Introduction to Impairment and Disability Evaluation
Definition of terms
Impairment rating of neuromuscular conditions in the United States originated in the 1950s. The American Medical Association (AMA) released the first edition of its AMA Guides to the Evaluation of Permanent Impairment in 1971. [1] The sixth edition is currently available. [2]
The impairment rating is an estimate of the severity of human impairment based on acceptable medical standards (see the images below).
Various reference books, including the AMA Guides, provide a standard method of analysis to evaluate, report on, and communicate information about impairments to any human organ system. [3]
According to the AMA Guides, impairment is an alteration of an individual's health status that has been assessed by medical means. Impairment is used to describe a static or stable condition that has had sufficient time to allow optimal tissue repair and that is unlikely to change, despite further medical or surgical therapy. The Florida Impairment Schedule defines impairment as anatomic or functional abnormality or loss after maximal medical improvement (MMI) has been achieved.
The purpose of impairment rating is to represent impairment by using a generally accepted system to estimate the degree to which illness or injury diminishes an individual's capacity to daily activities. Activities of daily living (ADL) include self-care, personal hygiene, preparing and eating food, communication (spoken and written), maintaining posture, standing, sitting, caring for home and personal finances, walking, traveling, recreational and social activities, and work-related activities. An individual with an impairment may or may not have sufficient capacity to meet the demands of a particular profession or occupation.
Performing an impairment rating
First, the examiner should gather information to document the nature of the impairment and its consequences. Review the patient's medical history, as well as his or her office and hospital records. Use multiple sources of information to promote objectivity and eliminate bias. For purposes of evaluation, the patient's medical condition should be stable and unlikely to change in the future despite further treatment. Treatment at this point is palliative rather than restorative.
Obtain clinical information from the patient's medical records and from physical examination. Compare clinical information from several sources to check for consistency. Resolve disparities when possible, if the clinical information is inconsistent. Use medically accepted and scientifically derived data based on the patient's normal functioning whenever data are available. The impairment rating values in the guides estimate the extent of impairments based on the authors' clinical experience, judgment, and consensus. Impairment ratings are estimates of the degree of impairment, based on the physician's judgment, experience, training, skill, and thoroughness.
Other factors in determining the rating of impairment include a consideration of the sensitivity, specificity, accuracy, reproducibility, and interpretation of findings from laboratory and clinical procedures, as well as a recognition of interobserver variability in interpretation.
In the impairment-rating process, a number derived from well-structured and thorough observations is assigned. The strength of medical support for an impairment estimate depends on the completeness and reliability of the patient's medical documentation. The rating does not convey any information about the effect of the impairment on the person's capacity to meet personal, social, or occupational demands.
The fourth edition of the AMA Guides suggests, "If, in spite of an observation or test result, the medical evidence appears not to be of sufficient weight to verify that an impairment of a certain magnitude exists, the physician should modify the impairment estimate accordingly, describing the modification and explaining the reason."
Impairment versus disability
Many practitioners confuse the terms impairment and disability. Disability refers to an individual's inability to complete a task or a duty. Disability is an alteration of the individual's capacity to meet personal, social, or occupational demands or statutory or regulatory requirements because of an impairment. Disability arises from a discrepancy between the limitations an impairment places on an individual and the external tasks that must be performed (eg, tasks in an occupational setting).
Impairment, however, is an artificial construct—usually one the legal system creates—to attempt to quantify the person's diminution in health. According to the fourth edition of the AMA Guides, "An impairment is a deviation from normal in a body part or organ system and its functioning." However, normal is a vague term that varies greatly depending on many factors, such as age and sex. Normal is not a fine point or an absolute reference in terms of physical and mental functioning or good health. Most often, normality is a range or a zone, as it is with vision and hearing.
Many state disability systems adopt an impairment guide or schedule for calculating damages. For example, Florida has adopted the Florida Uniform Permanent Impairment Rating Schedule (FUPIRS). This schedule is loosely modeled after the AMA Guides and purports to give impairment ratings based on various injuries or illnesses.
As a practical example, an individual may have minor impairment and still be considered totally disabled. For instance, an uneducated bricklayer may have 5% impairment due to lumbar strain. His physical restrictions may make it impossible for him to continue working in his field, and if he does not have the education to be retrained, he is effectively unable to return to work. Therefore, the extent of his impairment may be only 5%, but he is l00% disabled in terms of employment. In another example, a noted author and lecturer may have sustained a catastrophic injury causing thoracolumbar paraplegia. His impairment rating may be 70% according to the AMA Guides. However, because he can continue his work with little to no interruption, he may be considered to have no vocational disability.
A study by Farzad et al found only a limited association between impairment and disability in patients with hand injury. Using the AMA Guides to assess impairment, as well as the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire and the Michigan Hand Outcomes Questionnaire (MHQ) to measure disability, the investigators found that impairment level, together with gender, was responsible for only 22% of DASH score variability and, together with age, only 19% of MHQ score variability. Moreover, impairment level did not correlate with pain intensity, although other factors, including time since surgery, did. The study included 107 patients, who were followed up a mean 11 months after their hand injury. [4]
In summary, the impairment rating alone, without a consideration of the extent of disability and loss of function, does not provide a complete picture of the effect of illness or injury on a particular individual.
Concepts in Disability Evaluation
Overview
Evaluating disability is more complex and involved than the impairment rating discussed in the previous section. By definition, disability involves a consideration of many factors beyond the purview of impairment rating. Although impairment addresses a loss or deficit in any psychological, physiologic, or anatomic structure or function, disability encompasses vocational, educational, psychosocial, and financial factors, to name only a few, in addition to the rated impairment.
Whereas the impairment-rating system incorporates a coefficient of impairment, assessment of disability has no such rating system, but disability benefits are awarded by means of an administrative process the Social Security Administration (SSA) developed as a result of the Social Security Act Amendments of 1954. These amendments established the Disability Determination Units, through which claimants are referred to clinical examiners for an assessment of impairment in regard to appeals regarding Social Security Disability Income (SSDI) that the SSA adjudicates.
Assessment systems
SSA system
The most established disability-assessment system is the one the SSA developed for persons who claim a degree of impairment that makes the resulting disability significant. That is, impairment is significant enough that these individuals report being completely incapable of engaging in gainful employment, and, thus, they are unable to support themselves independent of state or federal subsidy.
The SSA expanded the traditional definition of impairment in determining an individual's fitness for work by adding consideration of factors that define function as a part of the disability assessment. For example, individuals who allege that they cannot work because of angina pectoris may find that the condition itself is not enough to permanently disqualify them from work. In evaluating the individual's ability to function in a clinically controlled work setting with typical physical and mental simulations, other issues directly related to diagnosis may apply. Examples are the character, location, and duration of pain and how it evolves, what relieves it, and how quickly relief is achieved. These factors, in addition to the patient's diagnosis, may be enough for the clinical examiner to recommend that the patient not return to gainful activity.
The SSA disability-evaluation process is bureaucratic, lacking a skilled and well-trained medical examiner. An analysis reviews all medical records, with input from a medical review officer but without any interaction with or examination of the claimant. Therefore, as Pace states, the records must be sufficiently complete to enable any independent reviewer who does not examine the claimant to determine the nature, limiting effects, and duration of impairment on the basis of only the written reports. [5] The quality of the review is contingent on the cooperation of the medical community to provide records to the SSA, a shortcoming of the current review process.
The Social Security Disability Evaluation System (SSDES) heavily relies on the establishment and definition of the respective diagnosis and on the principle that diagnosis can be determined objectively by using diagnostic and laboratory studies. Function is a secondary consideration, or, in terms of the 1994 AMA impairment-rating protocols, its application is that of a differentiator in determining the degree of impairment or the residual functional capacity of the claimant outside impairment parameters. In essence, function merits little consideration in impairment rating. Other systems predating the SSA evaluation process similarly focused on impairment, with some acknowledgment given to the effect of function on impairment.
McBride system
The earliest system, the McBride system (1936), was based on Workers' Compensation law and readily adopted by Workers' Compensation Boards in various states. The fundamental principle was that functional and/or social deficiencies were as relevant as impairment itself. Therefore, McBride implemented an average rating test that included the component of disabling functional deficiencies in addition to the component of disabling physical impairments, as follows [6] :
Disabling physical components include the following:
-
Anatomic and physiologic tissue damage
-
Clinical manifestations
-
Restrictions on work restoration
-
Restrictions on working conditions
-
Intangible and reactionary influences
Disabling functional deficiencies include the following:
-
Intangible and reactionary influences
-
Coordination
-
Strength
-
Endurance
-
Security
Earl McBride, MD, first expressed the problem of standardization in evaluating impairment, stating, "[G]uessing at percentages seems to be more in order than scientific reasoning. Consequently, the industrial commissioners in weighing and applying the evidence often make a practice of splitting the difference in percentages instead of weighing the facts scientifically. This is a reflection on the integrity of the medical profession more than it is on the commission."
Efforts of the AMA
It was not until 1956, around the time of the Social Security Act Amendments, that the AMA studied the issue of standardization in impairment rating. The AMA Board of Trustees appointed an ad hoc committee of physicians to develop standards for rating disability and impairment and to compile guides that all physicians could follow. From the deliberations of this committee evolved a structured framework and method of analysis "...through which physicians [could] evaluate, report on, and communicate information about the impairments of any human organ system."
What the AMA had hoped to establish was a standardized system for physicians, one that could produce consistent ratings, perhaps with models for standard calculations for impairments rated by 2 or more independent physicians at different times. However, in the decades since the AMA committee met, the goal of establishing a universally accepted method has seemed untenable, although evaluation standards have been established. The medical community remains divided on whether to use the guides and accompanying evaluation protocols, and questions have been raised about reliability and validity associated with the AMA standards and protocols. The establishment of consistent evaluation standards that impairment-rating clinicians use has not been attained yet.
American Academy of Orthopaedic Surgeons' manual
The American Academy of Orthopaedic Surgeons published the Manual for Orthopedic Surgeons in Evaluating Permanent Physical Impairment in 1962. This manual was based on the AMA protocols (eg, range of motion [ROM], amputation) but deviated somewhat, as it included a pain scale in line with documented organic pathology. The manual further included impairment ratings for orthopedic conditions and procedures not included in the AMA Guides. For example, in this rating system, fractures of the tibial plateau are considered to be a possible source of impairment, and the extent of the pain associated with this diagnosis is rated as well.
