Practice Essentials
Coccyx pain (tailbone pain) can frustrate patients and significantly impair quality of life, but relief is possible. [1] (See Treatment and Medication.)
Coccyx pain was first documented in 1588, and the term coccygodynia was coined by Simpson in 1859. [2] Currently, the term coccydynia is used somewhat more commonly than coccygodynia. The 2 terms are interchangeable, however, and indicate pain localized to the coccyx. Neither term specifies the underlying etiology. Coccyx pain can occur from local trauma or a tumor, but many cases are idiopathic, with no identifiable cause. (See Etiology.) [3, 4]
Patients with coccyx pain often report that their physicians minimize, dismiss, or belittle their symptoms. [3] Indeed, many physicians may have a bias against patients with coccyx pain, which has been referred to as the “lowest” form of “low back pain.” [5] Tailbone pain is often relatively severe and persistent, causing significant compromise of the patient's ability to perform or endure various activities. Physicians who understand coccydynia and the available treatment options can provide a great service to this otherwise neglected patient population. (See Presentation, Workup, Treatment, and Medication.)
Diagnosis of coccyx pain
The patient's response to injection of local anesthetic agents, with or without corticosteroids, can provide helpful information regarding whether the patient's pain generator has been accurately identified. However, the injection response may not be considered truly diagnostic of whether the pain generator is a specific anatomic structure unless the injection is performed with the guidance of fluoroscopy or other imaging aids. Similarly, if large volumes of fluid are injected, extravasation from the targeted site decreases the diagnostic specificity.
Plain radiographs are typically the initial imaging study of choice for patients with coccydynia, especially in cases of focal sacrococcygeal trauma. Plain radiographs may reveal fractures, abnormal sacrococcygeal curvature, osteophytes, or dislocations of the sacrococcygeal junction or intracoccygeal segments. [6, 7]
Lumbosacral magnetic resonance imaging (MRI) would be most helpful in cases in which the coccygeal pain is suspected to be referred from anatomic structures located more superiorly within the spine (ie, at the lumbar or sacral regions).
Computed tomography (CT) scanning and/or MRI of the pelvis can be helpful in cases in which intrapelvic pathology (ovarian, cervical, colon, testicular, or prostate cancer or their associated metastases) is suspected. [8]
Management of coccyx pain
Physical therapy for coccydynia may involve manually working on tight, painful muscular structures such as the levator ani, coccygeus, or piriformis muscles. Myofascial release techniques may be used. Local modalities also may be helpful.
Surgical treatment for coccydynia includes coccygectomy, in the form of partial or complete surgical removal of the coccyx. [9, 10]
One possible mechanism for persistent coccydynia is excessive activity or sensitivity of the ganglion impar, thus creating sympathetically maintained coccyx pain. [11] Local injection of an anesthetic can effectively block the ganglion impar and thereby relieve coccyx pain.
When the primary pain generator is thought to be at the sacrococcygeal joint, local injection can be administered to this site.
The authors of this article have found that in cases in which ischial bursitis is suspected as a substantial component of the patient's buttock pain, local injection of the bursa can be performed either with local anesthetic alone (diagnostic injection) or with corticosteroids (therapeutic injection).
Ablation can be used to intentionally destroy nerve fibers at the coccyx, so that those nerves can no longer send pain signals to the brain. Thermocoagulation of the ganglion impar using radiofrequency ablation (RFA) has been reported. [12, 13] Ablation can also be accomplished chemically (eg, by carefully injecting neurotoxic agents such as phenol and/or ethyl alcohol directly onto the targeted nerve tissues). These coccygeal ablation injections have been in clinical use for multiple decades and thus are no longer considered experimental. [2]
Osteopathic, chiropractic, or other "manual medicine" techniques to mobilize the coccyx are sometimes performed by clinicians who feel that the sacrococcygeal segments of a given patient have decreased mobility.
Anatomy
The coccyx is the terminal end of the spine, just inferior to the sacrum. The human coccyx is often considered a vestigial remnant or corollary of a tail; thus, the coccyx is colloquially referred to as the tailbone. The word coccyx comes from the Greek word for cuckoo, the name apparently having been derived from the tailbone’s shape, which resembles that of a cuckoo’s beak. [2]
The human coccyx is composed of 3-5 individual segments (coccygeal vertebrae), with variations occurring with regard to the number of segments, the overall angulation (curve) of the coccyx, and the degree of articulation versus fusion between the individual segments. In 80% of patients, the coccyx is made up of 4 coccygeal vertebrae. Typically, the coccyx is concave anteriorly and convex posteriorly.
