially tendon-related pathologies. [39, 40]
Biologic injections
Biologics (protein-derived medications from cultured cells) have also been explored in the treatment of OA, especially in patients whose condition was refractory to conventional drugs. In a 12-month pilot study on erosive hand OA, monthly intra-articular injections of infliximab (a monoclonal antibody against TNF-ɑ) into the affected joints was found to cause a reduction in anatomic lesions when compared with joints injected with saline. [41]
An investigation in rats, by Zhu et al, indicated that it may be possible to use platelet-derived growth factor-BB to decrease apoptosis and thereby reduce chondrocyte loss and increase type II collagen. Although the study was limited in scope by focusing only on caspase 3–induced apoptosis of chondrocytes, it did show that lowering the rate of cartilage remodeling and loss of chondrocytes could decrease disease progression, via this specific mechanism. [42]
Stem cell therapies
A therapeutic case series study published in 2015 found that adipose stem/stromal cell (ASC) and stromal vascular fraction (SVF) procedures improved symptom‐related, functional, radiographic, and histologic scores in patients with OA. Patients recruited into the study were usually refractory to oral medications, physical therapy, autologous cartilage transplantation, and HA injection. Patient questionnaires indicated that administration of SVF or ASCs into affected joints led to improvements in pain, function, mobility, and overall quality of life. Evidence for the effectiveness of SVF or ASC administration also emerged from evaluation with magnetic resonance imaging (MRI) and arthroscopy, with improvement or maintenance of cartilage status found. Patients in these studies experienced clinical improvement over a period of between several months and more than 2 years. [43]
Preclinical studies indicate that ASCs exercise their effects via an ASC-mediated decrease in pro‐inflammatory cytokines and chemokines, apoptosis of chondrocytes, hypertrophic and fibrotic chondrocyte phenotypes, and collagenases. Multiple phase-1 clinical trials have indicated that SVF-cell and ASC administration is safe. As evidenced in six studies (130 patients), joint pain is the most frequent adverse event. Neither liposuction nor intra-articular injection of stem cells was associated with adverse events. These results suggest that in patients with severe, treatment-refractory OA, especially that involving the knee, SVF cells and ASC are therapeutic candidates. [43]
Other Treatments
Orthoses
Although orthotic devices are widely used for OA, there is limited supporting evidence that such devices are beneficial.
Footwear interventions, such as cushioning, appear to reduce pain and increase function, and reduce plantar pressure in people with first metatarsophalangeal (MTP) OA. [44] A 12-month study of 200 people aged 50 years or older with medial knee OA found no symptomatic or structural differences between patients who wore lateral wedge insoles and those who wore flat control insoles, inside their footwear [45] .
Since 2015, a device known as the Unloader Hip brace has been available in the United States for use in patients with symptomatic hip OA. This brace was derived in part from the WISH-type modified S-form hip brace from Japan. The current Unloader Hip brace likely exerts its overall effect via several mechanisms, with the brace featuring a trochanteric pad that provides direct compression, thus helping with proprioceptive support of the hip joint, and a dynamic rotation strap that shifts compressive forces away from the main osteoarthritic region in the superior-lateral corner of the joint (via external rotation and abduction). The overall brace also improves joint stability. Supporting evidence for the Unloader Hip brace's efficacy includes a gait analysis study of 14 subjects with unilateral hip OA. The report found that use of the brace led to a significant reduction in peak internal hip abduction force (the major factor indicative of hip joint loading during the single support phase of gait) and a significant decrease in ambulation pain. [46]
A review study that included six randomized, controlled trials and five nonrandomized, controlled trials concluded that soft braces appear to provide moderate pain relief and improve functionality in knee OA, which may play an important role in short-term and long-term OA management. [47]
Kinesio Taping (KT) involves strategic placement of waterproof, hypoallergenic elastic tape on the affected joint. KT is believed to provide a therapeutic effect through reduction of pain and edema, as well as through mechanical correction and support. A randomized, clinical study by Donec and Kubilius showed that KT of OA-affected knees led to significant knee pain reduction, along with a decrease in NSAID usage. Furthermore, the report found that utilizing KT led to statistically and clinically significant improvements in knee pain when compared with nonspecific taping methods. The study's results suggested that KT can be an effective adjunct to other rehabilitation interventions for knee OA. [48]
However, although many clinical trials involving orthotic interventions have been performed, there has not yet been enough high-quality research to provide strong evidence for the benefit of orthotic devices. [49]
Nonetheless, people with OA may receive limited benefit from use of orthotic devices. Patients and physicians should discuss risks and benefits on individual basis to provide optimal outcome.