Kessler's Disability: Determination and Evaluation
H. Kessler, MD, published Disability: Determination and Evaluation in 1970, which was somewhat based on the McBride model. However, he focused on loss of function in his disability decision. Although Kessler supported McBride's efforts to delineate the physical and functional components of disability, he maintained that units of measure could be assigned to these components to provide a rational rating coefficient. Although this approach is valid for assessing the upper extremities (UEs) and lower extremities (LEs), rating the 3 spinal regions remains difficult. Kessler rationalized that emotion was the dominant factor in the persistence and intensity of back pain and noted that, in most patients reporting this problem, pain was the only complaint. He concluded that the impetus of rating spinal impairment was to use criteria based on the successful performance of ADLs.
Current challenges
The focus of this article thus far has been a review of the common and peer-reviewed disability rating systems that the medical community and the judicial system currently accepts and uses. The systems reviewed emphasize the documentation of impairment, with disability as a secondary consideration in the examiner's clinical judgment of whether a person is disabled or not. This emphasis remains true today despite the mandate of the Americans with Disabilities Act of 1990 to integrate job simulation and assessment of the claimant's ability to function into medical-examination protocols for return-to-work after disability leave.
The question remains: Why has the medical community avoided an evaluation of true work function based on biomechanical and ergonomic simulation, preferring the traditional independent medical examination (IME) method of systems review, reflex studies, strength measures, and records review?
The answer to that question may be found in a review of the literature regarding attitudes, training, and misuse of terminology that has perplexed the medical and judicial system for years. In 1983, Ziporyn interviewed Talmadge Hiebert, MD, founder of the National Association of Disability Evaluating Professionals (NADEP). [7] Hiebert took issue with terms used in the rating forms of workers' compensation and the SSDI programs, on which the disability and impairment were used interchangeably. He remarked that the examining physician is confused when asked about disability versus impairment issues. Hiebert further commented that physicians do not receive any formal training in their medical-school programs regarding evaluating or measuring function and that peer-reviewed articles about measuring functional capacity usually do not appear in the medical journals and instead appear in physiology, ergonomics, and exercise journals.
In 1988, Luck and Florence acknowledged that the problem rests primarily with a lack of standardization among medical specialties. [8] They specifically noted that many physicians use more than 1 system for disability evaluation or impairment rating. Like Hiebert, they found that many physicians are uncertain about the difference between impairment and disability when drawing conclusions from their ratings.
One interesting observation was that impairment rating is often viewed as an onerous and frustrating task because it lacks the positive reinforcement of helping the sick patient and strains the physician-patient relationship. In other words, physicians prefer the role of healer and medical practitioner to that of examiner of impairment and/or disability, which often leads to an adversarial relationship between themselves and their patients.
In 1993, Abdel-Moty et al identified the problem primarily as a skill deficiency among physicians, who have great difficulty in translating the results of medical impairment evaluations into functional measures. [9] Physicians have not had adequate training in functional measurement and disability evaluations to allow them to translate impairment into functional disability.
Demand for impairment ratings and functional-capacity evaluations
Despite the problems discussed above, impairment-rating services and functional-capacity evaluations (FCEs, ie, disability examinations) are in high demand from the legal and insurance professions because of rising healthcare costs and subsequent lawsuits. The demand is specifically high in the areas of personal injury (eg, auto liability), work-related injury (ie, workers' compensation [10] ), and product liability. Ziporyn stated, "[E]ach year American physicians receive hundreds of thousands of requests to determine impairment and disability, and every physician at some point in his or her career will be called upon to do so." [7]
Occupational statistics further support the need for such services, expanding the scope of the medical-service delivery system at a rapid pace. A study by Dieleman et al reported that in 2013, low back and neck pain were associated with an estimated $87.6 billion in personal healthcare spending in the United States, the third-highest amount that year, with the annualized rate of change for spending on these conditions between 1996 and 2013 coming to 6.5%. [11]
The insurance and legal communities have recognized the need for disability and impairment-rating services, given that in the United States between 1998 and 2010, direct workers’ compensation costs associated with the most disabling, compensable, nonfatal injuries and illnesses reached over $600 billion. [12] Physicians who have previously spurned the legal community, who scoffed at dealing with attorneys, or who refused to view their physician-patient relationships as adversarial should learn to embrace and nurture this potential service-contract opportunity.
Practitioners are constantly battling with the insurance industry to pay fees as billed, fighting the nuances of managed care and health-maintenance organization (HMO) programs, and coping with the customary and usual fee-for-service letters that reject bills and pay what the insurance industry believes the service is worth, not to mention the training and expertise required for provision of said service. Whatever terms are applied in a litigious setting (eg, forensic medicine, disability examinations, IMEs, FCEs), full 100% reimbursement for services rendered must be allowed. The future financial health of practicing clinicians may rest in the courtroom or administrative-law hearing room.
The 14-point Walter Reed Functional Impairment Scale was designed to evaluate functioning by members of the working military population in physical, occupational, social, and personal domains. A 2014 study by Herrell et al involving 3,380 soldiers found the scale to have great reliability and validity, demonstrating a Cronbach’s-alpha value of 0.92 and a strong correlation between both the individual items and the quartiles of sum scores with negative performance both occupationally and socially. The investigators also found results derived from the scale correlated strongly with posttraumatic stress disorder (PTSD), depression, and high levels of generalized physical symptoms. [13]
FCE systems
The most effective system for assessing disability in a forensic setting is the FCE protocol. This technique allows for the rating of impairment, as well as an examination of the person's ability to function in tasks, with standard norms simulating the mechanics of work.
Background
Klimek and Strait, as well as May, characterized the purpose of the FCE to access and predict work behavior and vocational potential, as well as to match a given level of work performance to appropriate tasks with a margin of safety that reduces likelihood of reinjury. [14, 15] The applications are numerous in terms of workers' compensation, personal injury, or product liability cases. One application is when an injured worker achieves MMI and the physician wants to know what work restrictions to document before releasing the patient from care.
The FCE can be used to document specific work tolerances and recommendations for the biomechanics of those tasks, detailing for the attending physician what restrictions should be applied. [16] If a discrepancy exists between the physician's findings and the examinee's complaints, the FCE can offer evidence of the complaints and specific diagnosis based on repeated measures and/or testing techniques, psychometrics, and behavioral observations.
In a study of 27 insurance physicians, Wind et al gave the doctors 2 chances to score the physical work ability of 2 insurance claimants with a musculoskeletal disorder—1 of whom had performed an FCE—on 12 activities. [17] The investigators found that the physicians most often changed their judgment regarding the claimant's work ability when taking the FCE into account (141 times vs 102 times for the control).
In another study, of 28 insurance physicians, Wind et al found that almost 68% of the doctors stated that an FCE was of complementary value in assessing the physical work ability of insurance claimants with a musculoskeletal disorder. [18]
A comparative analysis of current FCE programs and instruction on how to perform an FCE are beyond the purpose of this section. Instead, a few of the FCE programs reviewed in the literature are presented below.
Several FCE protocols have been published, along with detailed reviews of their application in the FCE process. [15, 19, 20, 21, 22, 23, 24, 25] In 1984, May first described a protocol he developed on the basis of the Matheson model, which incorporated job analysis, work-simulation activities, materials-handling assessment, and testing of gross muscle strength. [22, 23] In 1988, the role and function of the staff members on the FCE team was documented. [24] Hart et al reviewed specific FCE components, including (1) recording the examinee's history, (2) conducting preevaluation screening, (3) performing functional-capacity testing, (4) interpreting the results, and (5) writing a report of the findings. [20]
Isernhagen conceptualized the role of the physician in the FCE process with her assessment of the purpose of FCE, that is, to assess the examinee's maximum physical capabilities to arrive at a statement of the extent of the examinee's impairment. [26] Therefore, her statement alone suggests the involvement of a multidisciplinary team to determine the person's functional capacity and resulting impairment.
Hart et al supported this team concept, noting that the FCE: "combines a comprehensive neuromusculoskeletal examination [physician, physio/occupational therapist working as one evaluation team] with measurements of physical impairment, symptom magnification/worker behaviors, and function and culminates with the measurement of the current functional abilities of the client." [20]
A literature review by Ansuategui Echeita et al found that in adults undergoing an FCE, strong evidence exists that FCE performance is associated with the country where the evaluation is taking place, as well as with the examiner’s fear behavior, while moderate evidence exists that previous job salary also affects performance. However, evidence was low or very low that certain other social factors, including compensation status, litigation status, and ethnicity, are linked to FCE outcome. [27]
A study by Schindl et al supported previous results from these investigators indicating that in patients with musculoskeletal trauma, a link exists between FCE and a subsequent increase in patient-reported function. Using the WorkWell Systems FCE, which had also been employed in the first study, the investigators evaluated two separate cohorts, determining post-FCE function increases via Spinal Function Sort (SFS) questionnaire scores. The three cohorts, including the original (recruited in 2016) and the two new ones (recruited in 2017 and 2018), reported functional-ability improvements of 14.8, 14.8, and 15.3 points, respectively. [28]
NADEP protocol
The researched protocol with established construct validity is the one Dr. Talmage Hiebert of the NADEP developed and which May and Martelli refined in 1999. The NADEP FCE model is predicated on the work-capacity evaluation (WCE) protocol that Dr. L. Matheson of the Employment and Rehabilitation Institute of California researched and established.
One of the primary components this last FCE model, and all subsequent ones, is the analysis of materials handling and lifting.
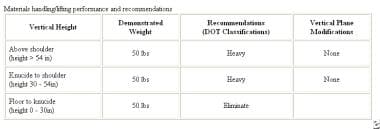
This component is essential, because most individuals referred for WCE have musculoskeletal injuries due to work-related lifting and falling accidents that culminate in orthopedic-related diagnoses. Therefore, the NADEP model must focus on documenting the functional integrity of a worker's materials-lifting and materials-handling capabilities to determine the most feasible work criteria for returning while maintaining acceptable safety and productivity.
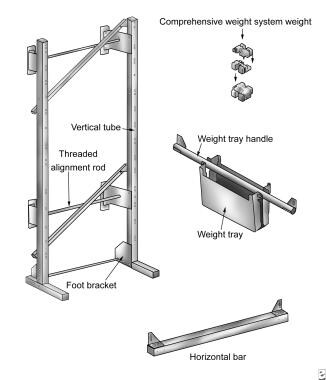
Matheson developed the lifting protocol in the NADEP model by using the Work Evaluation System Technology (WEST) evaluation system (see the image below).
