Practice Essentials
Pain attributed to muscle and its surrounding fascia is termed myofascial pain, with cervical myofascial pain thought to occur following either overuse of or trauma to the muscles that support the shoulders and neck. It can also result from compensation for an underlying spinal problem such as facet joint arthropathy or an annular tear in one of the discs. In the cervical spine, the muscles most often implicated in myofascial pain are the trapezius, levator scapulae, rhomboids, supraspinatus, and infraspinatus. [1, 2] (See Etiology.) Treatments for cervical myofascial pain include physical therapy, trigger point injection, stretch-and-spray therapy, and ischemic compression. [3]
Myofascial pain in any location is characterized on examination by the presence of trigger points located in skeletal muscle. A trigger point is defined as a hyperirritable area located in a palpable, taut band of muscle fibers (see the image below). (See Etiology, Presentation, and Treatment.)
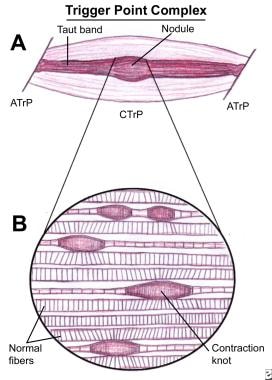 Schematic of a trigger point complex of a muscle in longitudinal section. A: The central trigger point (CTrP) in the endplate zone contains numerous electrically active loci and numerous contraction knots. A taut band of muscle fibers extends from the trigger point to the attachment at each end of the involved fibers. The sustained tension that the taut band exerts on the attachment tissues can induce a localized enthesopathy that is identified as an attachment trigger point (ATrP). B: Enlarged view of part of the CTrP shows the distribution of 5 contraction knots. The vertical lines in each muscle fiber identify the relative spacing of its striations. The space between 2 striations corresponds to the length of 1 sarcomere. The sarcomeres within one of these enlarged segments (ie, contraction knot) of a muscle fiber are markedly shorter and wider than the sarcomeres in the neighboring normal muscle fibers, which are free of contraction knots.
Schematic of a trigger point complex of a muscle in longitudinal section. A: The central trigger point (CTrP) in the endplate zone contains numerous electrically active loci and numerous contraction knots. A taut band of muscle fibers extends from the trigger point to the attachment at each end of the involved fibers. The sustained tension that the taut band exerts on the attachment tissues can induce a localized enthesopathy that is identified as an attachment trigger point (ATrP). B: Enlarged view of part of the CTrP shows the distribution of 5 contraction knots. The vertical lines in each muscle fiber identify the relative spacing of its striations. The space between 2 striations corresponds to the length of 1 sarcomere. The sarcomeres within one of these enlarged segments (ie, contraction knot) of a muscle fiber are markedly shorter and wider than the sarcomeres in the neighboring normal muscle fibers, which are free of contraction knots.
Descriptions of myofascial pain date back to the mid-19th century, when Froriep described muskelschwiele, or muscle calluses. He characterized these calluses as tender areas in muscle that felt like a cord or band associated with rheumatic complaints. In the early 1900s, Gowers first used the term fibrositis to describe muscular rheumatism associated with local tenderness and regions of palpable hardness.
In 1938, Kellgren described areas of referred pain associated with tender points in muscle. In the 1940s, Janet Travell, MD, began writing about myofascial trigger points. Her text, written in conjunction with David Simons, MD, continues to be viewed as the foundational literature on the subject of myofascial pain. [4]
The primary concern for patients with cervical myofascial pain is chronicity. Recurrence of myofascial pain is a common scenario. Prompt treatment prevents other muscles in the functional unit from compensating and, consequently, producing a more widespread and chronic problem. Migraine headaches and muscle contraction headaches are known to occur frequently in the patient with myofascial pain. [5] Temporomandibular joint (TMJ) syndrome also may be myofascial in origin. (See Prognosis, Presentation, Treatment, and Medication.) [1]
Symptoms of cervical myofascial pain
These include the following:
-
Cervical spine range of motion (ROM) is often limited and painful
-
The patient may describe a lumpiness or painful bump in the trapezius or cervical paraspinal muscles
-
Massage is often helpful, as is superficial heat
-
The patient's sleep may be interrupted because of pain
-
The cervical rotation required for driving is difficult to achieve
-
The patient may describe pain radiating into the upper extremities, accompanied by numbness and tingling, making discrimination from radiculopathy or peripheral nerve impingement difficult
-
Dizziness or nausea may be a part of the symptomatology
-
The patient experiences typical patterns of radiating pain referred from trigger points
Workup in cervical myofascial pain
The diagnosis of myofascial pain is clinical, with no confirmatory laboratory tests available. Magnetic resonance imaging (MRI) may be helpful in ruling out any significant abnormality within the structure of the cervical vertebrae or spinal canal. The cervical discs also may be evaluated. If the pain is in the shoulders or chest wall, be aware that visceral pain may refer to these areas and even produce some myofascial findings on examination. Be open-minded to the possibility that another problem also may be present.
It may also be reasonable, depending on the clinical presentation, to check for indicators of inflammation, assess thyroid function, and perform a basic metabolic panel to rule out a concomitant medical illness.
Management of cervical myofascial pain
The primary goal of physical therapy is to restore balance between muscles working as a functional unit. The physical therapist may progress toward that goal initially by attempting to diminish pain. This goal can be accomplished using a modality-based approach performed in conjunction with myofascial release techniques and massage. Cervical stretch and stabilization are integral parts of the approach as well. Postural retraining is crucial in cervical myofascial pain. An ergonomic evaluation may be indicated if overuse in the work setting is contributing to the patient's symptoms.
