Practice Essentials
Acute poliomyelitis is a disease of the anterior horn motor neurons of the spinal cord and brain stem caused by poliovirus. Flaccid asymmetrical weakness and muscle atrophy are the hallmarks of its clinical manifestations, due to loss of motor neurons and denervation of their associated skeletal muscles. Because of the success of poliovirus vaccine, poliomyelitis, once one of the most feared human infectious diseases, is now almost entirely preventable by proper immunization (see image below).
In 1988, the World Health Organization (WHO) began the Global Polio Eradication Initiative to eradicate poliomyelitis; at the time, it was endemic in 125 countries. By 2016, only three countries, Pakistan, Afghanistan, and Nigeria, were endemic for polio, [1] and with no evidence of wild poliovirus type I transmission in Nigeria after September 2016, the disease is now endemic only in Pakistan and Afghanistan. [2] However, the campaign to eradicate polio continues, as do efforts to prevent transmission of the disease into polio-free areas. [3, 4, 5, 6, 7]
Signs and symptoms of acute poliomyelitis
Paralytic poliomyelitis is characterized by the following:
-
Severe muscle pain and spasms, followed by weakness, develop; muscle weakness tends to become maximal within 48 hours but may develop for longer than a week; no progression of weakness should be noted after the temperature drops to normal for 48 hours; weakness is asymmetrical, with the lower limbs affected more than upper limbs
-
Muscle tone is flaccid, and the reflexes initially are brisk but then become absent; transient or occasionally persistent, coarse fasciculations also are observed frequently in patients with paralytic poliomyelitis
-
Patients also complain of paresthesias in the affected limbs without real sensation loss
-
Paralysis remains for days or weeks before slow recovery occurs over months or years; which factors favor development of paralytic disease remains unclear, but some evidence exists that physical activity and intramuscular injections during the prodrome may be important exacerbating factors [8]
Workup of acute poliomyelitis
Lab tests in the workup of acute poliomyelitis include a lumbar puncture test; a complete blood count (CBC); virus recovery via throat washing, stool culture, blood culture, and cerebrospinal fluid (CSF) culture; and a polymerase chain reaction (PCR) assay (to differentiate wild-type strains from vaccine strains).
With regard to imaging studies, magnetic resonance imaging (MRI) may show localization of inflammation to the spinal cord anterior horns.
In electromyographic evaluation, the earliest finding is a reduction in the recruitment pattern and a diminished interference pattern due to acute motor axon fiber involvement. Fibrillations develop in 2-4 weeks and persist indefinitely; fasciculations also may be observed.
Under microscopy, the spinal anterior horn cells are surrounded by inflammatory cells. Spongiosis of the gray matter, containing many scattered inflammatory cells, also is noted. Most inflammatory cells are neutrophil leukocytes.
Management
All patients should be placed on bedrest in an isolation unit. Monitor patients' vital signs carefully; focus especially on the swallowing function, vital capacity, pulse, and blood pressure, in anticipation of respiratory or circulatory complications.
Physical therapy plays an important role in rehabilitation for patients with poliomyelitis. Patients with muscle paralysis benefit from frequent passive range of motion (PROM) and splinting of joints to prevent contracture and joint ankylosis. Chest physical therapy (CPT) helps patients with bulbar involvement prevent any pulmonary complications, such as atelectasis. Frequent repositioning of paralyzed patients helps to prevent bedsores. Occupational, speech, and recreational therapy also can be beneficial.
In severe cases of contracture from limb immobilization, the patient may benefit from orthopedic surgery to release the contracture and restore limb function.
Pathophysiology
Acute poliomyelitis is caused by small ribonucleic acid (RNA) viruses of the enterovirus group of the picornavirus family. The single-stranded RNA core is surrounded by a protein capsid without a lipid envelope, which makes poliovirus resistant to lipid solvents and stable at low pH. Three antigenically distinct strains are known, with type I accounting for 85% of cases of paralytic illnesses. Infection with one type does not protect from the other types; however, immunity to each of the 3 strains is lifelong.
The enteroviruses of poliomyelitis infect the human intestinal tract mainly through the fecal-oral route (hand to mouth). The viruses multiply in oropharyngeal and lower gastrointestinal tract mucosa during the first 1-3 weeks of the incubation period. Virus may be secreted in saliva and feces during this period, causing most host-to-host transmission. After the initial alimentary phase, the virus drains into the cervical and mesenteric lymph nodes and then into the blood stream. Only 5% of infected patients have selective nervous system involvement after viremia. It is believed that replication in extraneural sites maintains the viremia and increases the likelihood that the virus will enter the nervous system.