This lifting evaluation system is the one that the NADEP protocol incorporates because of Matheson's timely research into the safety and application of this component in the FCE process.
The WEST system was developed to evaluate the lifting capacity of workers who have had various industrial injuries, using the full vertical work plane while gradually increasing the examinee's workload. The system is safe to administer and complies with the criteria for physical assessment measures published by the National Institute of Occupational Safety and Health (NIOSH). Furthermore, Matheson established that the instrument is reliable on repeated-measures testing and that the results compare favorably with isometric measures of lifting capacity.
Despite its focus on materials handling, however, the NADEP Work Disability Evaluation Model incorporates 5 other components: (1) clinical interview and/or intake screening, (2) patient profiling, (3) work–vertical plane functional ROM/systems examination, (4) grip-strength testing, (5) static validity and/or reliability and dynamic strength tests, and (6) domain testing.
The 6 components that constitute the NADEP model are easily documented and calculated by hand. However, with the advent of computerized systems and evaluation software the NADEP model has become an expedient evaluation tool that can now combine impairment-rating coefficients in its summary interpretations. In this way, it can provide the referring source with a combined report on functional capacity and impairment rating.
See the Example of Disability Evaluation section below for a case study that applies this protocol.
Other, including computerized, models
The NADEP model is only one of many FCE protocols, and the reader is encouraged to review all the models published in the literature. The reader can find a multitude of FCE computerized systems that advertise complete, valid, and reliable FCE programs that can withstand the scrutiny of litigation. These systems sell the clinician on the concept that they are designed to save time and effort because the system performs all the calculations and presents the data in nicely ordered tables with bar or line graphics of the repeated measures.
The reader is cautioned not to rely on these systems to complete the FCE in a valid and reliable manner. The FCE process and its administration are only as good as the examiner. The quality of the FCE administration and the interpretation of its results rest solely with the experience and training of the examiner and not with the equipment used.
Reliability and validity of FCE
Background on reliability and validity research
The issue of reliability and validity in the FCE process remains, despite the quality of the computerized system or the preferred manual method. Although Babisky and Sewall identified reliability and validity issues in the impairment rating process, little data suggest that the validity and reliability issues associated with FCE have been resolved satisfactorily. King et al identified a lack of validity and reliability as a major concern in their review of 10 major computerized FCE systems, 8 of which are well known and accepted in the US marketplace. Only 2 systems achieved peer-reviewed interrater and intrarater reliability research, and associated peer-reviewed validity study was available for only 1.
Lechner et al similarly took issue with the lack of established reliability and the potential for abuse in interpreting results from the application of test components in FCE protocols. They reviewed application of the Waddell nonorganic signs, the coefficient of variation, and the interpretation of heart-rate fluctuations with incidences of pain and concluded that these components may be misinterpreted and/or unreliable for determining maximum voluntary effort in the FCE. Overinterpretation or misinterpretation may lead to false-positive results or to identifying the examinee as one who is magnifying symptoms or malingering or as one who may not be suitable for the competitive labor market.
An accurate assessment of a patient's willingness to exert maximal effort during FCE is critical to interpreting the results of the evaluation. In a study by Lemstra et al, 90 patients with low back pain were evaluated for maximal effort during FCE. [29] The tester's opinion on the patients' results on the maximal-effort tests had an overall specificity of 84.1% and a sensitivity of 65.2%. Only 5 of 17 commonly used maximal effort tests were individually useful in differentiate between maximal effort and submaximal effort. The authors concluded that caution should be exercise when one identifies patients as giving maximal or submaximal effort during FCE.
Little doubt exists that more research is needed in the disability-examination process, both in the medical field regarding IMEs and in the allied-health professions involved in FCEs. As King et al noted, the overall quality of the examination process hinges on the examiner's competence and specific training. Poor training or inadequate preparation of evaluators can confound reliability and validity, perpetuating a rater effect in the testing protocol of the independent medical evaluation and FCE. The rater effect surfaces when results are extrapolated from the clinical examiner's personal biases or when the examination protocol is violated and its results are misinterpreted because of the examiner's lack of methodologic training.
Although the review by King et al was thorough regarding FCE equipment, they based their conclusions on the quality of the equipment rather than on the FCE process itself. [30] As noted before, the solution for this dilemma lies in the evaluator's skill and training and not in the type of equipment chosen FCE. The NADEP maintains that rater error and skill deficits can be minimized by establishing a standardized or consistent evaluation protocol across all specialties complete with consistent terminology. The NADEP attempted to achieve this goal with its FCE-researched protocol.
FCE systems reviewed
Since the inception of the FCE process, numerous designers of evaluation equipment have striven to build the optimal system. First, they wanted to take advantage of the expanding need for systematic application of testing components to minimize the time required of the therapist, physician, or evaluator and thus enhance productivity. Second, they wanted to establish their vendor's company as a leader in equipment design and function. The market demanded not only user-friendly equipment for measuring function but also equipment that had undergone the scrutiny of reliability and validation in peer-reviewed studies.
As noted earlier, King et al reviewed the 10 FCE systems or the equipment vendors that produce the most recognized FCE systems, 8 of which are from the United States or Canada and 2 from Australia. [30] The table below summarizes these systems.
Table 1. FCE Systems and Their Reliability and Validity (Open Table in a new window)
FCE System |
Developer |
Validity |
Reliability |
Hanoun Medical (not included in the original review by King et al) |
Reed Hanoun |
In progress |
In progress |
Blankenship |
Keith Blankenship |
No |
No |
Isernhagen Work Systems |
Susan Isernhagen |
No |
No |
Physical Work Performance Evaluation (Lecher, 1994) |
Deborah Lechner (ErgoScience) |
Yes |
Yes |
WEST-EPIC |
Leonard Matheson |
Not available |
Yes |
Key |
Glenda Key |
No |
No |
ERGOS* |
Work Recovery, Inc |
Yes |
Not available |
ARCON |
Dana Rasch |
No |
No |
Assess Ability |
Michael Coupland |
No |
No |
Note.—King et al (1998) reviewed 2 Australian systems not well known in this country and therefore excluded from this table. |
|||
The literature about reliability and validity was reviewed for the Isernhagen Work Systems FCE, the Blankenship system, the ERGOS Work Simulator, and the Ergo-Kit. The search resulted in 77 potentially relevant references, but only 12 were included and assessed for methodologic quality.
The interrater reliability and predictive validity of the Isernhagen Work Systems FCE was good, though the procedure used in the studies of interrater (test-retest) reliability was not rigorous enough to allow for any conclusion. Reneman et al studied the test reliability of the Isernhagen Work Systems FCE. The test-retest reliability of the material-handling group was acceptable. Crude analyses of the ceiling and criterion tests revealed acceptable test-retest reliability of most, but not all, tests. [31]
The concurrent validity of the ERGOS Work Simulator and the Ergo-Kit was not demonstrated, and no study of their reliability was found. Likewise, no study was on the reliability and validity of the Blankenship system was found.
The conclusion was that more rigorous studies are needed to demonstrate the reliability and the validity of FCE systems, especially the Blankenship system, the ERGOS Work Simulator, and the Ergo-Kit. [32]
Validity of FCE in work-related applications
Gross examined the validity of the Isernhagen Work Systems FCE in predicting timely return to work. [33] He found that 4% of patients passed all evaluation tasks, yet most had temporary total disability suspension and claim closure within 1 year after the FCE. Floor-to-waist lift performance had the same predictive value for timely return to work as the number of tasks failed in the entire FCE protocol had.
Insurance carriers have questioned the validity of FCEs. [34, 35, 36] In a review by Pransky and Dempsey, test criteria and the application of results were discussed. [37] The validity of FCE results was optimal with accurate job simulation and detailed, intensive assessments of specific work activities. When test criteria were unrelated to job performance, or when subjective evaluation criteria were used, the validity of the results is questionable. Reliability in a subject over time may be adequate to support serial FCE data collection to measure progress in worker rehabilitation. [38]
Data from Harbin and Olson support testing after a job offer is made and before placement. [39] Strength testing alone was of no value in predicting the incidence of work injury, though physical capacity was strongly correlated with physical job requirements. Injury rates were lower in employees who had the physical strength or ability to perform the essential functions of their jobs than in those who did not. The incidence of low back injuries in workers with or without the physical capability to perform the required job functions was 3% or 33%, respectively. Results from physical-capacity testing in which lifting ability is compared with the lifting requirements of the job were correlated with the incidence of work injury. The application of appropriate postoffer, preplacement testing is a cost-effective method to lower the incidence of work-related injuries.
Gross discussed concerns about what FCE really measure. [40] Although raters' judgments about a patient's maximum performance during FCE appear reliable, FCEs do not appear to be purely tests of physical capacity because many personal and environmental factors affect the patient's performance. FCEs are most accurately considered behavioral tests influenced by many factors, including physical ability, beliefs, and perceptions, and the results should be interpreted within the subject's broad personal and environmental context.
In a comparison of the ERGOS Work Simulator and the Ergo-Kit), researchers concluded that the concurrent validity for lifting between was poor for both FCE methods. [41]
Factors that affect performance on FCE
In 2003, Geisser discussed the effect of psychosocial factors on FCEs. [42] He stated that although psychosocial factors "have been found to have a significant impact on functional activity, particularly among persons with chronic pain," his review of the literature indicated that few psychosocial factors had been found that were "directly associated with FCE and functional measures, although many are related to various measures of disability."
Geisser found that the "strongest evidence that psychosocial factors are related to functional performance is based on the studies examining the association between functional activity and pain-related fear, self-efficacy, and illness behavior. Psychosocial factors have also been shown to influence measures of sincerity of effort often obtained during FCE."
Perception of the patient also influences performance on FCEs. In 2005, Good, discussed factors that influence performance on FCEs, stating:
Only the PDI (Pain Disability Index), pain intensity, age, and sex independently contributed to floor-to-waist lift performance. The PDI, pain intensity, and duration of injury contributed to the number of failed tasks. The results indicate that performance on FCEs is influenced by physical factors, perceptions of disability, and pain intensity. However, perceptions of workplace organizational policies and procedures were not associated with FCE results for workers' compensation claimants with chronic back pain disability. FCEs should be considered behavioral tests influenced by multiple factors, including physical ability, beliefs, and perceptions.