The base of the coccyx articulates with the sacral apex via the sacrococcygeal junction. The sacrococcygeal articulation and intracoccygeal articulations contain fibrocartilaginous discs, somewhat comparable to the intervertebral discs present at other spinal levels. The apex (distal tip) of the coccyx is typically rounded, but may be bifid. (See the image below.)
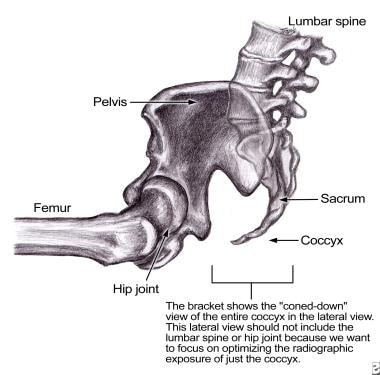 Lateral view of the pelvis and coccyx. The bracket shows the area of focus for radiographs that would provide a coned-down view of mainly the coccyx and distal sacrum. A more common lateral view would often also include larger bony structures, such as the lumbar spine and femur, all of which would make it difficult to optimize visualization of the small bones of the coccyx. In patients with coccyx pain, these coned-down, lateral views of the coccyx can provide important diagnostic information. Coned-down images obtained in the weight-bearing (seated) position can be compared with those obtained in a non–weight-bearing position (eg, side lying), thus allowing assessment for dynamic instability (eg, dislocations that occur only while seated).
Lateral view of the pelvis and coccyx. The bracket shows the area of focus for radiographs that would provide a coned-down view of mainly the coccyx and distal sacrum. A more common lateral view would often also include larger bony structures, such as the lumbar spine and femur, all of which would make it difficult to optimize visualization of the small bones of the coccyx. In patients with coccyx pain, these coned-down, lateral views of the coccyx can provide important diagnostic information. Coned-down images obtained in the weight-bearing (seated) position can be compared with those obtained in a non–weight-bearing position (eg, side lying), thus allowing assessment for dynamic instability (eg, dislocations that occur only while seated).
Muscles and ligaments
In humans, the coccyx serves important functions, including as an attachment site for various muscles, tendons, and ligaments. Physicians and patients should remember the importance of these attachments when considering surgical removal of the coccyx.
Muscles inserting on the anterior coccyx include the levator ani, which is sometimes considered as several separate muscle parts, including the coccygeus, iliococcygeus, and pubococcygeus muscles. This important muscle group supports the pelvic floor (preventing inferior sagging of the intrapelvic contents) and plays a role in maintaining fecal continence. A midline component is the anococcygeal raphe, by which the coccyx supports the position of the anus. [2] Muscles originating on the posterior coccyx include the gluteus maximus, which is the largest of the gluteal (buttock) muscles and which functions to extend the thigh during ambulation.
Multiple important ligaments attach to the coccyx. [2] The anterior and posterior sacrococcygeal ligaments attach the sacrum to the coccyx (similar to the functions of the anterior and posterior longitudinal ligaments spanning cervical, thoracic, and lumbosacral spinal segments). Laterally, the transverse process of the coccyx serves as an attachment site for the lateral sacrococcygeal ligaments (arising from the inferolateral sacrum), as well as for fibers from the sacrospinous ligament (arising laterally from the spine of the ischium) and the sacrotuberous ligament (connecting the sacrum with the ischial tuberosity, but with fibers attaching to the coccyx as well).
Function
The coccyx serves somewhat as a weight-bearing structure when a person is seated, thus completing the tripod of weight bearing composed of the coccyx and the bilateral ischium. The ischial weight-bearing surfaces are, more specifically, at the ischial tuberosities and inferior rami of the ischium.
The coccyx bears more weight when the seated person is leaning backward; therefore, many patients with coccydynia sit leaning forward (flexing at the lumbosacral and hip regions), which shifts more of the weight to the bilateral ischium rather than the coccyx (see the images below). Alternatively, patients with coccydynia may sit leaning toward one side so that the body weight is exerted mainly on one ischial tuberosity or the other, with less pressure on the coccyx. Such side leaning may lead to concomitant ischial bursitis in addition to the antecedent coccydynia.