The poliovirus enters the nervous system by either crossing the blood-brain barrier or by axonal transportation from a peripheral nerve. It can cause nervous system infection by involving the precentral gyrus, thalamus, hypothalamus, motor nuclei of the brainstem and surrounding reticular formation, vestibular and cerebellar nuclei, and neurons of the anterior and intermediate columns of the spinal cord. The nerve cells undergo central chromatolysis along with an inflammatory reaction while multiplication of the virus precedes onset of paralysis. As the chromatolysis process goes on further, muscle paralysis or even atrophy appears when fewer than 10% of neurons survive in the corresponding cord segments. Gliosis develops when the inflammatory infiltrate has subsided, but most surviving neurons show full recovery. [8, 9]
Epidemiology
Frequency
United States
Because of widespread use of the poliovirus vaccine, the incidence rate has been less than 0.01 cases per 100,000 population since 1965. The last case of wild-type polio in the United States was in 1979. Rare cases have been reported of poliomyelitis resulting from live attenuated poliovirus vaccine, with the disease having been brought into the United States via people who have traveled to countries where polio is endemic or where an outbreak is occurring. These vaccine-derived poliovirus infections were last reported in the United States in 2005. They have been seen primarily in low-vaccination communities and isolated religious sects, with the latter often choosing not to participate in government-sponsored public health services, such as immunizations for infectious diseases. [10, 11]
International
Acute poliomyelitis has had a worldwide distribution, with a peak season from July to September and a concentration in tropical areas of the Northern Hemisphere. The condition continues to occur epidemically in nonimmunized populations in developing regions. Poor sanitation and crowded circumstances are two additional factors associated with dissemination. Internationally, importation of polio continues to occur into polio-free countries. From 2002-2005, 21 previously polio-free countries experienced a resurgence of wild-type polio. [12] In eight of those countries, the cases were limited and no further spread was observed. In the remaining 13 countries, multiple cases were observed, with the outbreak lasting less than 6 months. [13, 14] In October 2013, Syria reported that, after having been eradicated there 15 years earlier, polio had returned to that country, with 13 cases from the Deir Al Zour province, caused by wild poliovirus type I, having been confirmed. [15]
As of 2018, wild-type polio remained endemic in Pakistan and Afghanistan; by late April, cases for 2018 numbered one in Pakistan and seven in Afghanistan. In 2016, it was discovered that wild poliovirus transmission was also endemic in Nigeria, although the virus was not detected there in 2017 or, as of a May report by the Centers for Disease Control and Prevention (CDC), in 2018. (However, the CDC report stated that because of access limitations for poliovirus surveillance in insurgent-held areas of Nigeria, the virus could have continued to be transmitted in that country undetected.) [1]
Mortality/Morbidity
Of acute poliovirus infections, 4-8% show only nonspecific illness, and 1-2% of infections finally result in neurologic symptoms. The incidence of paralytic diseases increases with young age, advanced age, recent hard exercise, tonsillectomy, pregnancy, and impairment of B-lymphocyte defenses. The mortality from acute paralytic poliomyelitis is 5-10%, but it can reach 20-60% in cases of bulbar involvement.
Race
Acute poliomyelitis has no racial predilection.
Sex
The male-to-female ratio for acute poliomyelitis is 1:1.
Age
Most cases of acute poliomyelitis occur in the pediatric population. Infection or immunization against poliovirus provides lifelong protection.
-
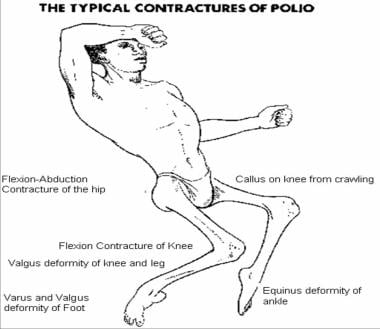
The typical contractures of postpolio residual paralysis.
-
Orthotic treatment for deformities around the knee in poliomyelitis.
-
Surgical correction of a fixed flexion deformity of the knee and hip due to iliotibial band contracture, by Souttar and Yount's release.