Other considerations
FCEs are behavioral assessments that are influenced by pain. Increased pain levels during and FCE can reduce performance levels. Therefore, pain factors must be taken into consideration when making predictions about future work status. Gross suggests that shorter FCEs be considered to address this effect. [43]
Taking this into account, a short-form FCE was compared with the traditional FCE. Floor-to-waist lift, crouching, and standing were maintained in the short-form FCE. This limited evaluation was found to predict comparably with the entire FCE protocol in 2 validation cohorts. [44]
Conclusion
The medical-service delivery system must adjust to the influences of managed care, HMO programs, and insurance capitation policies to control expenditures for medical benefits. Physicians must diversify into markets that they have not approached or even considered, given the current practice and business trends. The market for forensic services is thriving and seeks physicians to provide impairment ratings, IMEs, and FCEs to meet the escalating demand in personal-injury and product-liability litigation. The practicing physician may not know the FCE process, but it is one that effectively addresses the issue of disability and helps in identifying the functional deficits and capabilities of a patient with disability.
Almost as many manual disability-evaluation protocols exist as computerized disability-evaluation systems. The clinician is cautioned to approach FCE practice by first choosing a protocol that meets the scrutiny of the judicial system and by then selecting the FCE system that is flexible in accepting the chosen FCE protocol.
Impairment Rating Guides
Many states and jurisdictions have statutory requirements requiring the use of specific evaluation systems or guides to determine a permanent impairment rating (PIR) due to accident or injury. Some systems incorporate a disability schedule to supplement or complement the impairment-rating schedule. Many states place restrictions on which clinicians can provide impairment ratings. In Florida, for example, chiropractic physicians may issue ratings, but psychologists may not.
Although the American Board of Medical Specialties (ABMS) currently does not provide certification in impairment and disability evaluation, other organizations do. Certification for impairment rating may be obtained from the NADEP and the American Academy of Disability Evaluating Physicians (AADEP). These organizations provide education, training, and certification in impairment rating and related issues. Both organizations provide instruction by physicians and other healthcare professionals about impairment and disability-related issues.
Although certification is not required, if the healthcare professional foresees performing a substantial number of impairment rating evaluations, attendance at courses on the evaluation process is suggested. Disability medicine is the most likely of all areas of medicine to involve attorneys. Completion of a training course with certification by the AADEP or the NADEP increases the likelihood of a successful forensic experience.
Examples of guides include the following: the AMA Guides to the Evaluation of the Evaluation of Permanent Impairment, 6th edition, 2008 (order from the AMA), the 1996 FUPIRS, the Minnesota Disability Schedule, and the California Workers' Compensation Rating System.
Some states permit physicians to render impairment ratings based solely on their own experience and observation. This system presents a classic dichotomy between statutory permissiveness and scientific reliability (see Daubert v Merrell Dow Pharmaceuticals, Inc, 509 US 579 (l993).
Impairment Rating Examples
Impairment ratings have been calculated by using 2 systems. Eleven case examples and solutions are included here as examples. For specific cases, actual guides must be used. Further resources can be found at WorkersCompensation.com, where Florida's system is discussed extensively.
Please refer to the following PDF for the tables mentioned in the solutions below:
Tables from the Florida Uniform Permanent Impairment Rating Schedule (FUPIRS) (PDF)
Case 1. Shoulder impingement
A 37-year-old right-handed worker presents with impingement syndrome of the left shoulder. Examination of the left shoulder shows moderate crepitation with limited active ROM (AROM), as follows: left shoulder flexion 100°, abduction 90°, internal rotation 60°, and external rotation 60°. Radiography shows arthritic changes in the acromioclavicular joint of the left shoulder. MRI shows impingement of the left shoulder (referred to here as the UE).
Solution A (FUPIRS by ROM) is as follows:
-
3/46 (Table 14) Flexion 100° = 5% UE
-
3/48 (Table 16) Abduction 90° = 7% UE
-
3/49 (Table 17) Internal rotation 60° = 0% UE
-
3/49 (Table 17) External rotation 60° = 5% UE = 17% UE
-
Intro/6 Rule 2. Subtract 10% for nonpreferred arm.
-
17% UE - (17% UE X 10%) = 15% UE
-
3/58 (Table 21) 15% UE = 9% whole person (WP)
Solution B (FUPIRS by diagnosis) is as follows:
-
3/50 Impairment because of other disorders of UE
-
3/50 (Table 18) Shoulder AC joint maximum 30% UE X 3/51 joint crepitation 20% = 6.0% UE
-
3/58 (Table 21) Convert UE to WP 6.0% UE = 4.0% WP
Solution C (AMA Guides by ROM) is as follows:
-
3/43 (Figure 38) Flexion 100° = 5% UE
-
3/44 (Figure 41) Abduction 90° = 4% UE
-
3/45 (Figure 44) Internal rotation 60° = 2% UE
-
3/45 (Figure 44) External rotation 60° = 0% UE = 11% UE
-
3/20 (Table 3) Convert UE to WP 11% UE = 7% WP
Solution D (AMA Guides by diagnosis) is as follows:
-
3/58 Impairment because of other disorders of the UE
-
3/58 (Table 18) Shoulder AC joint maximum 25% UE X 3/59 (Table 19) joint crepitation 20% = 5.0% UE
-
3/20 (Table 3) Convert UE to WP 5.0% UE = 3.0% WP
Case 2. Shoulder arthroplasty
A 35-year-old right-handed man presents with right shoulder impingement after arthroscopic surgical acromioplasty (ie, arthroplasty). Examination shows a tender subdeltoid region with slight pain and constant moderate crepitation during AROM. The patient has full active and passive ROM. (Note: Calculations are performed with and without the surgical option.)
Solution A (FUPIRS by ROM) results in impairment = 0% WP
Solution B (FUPIRS by diagnosis, if no surgery is performed) is as follows:
-
3/50 (Table 18) Shoulder - acromioclavicular maximum 30% UE
-
3/51 Joint crepitation - moderate 20% joint
-
Multiply 30% UE X 20% = 6% UE
-
3/58 (Table 21) Convert UE to WP 6% UE = 4% WP
Solution C (FUPIRS by diagnosis, if surgery is performed) is as follows:
-
3/54 (Table 20) Shoulder resection arthroplasty 24% UE
-
3/58 (Table 21) Convert UE to WP 24% UE = 14% WP
Solution D (AMA Guides by ROM): Impairment = 0% WP.
Solution E (AMA Guides by diagnosis, if no surgery) is as follows:
-
3/58 (Table 18) Shoulder - acromioclavicular maximum is 25% UE.
-
3/59 Joint crepitation - moderate 20% joint
-
Multiply 25% UE X 20% = 6% UE
-
3/20 (Table 3) Convert UE to WP 5% UE = 3% WP
Solution F (AMA Guides by diagnosis, if surgery performed) is as follows:
-
3/61 (Table 27) Shoulder - resection arthroplasty 10% UE
-
3/20 (Table 3) Convert UE to WP 10% UE = 6% WP
Case 3. Elbow epicondylitis
A 25-year-old male worker presents with chronic left lateral epicondylitis. He is left handed, and his condition has failed to improve with conservative treatment. He has not undergone surgery. Examination shows mild painful crepitation in the left lateral epicondylar region. AROM of the left elbow is noted with extension 0°, flexion 130°, pronation 70°, and supination 80°. Radiography of the left elbow shows calcification of the lateral epicondylar region.
Solution A (FUPIRS by ROM) is as follows:
-
3/44 (Table 12) Extension 0° = 0% UE
-
3/44 (Table 12) Flexion 130° = 5% UE
-
3/45 (Table 13) Pronation 70°= 2% UE
-
3/45 (Table 13) Supination 80° = 0% UE = 7% UE
-
3/58 (Table 21) Convert UE to WP 7% UE = 4% WP
Solution B (FUPIRS by diagnosis) is as follows:
-
3/50 Impairment because of other disorders of the UE
-
3/50 (Table 18) Elbow proximal radioulnar maximum 20% UE X 3/51 joint crepitation 10% = 2% UE
-
3/58 (Table 21) Convert UE to WP 2% UE = 1% WP
Solution C (AMA Guides by ROM) is as follows:
-
3/40 (Figure 32) Extension 0° = 0% UE
-
3/40 (Figure 32) Flexion 130° = 1% UE
-
3/41 (Figure 35) Pronation 70° = 1% UE
-
3/41 (Figure 35) Supination 80° = 0% UE = 2% UE
-
3/20 (Table 3) Convert UE to WP 2% UE = 1% WP
Solution D (AMA Guides by diagnosis) is as follows:
-
3/58 Impairment because of other disorders of the UE
-
3/58 (Table 18) Elbow proximal radioulnar maximum 20% UE X 3/59 (Table 19) joint crepitation 10% = 2% UE
-
3/20 (Table 3) Convert UE to WP 2% UE = 1% WP
Case 4. Carpal tunnel syndrome
A 40-year-old right-handed woman presents after undergoing surgery in the right wrist for carpal tunnel syndrome. Examination shows normal motor strength with manual muscle testing of the right hand, including median nerve innervated muscles. Sensation is reduced, which interferes with activity of right median nerve distribution. EMG shows mild dropout of motor units with needle electrode findings in right abductor pollicis brevis, not first dorsal interosseous. Nerve-conduction study (shows mild slowing and right median sensory distal latency.