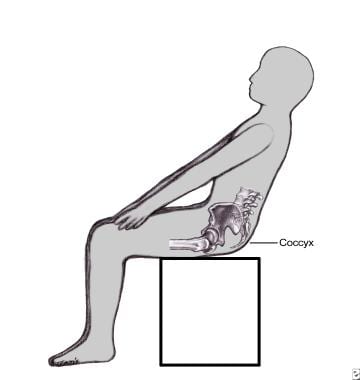 Coccyx pain (coccydynia, or tailbone pain) is typically worse when the patient is sitting. Often, the pain is even worse when sitting leaning slightly backward, since this increases the weight bearing on the coccyx, as shown in this image. Dynamic radiographs of the coccyx involve obtaining coned-down (focused) views of the coccyx while the patient is seated (eg, in his or her most painful position). Often, this involves having the patient lean backward 0-40°, depending on the symptoms. Radiographs obtained in this position are compared with those obtained in a non–weight-bearing position (eg, side lying) to assess for instability or dislocations in the seated position.
Coccyx pain (coccydynia, or tailbone pain) is typically worse when the patient is sitting. Often, the pain is even worse when sitting leaning slightly backward, since this increases the weight bearing on the coccyx, as shown in this image. Dynamic radiographs of the coccyx involve obtaining coned-down (focused) views of the coccyx while the patient is seated (eg, in his or her most painful position). Often, this involves having the patient lean backward 0-40°, depending on the symptoms. Radiographs obtained in this position are compared with those obtained in a non–weight-bearing position (eg, side lying) to assess for instability or dislocations in the seated position.
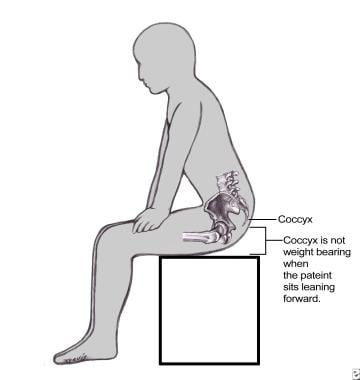 Patients with a painful coccyx often find it more comfortable to sit leaning slightly forward, as shown in this image. This forward-leaning position minimizes any weight bearing on the coccyx itself and thus minimizes the exacerbation of coccyx pain. As shown, when a patient sits leaning forward, most of the weight bearing occurs bilaterally through the inferior ischial regions of the pelvis and the posterior thigh (femur) regions.
Patients with a painful coccyx often find it more comfortable to sit leaning slightly forward, as shown in this image. This forward-leaning position minimizes any weight bearing on the coccyx itself and thus minimizes the exacerbation of coccyx pain. As shown, when a patient sits leaning forward, most of the weight bearing occurs bilaterally through the inferior ischial regions of the pelvis and the posterior thigh (femur) regions.
Etiology
Causes of coccyx pain include trauma, fractures, dislocations, and primary or metastatic malignancies. [14, 15, 16] (A retrospective study by Dang et al of primary spinal tumors [438 patients] indicated that those of the sacrum or coccyx are more likely to be malignant. [17] ) Sources of acute, abrupt trauma include internal trauma (eg, giving birth) and external trauma (eg, falling onto the coccyx). Nonabrupt trauma may include prolonged sitting. Tailbone pain may begin after certain medical procedures, such as colonoscopy. [18] Some cases of coccydynia are idiopathic, without any identified etiology.
One risk factor for coccyx pain is aging; degenerative changes of the sacrococcygeal junction and the intracoccygeal junctions, as well as fusion at these sites, seem to increase with age.
A gender-specific risk factor in females is trauma related to giving birth; substantial pressure may be placed on the coccyx as the baby descends through the mother's pelvis.
Epidemiology
Coccydynia is considered to be relatively uncommon, but data are lacking on the exact incidence and prevalence of the condition.
Coccydynia is seen in males and females; however, women seem to be affected more frequently than men. [3] As previously mentioned, one gender-specific risk factor in females is trauma related to giving birth; the coccyx may endure substantial pressure as the baby descends through the mother's pelvis.