Acupuncture
Acupuncture is becoming a more frequently utilized option in treating pain and physical dysfunction associated with OA. There appears to be a subjective benefit from acupuncture for the treatment for osteoarthritic pain, but no conclusive evidence can be drawn due to an insufficient amount of supporting evidence. [50, 51]
Massage therapy
Massage therapy is another alternative to improve symptoms of OA. Some research into the effects of massage therapy has shown positive results, with, for example, patients in a randomized, controlled trial of 125 adults with knee OA reporting improvements in pain and function in conjunction with 8 weeks of massage therapy. [52]
Moreover, in small-group studies performed in 2014 and 2017, patients reported increased activities of daily living after massage therapy. [53, 54]
Currently, however, not enough data are available to conclusively support massage therapy as having clinically significant therapeutic value in OA. Further research and study are required to determine its benefit.
Transcutaneous electrical nerve stimulation (TENS)
TENS may be another treatment option for pain relief. To date, however, there are conflicting study results regarding its efficacy.
Some studies support the use of TENS. Analysis of 3-month use of TENS in 23 people with OA of the knee found a reduction in the Visual Analog Scale score, implying subjective reduction of pain and improvement in function and quality of life. [55] One randomized controlled trial looked at the effects of TENS with home exercise in 60 patients with Kellgren-Lawrence grade 3 or 4 knee OA. Analysis at the 10-week and 6-month mark showed subjective improvement in pain and function. [56] (See the images below.) Another study evaluated the use of TENS with and without heat and cold packs on knee OA, with patients reporting subjective immediate pain relief, as well improvement in ambulation, gait, and balance; however, the long-term effects were unclear. [57]
There are also studies indicating that TENS is not effective. Patients referred for physiotherapy for knee OA involved in a randomized, sham-controlled clinical trial by Palmer et al reported no significant improvement after use of TENS. [58] Another study, which examined the use of TENS after TKA, concluded that no significant difference existed between TENS and non-TENS patients with regard to postsurgical opioid usage and other endpoints. [59]
The conflicting results from these studies suggest the needs for larger and higher-quality randomized, controlled trials.
Pulsed electromagnetic field (PEMF) stimulation
A PEMF-stimulation device (Bionicare) has been FDA-approved for use in patients with knee OA. PEMF stimulation is believed to act at the level of hyaline cartilage by maintaining proteoglycan composition of chondrocytes via down-regulation of composition turnover. [60] PEMF stimulation has also been shown to induce an anti-inflammatory mechanism through gene expression on the cellular and tissue levels.
A multicenter, double-blind, randomized, placebo-controlled, 4-week trial in 78 patients with knee OA found improved pain and function in patients who were treated with the PEMF-stimulation device. [61] Another, small study, of patients with cervical OA, found that the PEMF-stimulation group showed improvement in active range of motion and paravertebral muscle spasm and in the Neck Pain and Disability Scale, compared with the sham group. [62] (See the image below.)
However, other research has found a lack of evidence to support the use of PEMF stimulation. A literature review identified five randomized, controlled trials from between 1966 and 2005 on the use of PEMF stimulation. The analysis revealed no clear evidence that the modality provides significant pain relief in knee OA. [63] A clinical trial involving 459 osteoarthritic subjects reported that although PEMF stimulation did not reduce pain, it did improve function. [64]
Consequently, while PEMF stimulation may provide some pain relief to people with OA, it is still unclear whether it provides any therapeutic value. This option may be considered after unsuccessful results from other conventional and alternative treatment methods.
Genicular nerve radiofrequency ablation
The progressive nature of knee OA makes it difficult to achieve long-lasting pain relief with conservative management. Genicular nerve radiofrequency ablation (GNRFA) is an alternative to surgical intervention and in some cases is an adjunct to surgery in those patients who have persistent pain despite arthroplasty. GNRFA works outside the knee joint proper to ablate the nerves carrying pain signals and can provide analgesia for up to a year. Pain can and often does recur, due to axonal regeneration, but the procedure can be repeated indefinitely. [65]
Surgical Intervention
Surgical intervention for OA may be indicated. Types of procedures vary according to the site and the degree of involvement.
Surgical interventions for OA of the knee include the following:
-
Arthroscopic lavage - Using a saline lavage to wash out the joint
-
Joint realignment (realignment osteotomy) [66]
-
Joint fusion (arthrodesis) - Surgically fusing the joint to eliminate motion
-
Joint replacement (arthroplasty): TKA or unicompartmental arthroplasty
Surgical interventions for OA of the hip include the following:
-
Joint realignment (realignment osteotomy)
-
Joint fusion (arthrodesis) - Surgically fusing the joint to eliminate motion
-
Joint replacement (arthroplasty)
For the knee, unicompartmental arthroplasty can serve as an alternative to TKA, particularly when the OA is primarily unicompartmental. Improved surgical techniques and implants have led to more frequent use of this option, with recovery from the operation tending to be faster and the resulting range of motion better than those associated with TKA. [67]
Hip replacements generally are classified as either hemiarthroplasty (ie, replacement of the femoral side of the hip joint, while leaving the patient's acetabulum intact) or total hip arthroplasty (replacement of the femoral side of the hip joint and the acetabulum).