Solution A (FUPIRS by neurologic examination) is as follows:
-
5/84 Specific UE nerve
-
Median below mid forearm
-
Maximum for function from sensory deficit or pain = 40%
-
Maximum for function from motor/strength deficit = 35%
-
5/87 Determination of pain or loss of sensation - grade 3 = 16-30%
-
5/88 Determination of strength (power) and/or motor deficit - grade 2 = 1-40%
-
Therefore calculate as follows: Sensory loss 40% X 16-30% = 6-12% UE and motor loss 35% X 1-40% = 4-14% UE
-
15/189 Combine minimum 6% with 4% = 10% UE. Combine maximum 14% with 12% = 24% UE
-
3/58 (Table 21) Convert UE to WP 10-24% UE = 6-14% WP
Solution B (FUPIRS by diagnosis) is as follows:
-
5/85 Entrapment neuropathy table
-
Mild = 10% UE moderate = 25% UE
-
3/58 (Table 21) Convert UE to WP
-
For mild 10% UE = 6% WP
-
For moderate 25% UE = 15% WP
Solution C (AMA Guides by neurologic examination) is as follows:
-
3/54 (Table 15) Specific UE nerve
-
Median below mid forearm
-
Maximum for function because of sensory deficit or pain = 38%
-
Maximum for function because of motor/strength deficit = 10%
-
3/48 (Table 11) Determination of loss of sensation +/- pain or 4/151 (Table 20) Neurologic section for sensory loss or pain
-
Grade 3 = 26-60%
-
3/49 (Table 12) Determination of strength/power/motor deficit or 4/151 (Table 21) Neurologic section for strength deficit
-
Grade 4 = 1-25%
-
Therefore, calculate as follows: Sensory loss 38% X 26-60% = 10-22% UE and Motor loss 10% X 1-25% = 0-3% UE
-
P.322. Combine minimum 10% c/w 0% = 10% UE maximum 22% c/w 3% = 24% UE
-
3/20 (Table 3) Convert UE to WP 10-24% UE = 6-14% WP
Solution D (AMA Guides by diagnosis) is as follows:
-
3/57 (Table 16) Entrapment neuropathy
-
Mild = 10% UE moderate = 20% UE
-
3/20 (Table 3) Convert UE to WP
-
For mild 10% UE = 6% WP
-
For moderate 20% UE = 12% WP
Case 5. Hip degenerative joint disease
A 65-year-old man presents with moderate degenerative joint disease of the right hip after hip fracture. Examination shows mild antalgic gait, and the patient uses a cane for only outdoor ambulation. AROM of the right hip is normal, and the right leg is 1 in. shorter than left. Radiography shows moderate degenerative joint disease with a 3-mm cartilage interval for the right hip.
Solution A (FUPIRS by leg-length discrepancy) is as follows:
-
4/71 (Table 42) Leg 1 in. shorter 10% LE
-
4/71 (Table 42) Convert LE to WP 10% LE = 4% WP
Solution B (FUPIRS by diagnosis) is as follows:
-
4/69 Other disorders of hip, arthritis 10% LE
-
4/71 (Table 42) Convert LE to WP 10% LE = 4% WP
Solution C (AMA Guides by leg-length discrepancy) is as follows:
-
3/75 (Table 35) Leg 1 in. shorter 5% LE
-
3/75 Convert LE to WP 5% X 0.4 = 2% WP
Solution D (AMA Guides by gait derangement): 3/76 (Table 36) Mild category C 15% WP
Solution E (AMA Guides by diagnosis) is as follows:
-
3/83 (Table 62) Cartilage interval 3 mm 7% LE
-
3/75 Convert LE to WP 7% X 0.4 = 3% WP
Case 6. Hip bursitis
A 40-year-old woman presents with chronic bursitis of the greater trochanter of the right hip. Examination shows local tenderness with a trigger point at the right greater trochanter. Full active and passive ROM of the hip demonstrates pain reproduction on resisted abduction and an antalgic gait in the right LE if she walks longer than 30 minutes. The patient does not require the use of an assistive device.
Solution A (FUPIRS by ROM) - Impairment = 0% WP
Solution B (FUPIRS by diagnosis) is as follows:
-
2/28 Painful organic syndrome hip 4% LE
-
4/71 (Table 42) Convert LE to WP 4% LE = 2% WP
Solution C (AMA Guides by ROM or gait derangement - Impairment = 0% WP
Solution D (AMA Guides by diagnosis) is as follows:
-
3/85 (Table 64) Hip trochanteric bursitis 7% LE
-
3/75 Convert LE to WP 7% LE X 0.4 = 3% WP
Case 7. Knee-cartilage injury
A 25-year-old man presents with a tear of the medial meniscus tear in his right knee after partial medial meniscectomy. After rehabilitation, he continues to have knee pain, locking, swelling, and mild effusion. Examination shows that AROM of the right knee is 0° (full extension) to 130° flexion. Strength on manual muscle testing is grade 4/5 (extension/flexion) for the knee. Atrophy is 2 cm in the right calf and thigh compared with the left, and his gait is antalgic on the right leg. Radiographs show moderate degenerative changes of the right knee with a 3-mm cartilage interval.
Solution A (FUPIRS by ROM) is as follows:
-
4/68 (Table 35) 130° flex = 7% LE
-
4/71 (Table 42) Convert LE to WP 7% LE = 3% WP
Solution B (FUPIRS by diagnosis)
-
4/68 (Table 36) Other disorders of knee 5% LE arthritis
-
4/71 (Table 42) Convert LE to WP 5% LE = 2% WP
Solution C (AMA Guides by ROM) - 3/78 (Table 41) Not less than 110° flexion 0%
Solution D (AMA Guides by gait derangement) - 3/76 (Table 36) Mild Category A. 7% WP
Solution E (AMA Guides by atrophy) is as follows:
-
3/77 (Table 37) Mild/moderate category 8% LE
-
3/75 Convert LE to WP 8% X 0.4 = 3% WP
Solution F (AMA Guides by strength deficit) is as follows:
-
3/77 (Table 38-39) Grade 4 = 12% LE
-
3/75 Convert LE to WP 12% X 0.4 = 5% WP
Solution G (AMA Guides by diagnosis) is as follows:
-
3/85 (Table 64) Partial meniscectomy 2% LE
-
3/84 Combine with arthritis and ROM impairment if any (weakness and atrophy are combined in diagnosis-based estimates, ie, for meniscectomy).
-
3/83 (Table 62) 3-mm cartilage interval 3% LE
-
3/78 (Table 41) Not less than 110° flexion 0%
-
P. 322. Combine 3% LE with 2% LE = 5% LE
-
3/75 Convert LE to WP 5% LE X 0.4 = 2% WP
Case 8. Knee arthroplasty
A 62-year-old woman presents with a knee injury, aggravating severe degenerative joint disease of the left knee. Patient has undergone left total knee arthroplasty with no pain after surgery. She has stable anteroposterior and mediolateral motion. She has no flexion contracture, no extension lag, and normal alignment. Examination shows well-healed left knee surgical scar, mild effusion of left knee, and left knee AROM/passive ROM (PROM) of 0-100°. Patient can ambulate with routine use of cane but does not require a brace. Radiography shows left total knee arthroplasty.
Solution A (FUPIRS by ROM) is as follows:
-
4/68 (Table 35) Flexion 100° = 18% LE
-
4/71 (Table 42) Convert LE to WP 18% LE = 7% WP
Solution B (FUPIRS by diagnosis) is as follows:
-
4/68 (Table 36) Knee replacement arthroplasty 10-30% LE
-
4/71 (Table 42) Convert LE to WP 10-30% LE = 4-12% WP
Solution C (AMA Guides by ROM) is as follows:
-
3/78 (Table 41) Knee ROM impairment < 110° = 10% LE
-
3/75 Convert LE to WP 10% LE X 0.4 = 4% WP
Solution D (AMA Guides by gait derangement): 3/76 Table 36. Gait-Moderate category "e" 20% WP
Solution E (AMA Guides by diagnosis) is as follows:
-
3/88 (Table 66) Knee replacement results: a = 50 points; b = 20 points; c = 0 points; d = 0 points; e = 0 points; f = 0 points
-
a + b + c - (d + e + f) = 70 points
-
3/85 (Table 64) Knee replacement impairment
-
Fair result category 50% LE
-
3/75 Convert LE to WP 50% LE X 0.4 = 20% WP
Case 9. Reflex sympathetic dystrophy
A 45-year-old right-handed woman presents with history of severe stretch injury in the left brachial plexus. She as residual, severe reflex sympathetic dystrophy of her left arm, with causalgia and complex regional-pain syndrome. Examination shows an atrophic left arm and forearm with cold, clammy, dusky, shiny skin. No AROM is noted at the shoulder, elbow, wrist, or hand. PROM shows clinically significant guarding, but it is generally restricted. Contractures are noted in the shoulder, elbow, wrist, and hand, but the examiner cannot establish consistent measurements with a goniometer because of guarding. Pulses are +2 and equal for both radial and ulnar arteries.
No voluntary motion more than trace motion is noted in the patient's entire left UE. Sensation is noted in the left UE, with hyperpathia and allodynia. EMG and nerve-conduction studies are performed. EMG of the left arm shows decreased insertional activity and poor recruitment of motor units. Nerve-conduction study of the left arm is impossible of pain. Radiography shows evidence of osteopenia in the left arm.
Solution A (FUPIRS by diagnosis) is as follows:
-
2/29 Reflex sympathetic dystrophy UE 25% UE
-
Intro/6 Basic rule 2 subtract 10% for nonpreferred arm 25% UE - 2.5% UE = 22.5% UE = 23% UE
-
3/58 Convert UE to WP 23% UE = 24% WP
Solution B (AMA Guides by diagnosis) is as follows:
-
3/56 Causalgia and reflex sympathetic dystrophy 4 100% UE
-
3/18 (Figure 2) Impairment for amputation 100% UE = 60% WP or 3/20 (Table 3) Convert UE to WP 100% UE = 60% WP
Case 10. Lumbosacral strain
A 29-year-old man presents with chronic lumbosacral strain, no numbness or weakness of LEs, and no loss of bladder or bowel function. Examination shows spasms and rigidity on palpation in the lumbosacral paraspinal muscles. Restricted flexion-extension lumbosacral ROM is noted, but readings are inconsistent with those obtained with an inclinometer or goniometer. Neurologic examination of the lower extremity is normal, showing no weakness or atrophy. Deep tendon reflexes are normal with no sensory loss. Radiographic and MRI findings in the lumbosacral spine are normal.
Solution A (FUPIRS by diagnosis) is as follows:
-
1/12 Intervertebral disk or other soft tissue lesions
-
Lumbar spine = 3% WP
Solution B (AMA Guides by diagnosis) is as follows:
-
3/109 (Table 71) 1 Guarding/dysmetria is present.
-
3/102 diagnosis-related estimate (DRE) lumbosacral category II: minor impairment 5% WP
Case 11. Lumbosacral herniated nucleus pulposus with radiculopathy
A 45-year-old man with L4-5 herniated nucleus pulposus presents after single-level laminectomy, discectomy, and fusion surgery. His symptoms include continued back pain and sciatica of the right leg. Numbness noted in the L5 distribution of the right leg does not interfere with his function. Mild weakness of the right leg is noted, but the patient can ambulate without use of cane. He has difficulty sleeping because of pain when he lies supine.
Examination shows rigidity and a surgical scar over the lumbosacral region. AROM/PROM of the thoracolumbosacral spine in all planes are normal, though values on straight-leg raising and inclinometry are inconsistent. On straight-leg raising, positive findings are noted on the right side are in the when the patient is supine but not when he is seated. Strength of the right great toe and right ankle dorsiflexor is 4/5; no atrophy of the calf musculature is noted.
