Practice Essentials
Central cord syndrome (CCS), an acute cervical spinal cord injury (SCI), was initially described by Schneider and colleagues in 1954. It is marked by a disproportionately greater impairment of motor function in the upper extremities than in the lower ones, as well as by bladder dysfunction and a variable amount of sensory loss below the injury level. [1, 2, 3, 4, 5, 6] Magnetic resonance imaging (MRI), computed tomography (CT) scanning, and the production of plain radiographs of the cervical spine can facilitate the diagnosis of central cord syndrome. [7] The focus of physical therapy in CCS is the preservation of range of motion (ROM) and the enhancement of mobility skills. [8]
Although CCS has been reported to occur with particular frequency among older persons with cervical spondylosis who sustain hyperextension injury, it can be found in persons of any age and can be associated with various etiologies, injury mechanisms, and predisposing factors. [2] CCS, the pathophysiology of which appears in the image below, is the most common incomplete SCI syndrome.
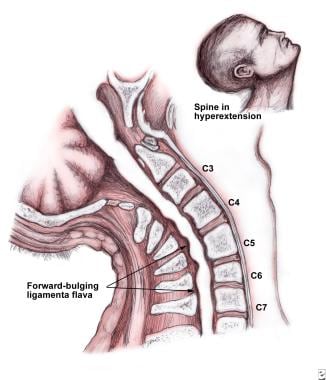 Illustration of the pathophysiology of central cord syndrome. Note the "pincer" effect on the central cord by anterior and posterior compression.
Illustration of the pathophysiology of central cord syndrome. Note the "pincer" effect on the central cord by anterior and posterior compression.
Signs and symptoms of central cord syndrome
Symptoms of central cord syndrome (CCS) occur following trauma (most commonly falls) and consist of upper and lower extremity weakness, with varying degrees of sensory loss.
Pain and temperature sensations, as well as the sensation of light touch and of position sense, may be impaired below the level of injury. Neck pain and urinary retention are common.
Workup in central cord syndrome
Imaging studies in central cord syndrome (CCS) include the following [7] :
-
Plain radiography - Radiographic films of the cervical spine delineate fractures and dislocations, as well as the degree and extent of spondylotic changes
-
Computed tomography (CT) scanning - CT scanning of the cervical spine shows spinal canal compromise and allows the indirect approximation of the degree of spinal cord impingement
-
Magnetic resonance imaging (MRI) - MRI demonstrates direct evidence of spinal cord impingement from bone, a disc, or a hematoma [9]
Management of central cord syndrome
Physical therapy
The focus of physical therapy in central cord syndrome (CCS) is the preservation of range of motion (ROM) and the enhancement of mobility skills. [8] The strengthening of any preserved lower extremity musculature is essential, as are trunk balance and stabilization.
Occupational therapy
Given the predominance of upper extremity weakness that occurs in CCS, the restoration of the basic activities of daily living (ADLs), upper extremity strength, and ROM are the main goals of occupational therapy.
Speech therapy
A speech therapist should be involved in the treatment of patients with CCS who have dysphagia from the head position maintained by cervical orthoses or as a result of anterior cervical spine fusion.
Recreational therapy
The primary goal of recreational therapy is to help patients with CCS return to preinjury areas of interest.
Surgery
Surgery is rarely indicated in CCS, because of the inherently favorable prognosis for patients with the condition. However, surgical intervention should be considered when progress becomes inconsistent after an initial period of improvement, when compression of the spinal cord persists, when gross spinal instability is present, and when neurologic deficits progress. [10, 11, 12, 13]
Pathophysiology
Central cord syndrome (CCS) most often occurs after a hyperextension injury in an individual with long-standing cervical spondylosis. (See also the Medscape Reference article Cervical Spondylosis.) Injury may result from posterior pinching of the cord by a buckled ligamentum flavum or from anterior compression of the cord by osteophytes. [14] Historically, spinal cord damage was believed to originate from concussion or contusion of the cord with stasis of axoplasmic flow, causing edematous injury rather than destructive hematomyelia. Autopsy studies subsequently demonstrated that CCS may be caused by bleeding into the central part of the cord, portending a less favorable prognosis. Studies have also shown that CCS probably is associated with axonal disruption in the lateral columns at the level of the injury to the spinal cord, with relative preservation of the grey matter.
The syndrome also may be associated with fracture dislocation and compression fracture, especially in a congenitally narrowed spinal canal. [10] These anteroposterior compressive forces also distribute the greatest damaging effect on the central mass of the cord substance.
CCS-related motor impairment results from the pattern of lamination of the corticospinal and spinothalamic tracts in the spinal cord. Sacral segments are the most lateral, with lumbar, thoracic, and cervical components arranged somatotopically, proceeding medially toward the central canal.
Epidemiology
Frequency
United States
The prevalence rate of central cord syndrome is 15.7-25%.
International
In a retrospective French study, by Ronzi et al, of 63 patients hospitalized for traumatic SCI associated with cervical spinal canal stenosis (without spinal instability), 78.6% of subjects were found to have a clinical syndrome, with central cord syndrome being the second most common, after Brown-Séquard–plus syndrome. [15]
Mortality/Morbidity
Central cord syndrome is generally associated with a favorable prognosis for the achievement of some degree of neurologic and functional recovery. [1, 16, 17, 18]
Sex
Similar to all other SCIs, central cord syndrome predominantly affects males. [18]
Age
Central cord syndrome (CCS) has a bimodal distribution; in young persons, CCS tends to result from trauma, while in older individuals, it is typically caused by falls sustained by persons with preexisting spondylosis. [16, 19]
-
Illustration of the pathophysiology of central cord syndrome. Note the "pincer" effect on the central cord by anterior and posterior compression.