Further classification often involves specification of the hardware used (eg, unipolar prosthesis, bipolar prosthesis) and whether or not cement is used to hold the hardware in place.
The prognosis is good for patients with OA who have undergone joint replacement. According to a meta-analysis by Vissers et al, patients who undergo hip replacement can return to as much as 80% of normal daily activity around 6 months after surgery. [68] The prosthesis may need revision 10-15 years after its installation, depending on the patient's activity level.
Consultations
Consultation with an orthopedic surgeon may sometimes be needed. Rheumatology consultation is indicated if an alternative diagnosis (eg, rheumatoid arthritis) is suggested.
Deterrence and Prevention
The overall topic of OA prevention is lacking in significant research evidence. The following factors have been examined to different degrees.
Body mass index (BMI)
The relationship of BMI to OA has been explored in some detail. For example, it is believed that maintaining ideal body weight lessens the probability of developing OA. This appears to be particularly true for weight-bearing joints (ie, hips, knees) in women. A cross-sectional, retrospective analysis concluded that individuals with a higher risk for worse knee OA symptoms include women and persons with a higher BMI. [69] According to Messier et al, even a 10% weight loss in overweight and obese patients could improve knee OA by decreasing weight loads during walking. [70]
Therapeutic exercise
Although various studies have found that physical activity improves function in adults with arthritis, it is unclear if this translates into a decreased likelihood of OA development and progression. [71]
Vitamin supplementation
It was formerly believed that adequate vitamin D intake can lessen the risk of developing OA. However, a 2018 study by Cakar et al found no statistically significant association between serum vitamin D concentrations and osteoarthritic knee pain. [72] Nonetheless, additional studies are needed to conclusively determine the role of vitamin D in OA pathophysiology and pain perceptions. In contrast to the lack of association of vitamin D levels with knee OA pain, limited evidence suggests that in patients with late-stage knee OA, improvement in clinical symptoms and a decrease in oxidative stress conditions can be achieved via vitamin E's antioxidant properties. [73]
Surgical intervention
Meniscus-preserving techniques rather than partial meniscectomy can in the long-term help to prevent the development of knee OA. [74]
Patient Education
As the prevalence of OA increases, more patients are dealing with chronic osteoarthritic pain. A systematic review by Ali et al showed that patient education and psychosocial support play a critical role improving outcomes of patients with OA and their adherence to treatment. [75] Patient education is one of the primary therapeutic approaches to OA. [76] Several Arthritis Foundation studies have demonstrated that education in OA benefits the patient. Through education, patients can institute ways to reduce pain and increase joint function. It is important for the clinician to emphasize the need for physician follow-up visits.
For patient education information, see the Arthritis Center and Osteoarthritis, as well as the Arthritis Foundation.
-
This radiograph demonstrates osteoarthritis of the right hip, including the finding of sclerosis at the superior aspect of the acetabulum. Frequently, osteoarthritis at the hip is a bilateral finding, but it may occur unilaterally in an individual who has a previous history of hip trauma that was confined to that one side.
-
This radiograph shows a knee without significant osteoarthritis (for comparison with radiographs demonstrating osteoarthritis).
-
This radiograph (lateral view) demonstrates a knee without significant osteoarthritis (for comparison with osteoarthritis radiographs).
-
This radiograph demonstrates osteoarthritis of bilateral knees. Radiographic findings of osteoarthritis are often graded using the Kellgren-Lawrence Grading System. These knees would be classified as Kellgren-Lawrence grade 3.
-
Osteoarthritis of the knee, Kellgren-Lawrence grade 3.
-
Osteoarthritis of the knee, Kellgren-Lawrence grade 3.
-
Osteoarthritis of the bilateral knees, Kellgren-Lawrence grade 2.
-
Osteoarthritis of the right knee, Kellgren-Lawrence grade 2.
-
Osteoarthritis of the left knee, Kellgren-Lawrence grade 2.
-
This radiograph demonstrates osteoarthritis of the cervical spine. Note the bridging osteophytes between the spinous processes, as well as the significant degree of degenerative disk disease.
-
This radiograph demonstrates osteoarthritis of the cervical spine. Note the bridging osteophytes seen between the spinous processes.
-
Osteoarthritis of the cervical spine, anteroposterior view.
-
Osteoarthritis of the elbow is not commonly seen; however, it can occur with a history of previous trauma.
-
Osteoarthritis of the elbow is not commonly seen; however, it can occur with a history of previous trauma.
-
Osteoarthritis of the elbow is not commonly seen; however, it can occur with a history of previous trauma.
Tables
What would you like to print?
- Overview of Osteoarthritis Rehabilitation
- Therapeutic Exercise for Osteoarthritis
- Occupational Therapy for Osteoarthritis
- Medication for Osteoarthritis
- Intra-Articular Injections
- Other Treatments
- Surgical Intervention
- Consultations
- Deterrence and Prevention
- Patient Education
- Show All
- Media Gallery
- References