Testing of the deep tendon reflexes an absent right medial hamstrings reflex. Sensation is decreased to pain in the right L5 distribution. Gait analysis shows an antalgic pattern in the right leg. Presurgical radiography of the lumbosacral spine shows spondylosis at L4-L5. Presurgical MRI shows herniated nucleus pulposus at L4-5 on the right. After surgery, lumbosacral MRI shows evidence of gad fusion and scarring at L4-L5. EMG shows active right L5 radiculopathy before surgery and chronic, mild right L5 radiculopathy after surgery.
Solution A (FUPIRS) is as follows:
-
1/13 Intervertebral disk 5 lumbar 7% WP
-
1/13 Intervertebral disk 8 fusion add 1% WP
-
7% WP + 1% WP = 8% WP
-
5/85 Spinal nerve, LE L5 nerve root maximum loss sensory 5.0% maximum loss motor 37%
-
5/87 Grade 2 sensory loss 1-15% (use 15%)
-
5/88 Grade 2 motor 1-40% (use 30%)
-
Sensory 5% X 15% = 1.0% LE
-
Motor 37% X 30% = 11% LE
-
15/189 Combine 11% LE c/w 1% LE = 12% LE
-
4/71 (Table 42) Convert 12% LE = 5% WP
-
15/189 Combine 8% WP + 5 % WP = 13 % WP
Solution B (AMA Guides by DRE model): 3/110 (Table 72) DRE lumbosacral category III 10% WP
Solution C (AMA Guides by ROM model) (see 3/99) is as follows:
-
3/113 (Table 75) Disorder category II E 10% WP
-
3/130 (Table 83) Spinal nerve, LE L5 nerve root maximum loss sensory 5.0% maximum loss motor 37%
-
4/151 (Table 20) Class 2 sensory loss 1-25% (use 25%)
-
4/151 (Table 21) Grade 4 motor 1-25% (use 25%)
-
Sensory 5% X 25% = 1.0% LE
-
Motor 37% X 25% = 9.0% LE
-
P. 322. Combine 9.0% LE combine with 1.0% LE = 10% LE
-
3/75 Convert LE to WP 10% LE X 0.4 = 4.0% WP
-
P. 322 Combine 10% WP c/w 4.0% WP = 14% WP
-
3/99 ROM to DRE 14% WP closest to DRE lumbosacral category III
-
DRE lumbosacral Category III = 10% WP
No additional impairment is added for disturbed sleep because of pain or discomfort in supine position. No impairment is included for fusion with loss of ROM of the lumbosacral spine.
Example of Disability Evaluation
The following case study is from a FCE by using the NADEP protocols. The testing components of this particular example include intake patient screening, grip-strength testing, ROM and strength studies, and dynamic-lifting evaluation. These components were observed as May and Martelli outlined and emphasize the need for the examining physician to review all physiologic aspects, as well as the potential psychological response.
History taking
This history was collected during intake screening, the first component of the model.
The examinee had an open, grade 3C fracture left tibia due to a fall at work. He was immediately transported to a trauma center. He underwent irrigation and debridement of the left ankle and external fixation of the left distal tibia. He remained in the hospital for approximately 1 week. He stated that he was given instruction on how to use crutches before he was discharged. He was advised to return to his orthopedic physician for follow-up and treatment on a weekly basis. This schedule continued for approximately 4 months, and then he saw his orthopedic surgeon once a month.
During the 4-month period, he was hospitalize twice for additional surgery: repeat irrigation and debridement of the left tibial pilon fracture with closure of the ankle wounds took place and later open reduction internal fixation of the left distal tibia and irrigation and debridement of the medial ankle wound with removal of the external fixator.
The patient then began formal physical therapy and aquatic therapy. At present, he is continuing home aquatic therapy by using the pool at his local YMCA. He will next begin therapy to evaluate progress with his home program with a visit schedule of once a week.
The patient's medications are celecoxib (Celebrex) 100 mg bid and acetaminophen and hydrocodone (Lortab 500/7.5 mg). He states that he had no prior medical injuries or disabilities related to his work or personal life.
Additional information that is collected but not reported here included the patient's educational level, family history, support system, financial situation (ie, whether he receives disability income or whether he has no income [The amount is not important.]), and vocational history in the previous 15 years.
Patient profiling
The examiner administers the second component, patient profiling. At this point, the examiner learns how the patient is coping with his disability, how well he has adjusted to the disability period, if the patient is exaggerating symptoms, and if the individual is reporting systemic or localized profile.
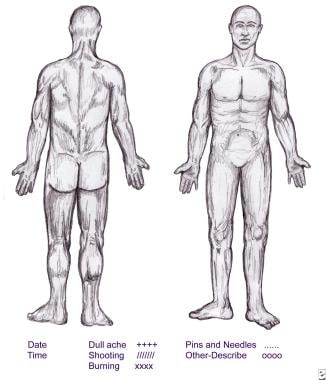
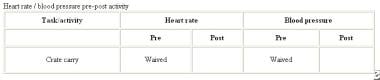
The patient completes a symptom chart (see the image below). This chart is specific to the injury and locations of any surgical incisions, and it presenting a localized profile.
The information is encouraging because it suggests that the patient has some control over his symptom-response patterns in response to daily activities and that no other anatomic locations are involved. The patient's rehabilitation potential may be good, but no opinion can be given confidently without a review of all profiling and functional data. Reviewing the form can help in identifying a possible trend.
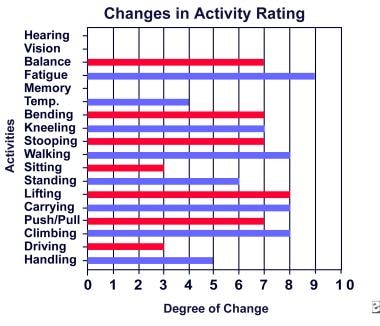
Changes in activity rating
The image below shows the changes in activity rating.
As much control as the symptom chart suggested, the patient's activities indicates a more substantial effect of his disability. The findings are this chart a notable, and suggest that the effect on his activities is directly related to the diagnosis. Had the patient described substantial changes in the first 2 senses (ie, hearing and vision), the examiner would flag this complaint as a possible sign of exaggeration of symptoms. One item that was not expected was the last one, material handling. This finding should alert the examiner to look for significant deficit profiling in the remaining test activities, as this item was not related to the affected area and/or diagnosis.
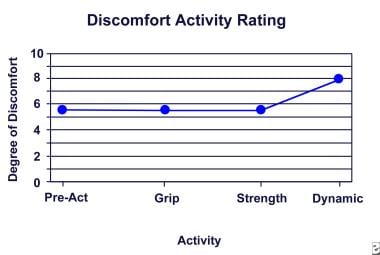
The image below graphically depicts the patient's symptomatic response to physical activities as he progresses through the evaluation process.
His pretest, resting discomfort levels are documented, and his performance and behavior are monitored from that point until the end of the last test item. The patient demonstrated some control and management of symptoms until he engaged in the dynamic lifting and carrying activities, which stressed his affected extremity the most.
Summary of history and patient profile
At this point, the patient's response to the activities, his ability to participate in the test activities, and his overall functional responses are summarized in the report.
The following text is quoted from page 6 of the report:
To summarize, Mr. [Examinee] demonstrated an ability to negotiate his symptoms, or an ability to manage and control his symptoms until functional activity was applied to his lower extremity. He exhibited mechanical/strength deficits in ROM and dynamic activities. Regarding the dynamic lifting study, he completed the WEST lifting evaluation but the crate carrying activity was waived due to his lower extremity weakness and mechanical dysfunction. Based on the medical records and the Examinee's performance on this functional study, it is this evaluator's opinion that the Examinee can function independently in the competitive labor market without accommodation at the LIGHT physical exertional demand level. He requires accommodation when functioning at the MEDIUM to HEAVY physical demand levels.
Additional questioning
At this point, the examiner is asked 4 questions:
Did the examinee complete all of the assigned activities?
Was the examinee consistent in all activities per the repeated measures testing protocol?
Did the examinee manage and control his symptoms adequately such that he could perform work independently in the competitive labor market?
What is the maximum physical demand level this individual can perform safely while maintaining acceptable production levels?
Grip-strength study
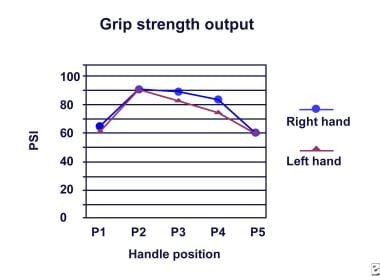
The next component is the grip-strength study. The graph below shows a good, symmetrical strength pattern between the right and left hands.
This component is not used to investigate strength output. Instead, this component helps the examiner obtain an impression of how the patient will perform during the rest of the examination. Will he or she be inconsistent? Will he or she display overt pain behaviors when engaged in activity? Will he or she complain of unrelated symptoms? In this case, the examiner can conclude that the patient had a good effort, given the symmetrical output of the patterns and that repeated measures were within acceptable variances.
ROM and systems review
The next component is the ROM and systems review and physical examination when the patient is measured for joint ROM and strength in the UEs and LEs. The patient undergoes thorough musculoskeletal and neurologic examination.
This examinee was tested for strength discrepancies between the affected and unaffected legs. Repeated measurements were collected to determine the reliability of data among trials. The images below show his strength output.
The patient's left LE, the affected extremity, constantly performed at a level below that of the right. His repeated demonstrated good reliability of effort between and among trials. Because no normative data exist, the examiner used this technique to determine the patient's consistency of performance and to document any notable strength deficits.
These images show how the tests were administered. In the NADEP model, these digital images are used in reports, for obvious reasons. Because forensic disability is being assessed, attorneys from both sides need to know what was done and how the data were collected.
Static-strength testing
Next is the static strength component, which was not performed in this case study. Because strength data were obtained in the ROM component, this one was waived.
Dynamic lifting
The final component is dynamic lifting. Domain testing was not administered because the examiner already had sufficient data to render an opinion on the patient's work capability. Therefore, work-simulation activities were not necessary.
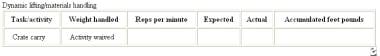
In the dynamic-lifting component, stationary lifting system (WEST Evaluation System) was used. Before dynamic study, the patient's lifting mechanics and his maximum lifting weight were determined by using the pretest lifting-evaluation protocol May and Martelli cited. [45] The patient was observed to compensate for his mechanical deficits (see the first image below). He holds his left leg higher than his right, suggesting that his weight-bearing capacity is greater on the right leg than on the left. The second and third images below show his maximum upper and lower lifting ranges. The examiner is looking for any compensatory mechanics on these images.