Trigger point injection probably is one of the most accepted means of treating myofascial pain besides physical therapy and exercise. Injection is performed most commonly with local anesthetic, although dry needling has been shown to be equally effective. [6]
Stretch and spray is another method of treating cervical myofascial pain. This technique is performed using a vapocoolant spray applied to the affected muscle after it has been placed in passive stretch.
Ischemic compression involves application of sustained pressure on the trigger point. Have the patient place the muscle in a fully stretched position. Press firmly on the trigger point with a thumb. Gradually increase the pressure as the pain lessens.
Botulinum toxin (BoNT) injection therapy has received mixed reviews in the literature. Injection directly into the trigger point produces inconsistent results. The best use of BoNT may be for correcting abnormal biomechanics that incite a myofascial response. [7, 8]
Etiology
Cervical myofascial pain is thought to occur following either overuse of or trauma to the muscles that support the shoulders and neck. It can also occur as a reaction to an underlying spinal pathology such as facet joint arthropathy or an annular tear in one of the cervical discs. Common scenarios among patients are recent involvement in a motor vehicle accident or performance of repetitive upper extremity activities.
In the cervical spine, the muscles most often implicated in myofascial pain are the trapezius, levator scapulae, rhomboids, supraspinatus, and infraspinatus. [1] Trapezial myofascial pain commonly occurs when a person with a desk job does not have appropriate armrests or must type on a keyboard that is too high.
Other issues that may play a role in the clinical picture of cervical myofascial pain include endocrine dysfunction, chronic infections, nutritional deficiencies, poor posture, and psychological stress.
Epidemiology
Occurrence in the United States
Myofascial pain is thought to occur commonly in the general population. As many as 21% of patients seen in general orthopedic clinics have myofascial pain. Of patients seen at specialty pain management centers, 85-93% have a myofascial pain component to their condition.
International occurrence
A South American study, by Munoz-Ceron et al, reported that of emergency department patients with nontraumatic headaches, cervical myofascial pain was the most frequent nonprimary cause. [9]
Sex- and age-related demographics
Cervical myofascial pain occurs in both sexes, but with a predominance among women. Myofascial pain seems to occur more frequently with increasing age until midlife. The incidence declines gradually after middle age.
Prognosis
When the patient with cervical myofascial pain undergoes appropriate treatment (eg, physical therapy, massage therapy, stretch and spray, trigger point injections, identification and elimination of an underlying, triggering pathology), the prognosis is generally good. However, recurrence can be a common scenario. Outcomes seem to be better when treatment is initiated early in order to prevent compensation patterns that exacerbate pain. Increased mortality is not associated with cervical myofascial pain.
A Turkish study found evidence that patient disability in chronic myofascial pain is most strongly linked to the duration of pain. The report's assessment was based on data collected from 103 female patients with the chronic disorder and from 30 healthy female participants, using the Neck Pain and Disability Scale, the Beck Depression Inventory, and a visual analog scale, as well as pain pressure threshold measurements from common cervical myofascial pain trigger points. [1]
Patient Education
Patients with cervical myofascial pain need to be educated regarding the factors or underlying problems that may contribute to their pain and loss of mobility. The physical therapist can educate the patient on proper exercise habits and instruct them in a home exercise program for stretching and reconditioning. The patient also may benefit from specific exercises and strategies to improve posture awareness and body mechanics with activities of daily living. If poor workplace ergonomics contribute to the patient's condition, offer instruction in proper ways to modify and revamp the workstation. Cervical myofascial pain is a treatable condition if the patient is educated on the condition and takes an active role in the recovery process.
For patient education information, see Temporomandibular Joint (TMJ) Syndrome, Fibromyalgia, and Chronic Pain.
-
Schematic of a trigger point complex of a muscle in longitudinal section. A: The central trigger point (CTrP) in the endplate zone contains numerous electrically active loci and numerous contraction knots. A taut band of muscle fibers extends from the trigger point to the attachment at each end of the involved fibers. The sustained tension that the taut band exerts on the attachment tissues can induce a localized enthesopathy that is identified as an attachment trigger point (ATrP). B: Enlarged view of part of the CTrP shows the distribution of 5 contraction knots. The vertical lines in each muscle fiber identify the relative spacing of its striations. The space between 2 striations corresponds to the length of 1 sarcomere. The sarcomeres within one of these enlarged segments (ie, contraction knot) of a muscle fiber are markedly shorter and wider than the sarcomeres in the neighboring normal muscle fibers, which are free of contraction knots.
-
Cross-sectional drawing shows flat palpation of a taut band and its trigger point. Left: A. The skin is pushed to one side to begin palpation. B. The fingertip slides across muscle fibers to feel the cord-line texture of the taut band rolling beneath it. C. The skin is pushed to the other side at completion of the movement. This same movement performed vigorously is called snapping palpation. Right: A. Muscle fibers are surrounded by the thumb and fingers in a pincer grip. B. The hardness of the taut band is felt clearly as it is rolled between the digits. C. The palpable edge of the taut band is sharply defined as it escapes from between the fingertips, often with a local twitch response.
-
Longitudinal schematic drawing of taut bands, myofascial trigger points, and a local twitch response. A: Palpation of a taut band (straight lines) among normally slack, relaxed muscle fibers (wavy lines). B: Rolling the band quickly under the fingertip (snapping palpation) at the trigger point often produces a local twitch response, which usually is seen most clearly as skin movement between the trigger point and the attachment of the muscle fibers.
-
Cross-sectional schematic drawing shows flat palpation to localize and hold the trigger point for injection. A and B show the use of alternate pressure between 2 fingers to confirm the location of the palpable module of the trigger point. C shows the trigger point being positioned halfway between the fingertips to keep it from sliding to one side during the injection.
-
Sequence of steps to use when stretching and spraying any muscle for myofascial trigger points.
-
Schematic drawing showing how the jet stream of vapocoolant is applied.