Coccydynia can occur in children and adults. Degenerative changes of the sacrococcygeal junction and the intracoccygeal junctions, as well as fusion at these sites, seem to increase with age.
Prognosis
While some patients with coccydynia have complete relief via natural recovery over time, others develop a persistent, chronic pain syndrome at the coccyx region.
One proposed reason why coccyx pain seems to be more chronic than other injury sites is the inability to immobilize or brace the site (eg, as compared with bracing and casting that is available for injuries at the wrist, ankle, or others, but is not available for similar immobilization at the coccyx). This may contribute to delayed or prolonged recovery as well as the development of chronic, persistent, intractable pain syndromes.
Once the coccyx pain has become chronic (persisting for more than 3-6 mo), it may be less likely to resolve by natural recovery alone, more likely to continue indefinitely, more likely to be resistant to treatment, and more likely to require a multimodal treatment approach (eg, oral medications combined with local injections).
Early interventions (eg, oral medications, injections, physical therapy) are presumed to decrease the chance that acute coccydynia will develop into chronic coccydynia. This may be considered a reason for aggressive nonsurgical treatment early on, to potentially decrease the chances of lifelong pain and disability.
Although coccydynia is generally not associated with increased mortality, it is often associated with substantial morbidity. Patients with coccydynia often report severe and persistent pain that compromises functional activities requiring sitting and diminishes their quality of life.
A study by Kodumuri et al indicated that body mass index (BMI) and traumatic etiology independently predict coccydynia treatment outcomes. Individuals in whom coccydynia resulted from trauma seemed to respond better to treatment than did the other patients, with a higher mean outcome satisfaction score (80%) than that of the rest of the group (61%), at 6 weeks postintervention. Treatment responses also tended to be more favorable in patients with a BMI of below 30. [19]
One case series indicated that a positive coccygeal discogram is correlated with better outcome from surgery, but these results were based on small numbers, including just 2 surgical patients who had positive preoperative discograms and 2 surgical patients who had negative preoperative discograms. [20] Further, the usefulness of a positive discogram at predicting surgical outcome intuitively seems to be contraindicated by a separate, histologic study showing that disc degeneration at the sacrococcygeal joint in 5 patients was associated with poor surgical outcome in all 5 cases. [21]
Patient Education
The author of this Medscape Reference article (Dr. Foye) has provided further information on the topic of tailbone pain at the following websites:
-
Coccyx Pain Relief - A blog about coccyx pain
-
Dr. Foye's website on tailbone pain, at www.TailboneDoctor.com
-
Radio interviews with Dr. Patrick M Foye, specifically discussing tailbone pain - The interviews can be heard for free online.
-
Lateral view of the pelvis and coccyx. The bracket shows the area of focus for radiographs that would provide a coned-down view of mainly the coccyx and distal sacrum. A more common lateral view would often also include larger bony structures, such as the lumbar spine and femur, all of which would make it difficult to optimize visualization of the small bones of the coccyx. In patients with coccyx pain, these coned-down, lateral views of the coccyx can provide important diagnostic information. Coned-down images obtained in the weight-bearing (seated) position can be compared with those obtained in a non–weight-bearing position (eg, side lying), thus allowing assessment for dynamic instability (eg, dislocations that occur only while seated).
-
Coccyx pain (coccydynia, or tailbone pain) is typically worse when the patient is sitting. Often, the pain is even worse when sitting leaning slightly backward, since this increases the weight bearing on the coccyx, as shown in this image. Dynamic radiographs of the coccyx involve obtaining coned-down (focused) views of the coccyx while the patient is seated (eg, in his or her most painful position). Often, this involves having the patient lean backward 0-40°, depending on the symptoms. Radiographs obtained in this position are compared with those obtained in a non–weight-bearing position (eg, side lying) to assess for instability or dislocations in the seated position.
-
Patients with a painful coccyx often find it more comfortable to sit leaning slightly forward, as shown in this image. This forward-leaning position minimizes any weight bearing on the coccyx itself and thus minimizes the exacerbation of coccyx pain. As shown, when a patient sits leaning forward, most of the weight bearing occurs bilaterally through the inferior ischial regions of the pelvis and the posterior thigh (femur) regions.