The image below shows the swelling in the left LE that the patient reported as being problematic in his functioning and overall symptom response.
The images below demonstrate the patient's cumulative lifting in terms of the weight carried in foot-pounds, as well as his heart rate and blood pressure before and after the test.
This information is crucial because it documents the patient's effort the in the lifting exercises and his vital-sign responses. For example, if the patient's heart rate does not increase and if he or she demonstrates substantial pain and response, the examiner suspect the person's overall effort in the test. The patient in this case demonstrated good effort.
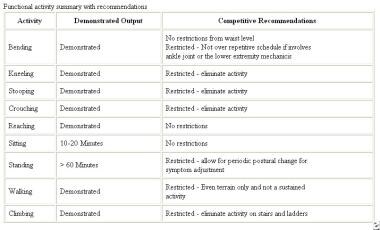
Summary
The images below show the method for summarizing the examinee's functional performance, including how his performance was documented and what competitive functional levels are recommended.
The bottom image shows a summary if his dynamic lifting/materials handling capabilities. In this case, the examinee was rated being as capable of performing lifting considered in the heavy category, but only with modifications to his work setting, specifically, to his vertical work plane.
Conclusion
Conclusions are summarized under the NADEP heading vocational implications. This section indicates the physical demand level or characteristic, as the US Department of Labor defines it. In this, case the rating for physical demand characteristic was awarded from the restricted and unrestricted vertical and/or horizontal work planes.
The final comments address workplace considerations. Here, the examiner outlines the specific physical activity restrictions, such as those applied to bending, kneeling, stooping, standing, walking, and climbing. The individual's likelihood of being placed in a suitable job and his or her overall likelihood of employment may be addressed as well.
The conclusion in this case is quoted below.
Vocational Implications:
Based on the US Department of Labor definitions for WORK and accompanying physical exertion demand levels, it is this examiner's conclusion that the examinee qualifies for the HEAVY work category within the restricted work plane, provided that the work criteria, as presented in Tables 1 and 2, are integrated into any return-to-work considerations. When considering the competitive unrestricted vertical and horizontal work planes, the examinee qualifies for the LIGHT work category.
Work Place Considerations:
Mr. Chenault manipulated weight at a level that qualifies him for the HEAVY physical demand characteristic under the Department of Labor definition of work. However, what this resistance level does not detail is his lack of tolerance and stability for moving this weight level from point "A" to point "B". His left lower extremity demonstrated significant atrophy when circumference measurements were taken and his strength patterns were significantly weaker than the right. Thus, while he can manipulate a maximum of 50 pounds from a standing position, this is not a true measure of work performance, or the ability to manipulate the weight in terms of carrying and stacking. Thus, it is highly recommended that Mr. Chenault be removed from activities that require repetitive kneeling, stooping, squatting/crouching, walking and climbing stairs and/or ladders.
This gentleman would benefit from an active job placement and development program at this time, as he should begin focusing on return-to-work options and strategies. I conclude that his returning to carpentry work or related fields with similar work demands is poor and guarded at best, regardless of physical rehabilitation efforts. He is a highly motivated individual and I strongly believe that he wants to become gainfully employed as soon as possible.
Thank you for allowing me to evaluate your patient.
Sincerely yours,
V. Robert May III, Rh.D., CDE II Certified Disability Examiner
Legal and Other Issues of Impairment Rating and Disability Evaluation
Questions
What is a PIR?
Case law discusses a PIR as an anatomic or functional abnormality or loss that a physician establishes and rates. (Escambia County Council on Aging v Goldsmith, 500 So2d 626 [1st DCA 1987]). Judges and courts throughout the nation have generally accepted this definition.
In the worker's-compensation system in Florida, as in many other states, impairment ratings determine specific benefits the claimant can receive. For example, a 7% PIR may mean that the claimant receives benefits for 7 weeks. The Florida Supreme Court has upheld the fact that benefits are tied to impairment ratings and not disability (Bradley v Hurricane Restaurant, 670 So2d 162 [Fla 1996]).
What can be rated?
The PIR can originate only from a compensable injury (Murphy v NE Drywall, 692 SO2d 918 [1997]).
Who can typically give PIRs?
Medical doctors, osteopathic physicians, chiropractic physicians, optometrists, dentists, and psychologists can make PIRs. Some states, such as Florida, restrict the medical specialists who may assign ratings.
Can the impairment rating include subjective evidence?
Yes. Ratings are usually based on objective and subjective information. Subjective complaints include pain, numbness, and depression. The practitioner cannot ignore these complaints when determining an impairment rating.
The best example of the use of scientific evidence is found in the case of Daubert v Merrell Dow Pharmaceuticals, Inc, 509 US 579 (1993), which demonstrated that certain factors may bear on the judge's determination about the admissibility of scientific data. Considerations included (1) whether a "theory or technique can be (and has been) tested"; (2) whether it "has been subjected to peer review and publication"; (3) whether, in respect to a particular technique, the "known or potential rate of error" is high and whether "standards controlling the technique's operation" are established; and (4) whether the theory or technique enjoys "general acceptance" within a "relevant scientific community" (509 US at 592-594). The Federal Rules of Evidence, as well as many state courts, have adopted this decision.
The US Supreme Court extended the Daubert philosophy to nonmedical experts (Kumho Tire Company, LTD, et al, Petitioners v Patrick Carmichael et al, 526 US 137 [1999]). The fact that a practitioner assigns an impairment rating does not mean that it is admissible. The rating must be scientifically based and must rely on a disability guide with a proven record.
When should the patient be rated?
The impairment rating should occur at MMI, the point at which further recovery from or lasting improvement too an injury or disease can no longer be anticipated on the basis of reasonable medical probability. The PIR is given when the claimant has an injury (Murphy v NE Drywall, 692 SO2d 918 [1997]).
When should a PIR be documented?
The examiner should not wait rating until after completing all reports to document an impairment. By then, it may be too late.
A court decision precluded an expert from testifying about to PIR on the witness stand (Auto Owners Insurance Co and Roberts v Clark, 676 So2d 3 [4th DCA 96]). In this case, the court held that the neurosurgeon could not give testimony regarding an impairment rating because his observations would have been based on a treatment session after the cutoff date for discovery. This ruling is intended to prevent 1 party from having an unfair advantage of surprise over the other.
For example the defense team hires an examiner who renders a report, the plaintiff prepares for the hearing on the basis of the contents of the report. If the examiner arrives at trial and changes his or her diagnosis, the judge may strike all of the testimony as being inconsistent with the initial report if the examiner's testimony is a surprise and if it was developed after the cutoff date for discovery.
Is the test scientific in a forensic environment?
In a forensic environment, when FCEs are frequently used, scientific nature of the test may be questioned.
The decision of the United States Supreme Court in Daubert v Merrell Dow Pharmaceuticals, Inc, 509 US 579 [1993] and progeny, in conjunction with Federal Rule of Evidence 702, define the Court's gatekeeping function in relation to the admissibility of proposed scientific and other expert testimony.
Rule 702 states, "If scientific, technical, or other specialized knowledge will assist the trier of fact to understand the evidence or to determine a fact in issue, a witness qualified as an expert by knowledge, skill, experience, training, or education, may testify thereto in the form of an opinion or otherwise, if (1) the testimony is based on sufficient facts or data, (2) the testimony is the product of reliable principles and methods, and (3) the witness has applied the principles and methods reliably to the facts of the case."
Under Rule 702, a district court must first determine whether the proposed testimony will "assist the trier of fact." If the answer to is affirmative, the court must consider whether the proffering expert is qualified by "knowledge, skill, experience, training, or education" to render an opinion on the particular subject. If the expert is so qualified, the district court must finally determine whether the expert's opinions are "reliable" under the factors enunciated in Daubert and Kumho Tire Co, Ltd. v Carmichael, 526 US 137 [1999].
Tests of reliability and validity in the forensic environment
Blankenship method
The Blankenship method suggests that, if movements are not reproducible in an acceptable coefficient of variants, they are not reliable.
Examples of situations that might reflect incorrect invalidity are the following:
-
The patient is obese.
-
The patient is out of shape and/or has pulmonary problems.
-
The patient has psychiatric problems.
-
The patient does not understand the instructions.
-
The patient's sex may affect the results.
Heart rate/blood pressure method
The theory underlying the heart rate/blood pressure method of determining an examinee's effort is this: If the person's blood pressure is elevated, his or her effort is valid.
Examples of situations that may result in inappropriate invalid findings are as follows:
-
The patient has oily skin or sweats profusely. (These observations are used to determine that the person's heart rate may be unstable.)
-
The patient has cardiac abnormalities.
-
The patient has psychiatric problems.
-
The patient does not understand the instructions.
-
The patient is taking medications that affect his or her blood pressure.
Research suggests that patients with chronic back disabilities may have more dysfunctional coping mechanisms, pain avoidance, depression and self-reported disability than do other individuals. Psychosocial variables strongly related to test performance, and therefore FCE findings, may not be "necessary or valid in assessing the physical performance of this population of chronic pain patients." [46]
Duration and extrapolation of FCE results
FCE should take 4 hours to 1 week to perform, and an occupational or physical therapist should perform the examination. [47]
How are results of 2-4 hours extrapolated to a 40-hour work week? Those who report FCE results in a forensic environment must be prepared to answer the following questions:
-
How was the validity of your FCE determined?
-
What is the minimum number of validity criteria?
-
Were they met in this case?
-
Who performed the evaluation and recorded the data?
-
Did someone help the claimant fill out the paperwork?
-
Can the claimant read? If so, does he or she read English or any other language?
-
How do you know if the claimant can read or not?
-
Did you prescreen the claimant for cardiac restrictions?
-
What medication did the claimant take, or what medication was the claimant taking, and how can it affect the test results? (Examples are medications to treat cardiac problems and Xanax, which affects concentration and energy levels)
-
How was the coefficient of variances determined? Do other organizations or professionals use different numbers? Why?
-
Why are your numbers more valid than numbers others might report?
-
Which extrapolation method was used? (Examples: Snook, Blankenship, Dictionary of Occupational Titles [DOT])
-
How many participants were in the control group of the study that determined the validity of this research?
-
What research supports the assertion that reproducible results that are inconsistent an arbitrarily established coefficient of variance, or range, means that the study is invalid and that the patient is showing a lack of effort?
-
Did the results exclude the claimant from sedentary, light, medium, or heavy duty?
-
Did the results squarely fit within the DOT's definitions of sedentary, light, medium, or heavy duty?
-
How long did the test take?
-
If the test is unquestionably not reproducible, would you not agree the claimant can still have a valid medical condition resulting in impaired function?
Conclusion
Controversy surrounds the use of the aforementioned tests. If it is used in a forensic environment, one can assume there the legal community may pose difficult and probing questions about the test chosen and the science behind it. The practitioner must fully understand how the test was developed and be prepared to discuss the science supporting its validity scales and extrapolation methods.
Psychiatric Issues of Impairment Rating and Disability Evaluation
Determination of a permanent rating for a psychiatric impairment presents complications. For example, in Florida, a psychologist cannot issue a PIR.
Minnesota Multiphasic Personality Inventory
The more information that is obtained about an examinee's condition, the more grounded the impairment rating. For example, a psychological evaluation based on the Minnesota Multiphasic Personality Inventory (MMPI) is appropriate in many cases. This 570-question test has a built in F scale to compensate for exaggerating, a feature that can lend credibility to a diagnosis. This test is widely accepted by psychiatrists and psychologists and commonly used throughout the nation. However, caution is urged to ensure that only individuals who meet the requirements of National Computer Systems and the University of Minnesota administer the test.
The MMPI is not the sole factor used in arriving at a diagnosis. This tool must be taken into account along with the results of a clinical interview. In fact, a PIR should not be rendered without a clinical interview. The American Psychiatric Association (APA) code of ethics specifically requires a clinical interview or an attempt to interview the patient before an opinion is rendered.
Diagnostic and Statistical Manual, Fourth Edition
The most commonly accepted treatise or book on how to determine the nature of a psychiatric illness is the Diagnostic and Statistical Manual, Fourth Edition (DSM-IV). This book is divided into sections based on diagnoses and the criteria for such diagnosis. The presentation is straightforward and serves to assist the nonmedical professional to verify that the psychiatrist or psychologist followed the proper steps before making a diagnosis.
Multiaxial psychiatric evaluation
The psychiatric evaluation should be performed in a multiaxial format, as indicated below. The DSM-IV also suggests this format, as do the AMA Guides. Furthermore, the figure in the introduction to the mental issues chapter represents this format. A multiaxial evaluation contains references for 5 axes the practitioner addresses, a follows:
-
Axis 1: The psychiatric diagnosis is major depression. What is the patient's actual condition in psychiatric terms?
-
Axis 2: The patient is diagnosed as suffering from a personality disorder (eg, obsessive compulsive personality disorder). By definition, a personality disorder develops in late adolescence or early adulthood and cannot develop spontaneously. An individual with a personality disorder has significant functional impairment or significant stress secondary to that disorder. By definition, personality disorders are serious, not mild. This axis applies only to personality disorders. By saying "none," the professional is indicating here that the patient had no preexisting personality disorder.
-
Axis 3: This axis for low back pain represents physical problems or conditions suffered by the patient (eg, glaucoma, cancer, stomach problems). Diagnosis of these conditions is important because many physical problems can cause psychiatric problems. For example, hypothyroidism can cause depression, as can many medications given for other disorders. This axis explains that the physical problems exist, so any part they may play in the psychiatric diagnosis must be addressed.
-
Axis 4: This divorce axis represents psychosocial stressors (eg, loss of a child, problems with primary support group, occupational problems, economic problems, law suits).
-
Axis 5: The axis for global assessment functioning (GAF) represents the GAF scale from 0-100 referred to on page 32 of the DSM-IV. A patient functioning in the 90-100 range has few, if any, psychiatric symptoms. Someone functioning in the l0-20 range probably should be hospitalized because of the threat they represent to themselves and others. A score of 45 means the patient has serious symptoms, significant functional impairment, and even may be suicidal. NOTE: This rating number can change throughout the course of treatment and frequently does.
Many psychiatrists may not follow this format and simply evaluate a patient and render a diagnosis. This type of assessment is less desirable and has less scientific basis than the multiaxial format. If a multiaxial format is followed, comparing and contrasting the reports of psychiatrists become much easier. The multiaxial format also encourages consistency, which can legitimize the approach to assessment.
Assessment of symptoms
The PIR must be based on a complete report that discusses specific symptoms of psychiatric illness. The most common indications include the following:
-
Change in weight
-
Desire to commit suicide
-
Anhedonia (ie, pervasive lack of interest in things, feeling BLAH, not wanting to do anything fun)
-
Feelings of guilt or worthlessness
-
Psychomotor agitation or retardation (eg, talking and moving very quickly as expected with psychomotor agitation or very slowly in psychomotor retardation)
-
Somatic symptoms (ie, physical symptoms actually caused by psychiatric distress, such as chest pain, heart palpitations, headaches, stomach aches, bowel problems)
-
Difficulty concentrating
The evaluation can be incomplete if the patient was not asked about these symptoms or if such questions were not discussed. Most patients do not know what information is being collected unless the doctor is direct. A 15-minute interview during which the psychiatrist asks the patient if he or she is depressed is wholly insufficient for initial diagnosis. The examiner should establish rapport with the patient, observe his or her body language, and review the medical history.
Ancillary tests
Ancillary tests, such as those previously mentioned, also are recommended. These tests are most commonly administered by psychologists, who then provide the results to the psychiatrist for treatment. If possible, enlist the cooperation of outside individuals (eg, employer, spouse, friend). A review of the information supporting other medical diagnoses is also important.
If traumatic brain injury (TBI) is suspected, information about the examinee's premorbid functioning is important and may be extracted from school records. If the patient's psychiatric condition is expected to improve with treatment, the patient has not reached MMI.
One common pitfall with doctors that defense attorneys frequently hire is that they tend to make improper diagnoses. Often, a psychiatrist or psychologist diagnoses a personality disorder to explain psychiatric symptoms and soften the blow for the defense because a personality disorder, by definition, predates an accident. Therefore, although the patient may have an impairment rating, the rating may not due to the accident or injury. Some plaintiff-oriented doctors may ignore the symptoms of personality disorders and attribute an injury on psychopathology.
Evidence of personality disorder may include poor grades, failure to develop important interpersonal relationships, repeated problems with the law or authority, a failure to hold steady jobs, and being defined by the environment.
If the practitioner is unsure if a diagnosis is appropriate, the diagnostic tree contained in the DSM-IV (page 689) may be helpful. This appendix is useful in ruling out other diagnoses. By answering the questions, the examiner reaches the ultimate diagnosis. An attorney who is preparing to cross-examine the practitioner may also find this diagnostic tree helpful.
Sample Deposition Questions on Impairment Rating and Disability Evaluation
Sample disposition questions to ask during the impairment rating and disability evaluation are shown below.
Which disability/impairment guide was used and why?
What is the examiner's training and expertise on impairment rating?
Which extraneous factors were taken into consideration for the impairment rating?
Was the persons' intelligence quotient (IQ) considered in the physical impairment rating?
Was IQ considered in the mental impairment rating?
Was vocational dysfunction considered in the impairment rating?
How many ROM studies were performed in each joint plane?
Was the spinal muscle spasm graded?
Is the examiner familiar with the entire AMA Guides or just with the section used for rating?
In rendering orthopedic/spinal impairment rating, did the examiner also consider the neurologic section for determining impairment rating?
Did the examiner consider chronic pain syndrome or other associated mental disorders when determining the overall impairment rating?
Did the examiner consider the effect of lack of sleep and concentration in the overall impairment rating?
Did the examiner determine whether or not there was any urologic or sexual dysfunction caused by the injury and was it rated?
If the examiner became aware that the claimant's function was far greater than claimed, would the impairment rating be adjusted?
If there were a prior impairment rating for a similar condition, what impact would it have on the impairment rating for the present accident?
If there are physical and mental impairments, are the ratings added or combined? (Impairment ratings associated with mental disorders are combined with physical impairments to determine a person's overall impairment. These values are combined by using the combined-value chart, rather than simply added, to determine the overall impairment. A combined-values chart is used when more than 1 impairment rating for different diagnoses [eg, limb, organ, system] are determined. Values are added, rather than combined, only when multiple range-of-motion ROM measurements are considered for a single joint.)
Does the final impairment rating include consideration of whether the impairment rating is likely to worsen over time?
At what point was the impairment rating assigned?
What factors would cause the examiner to reevaluate this impairment rating?
Is the impairment rating secondary to the accident under consideration or to some other cause?
Is it not true that a patient can have significant impairment with no vocational disability?
Is it not true that a patient can have minimal or no impairment with significant vocational disability?
What is the scientific basis for the impairment guide used?
Did the patient ever ask the examiner to increase the impairment rating?
Is it not true that an impairment rating may be appropriate even without the patient's having sustained injury in an accident?
Is it not true that the guides give no impairment rating for chronic pain?
Please apportion the impairment rating based on the preexisting degenerative condition versus the injury caused by aggravation following the accident.
What effect does personality disorder have on the impairment rating?
What are the objective findings that support the impairment rating?
What are the subjective findings that the support the impairment rating?
-
Work Evaluation System Technology (WEST) schematic.
-
Symptom-discomfort chart.
-
Changes in activity rating.
-
Discomfort activity rating.
-
Functional-activity summary and recommendations.
-
Materials handling and lifting table.
-
Grip strength graph.
-
Ankle strength. Dorsiflexion.
-
Ankle strength. Plantar flexion.
-
Dorsiflexion test. Image courtesy of Bob May, MD.
-
Plantar flexion test. Image courtesy of Bob May, MD.
-
Compensatory mechanics. Lower lift. Image courtesy of Bob May, MD.
-
Maximum lift, upper range. Image courtesy of Bob May, MD.
-
Maximum lift, lower range. Image courtesy of Bob May, MD.
-
Edema in the left leg. Image courtesy of Bob May, MD.
-
Dynamic lifting results table.
-
Heart rate and blood pressure table.
Tables
What would you like to print?
- Introduction to Impairment and Disability Evaluation
- Concepts in Disability Evaluation
- Impairment Rating Guides
- Impairment Rating Examples
- Example of Disability Evaluation
- Legal and Other Issues of Impairment Rating and Disability Evaluation
- Psychiatric Issues of Impairment Rating and Disability Evaluation
- Sample Deposition Questions on Impairment Rating and Disability Evaluation
- Show All
- Media Gallery
- Tables
- References