Practice Essentials
Tendon ruptures of the biceps brachii, one of the dominant muscles of the arm, have been reported in the United States with increasing frequency. Ruptures can occur at the proximal or distal biceps tendon, with 90-97% of tears involving the proximal biceps tendon. [1, 2]
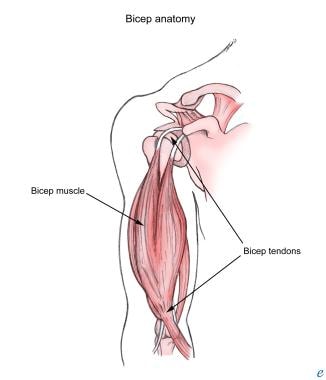
Anatomy
At its proximal attachment, the biceps has two distinct tendinous insertions on the scapula from its long and short heads. The short head arises from the coracoid process with the coracobrachialis, while the long head originates from the supraglenoid tubercle and passes over the humeral head within the capsule of the glenohumeral joint (see image below).
The biceps muscle then continues down the arm within the intertubercular groove, covered by a synovial outpouching of the joint capsule. The two muscle bellies unite near the midshaft of the humerus and attach distally on the radial tuberosity. The distal tendon blends with the bicipital aponeurosis, which affords protection to structures of the cubital fossa, allowing distribution of forces across the elbow to lessen the pull on the radial tuberosity. [3, 4] The biceps receives innervation via the musculocutaneous nerve (C5, C6) from the lateral cord of the brachial plexus.
Diagnosis and management of biceps rupture
In most cases, proximal or distal biceps tendon ruptures can be detected on the basis of history and physical examination alone. Physical examination may show the classic "Popeye" muscle bulge of the humerus midshaft with a complete biceps tendon rupture. However, several imaging studies can be employed as an extension of the physical examination to rule out other disorders from the lengthy list of possibilities; these include plain radiography, arthrography, ultrasonography, and magnetic resonance imaging (MRI).
Depending on the individual case scenario, the type of facility, and physician preference, patients who have suffered a rupture of the biceps tendon can benefit from physical and/or occupational therapy. Rest the affected joint in the acute stage, with or without soft immobilization. Control swelling with cold modalities (eg, cold packs, ice massage, hydrotherapy, specialized cold compression units) and treat inflammation with nonsteroidal anti-inflammatory drugs (NSAIDs), barring contraindications. Early evaluation and treatment by occupational therapy resemble strategies used in rotator cuff repairs. Current recommendations advise, for most patients, an initial course of conservative (nonoperative) management for proximal biceps tendon tears. Should the patient fail conservative management, surgical options need to be considered. In distal biceps tendon tears, most patients proceed to surgical management. [1]
Several reviews of surgical repair versus conservative (nonoperative) management report conflicting results. Generally accepted clinical guidelines advocate surgical repair consisting of tenodesis and subacromial decompression proximally (or anatomic reattachment distally) for young or athletic patients or for persons who require maximum supination strength. [5, 6] Cosmetic concerns may prompt a surgical approach when appearance is unacceptable to the patient following rupture. [7, 8, 9, 10]
Pathophysiology
The biceps muscle and its tendons are some of the most superficial structures of the arm. These structures account for a significant portion of shoulder injuries and a smaller number of elbow injuries. Ruptures of the proximal biceps tendon make up 90-97% of all biceps ruptures and almost exclusively involve the long head. [11] Proximal tendon ruptures occur at the tendon-labral junction or bony attachment and are typically not associated with a unique mechanism. Distal biceps tendon tears occur at the radial tuberosity and are commonly linked to an excessive eccentric overload. [2]
Shoulder pathology, specifically symptomatic rotator cuff tears, has been reported in 46-82% of patients with proximal biceps tendon pathology. [1]
Epidemiology
Frequency
United States
As previously noted, biceps ruptures have been reported in the United States with increasing frequency.
Mortality/morbidity
Overall consequences of biceps rupture may differ among various demographic groups. The major impairment resulting from proximal biceps rupture involves limitations due to pain during the acute phase, but impairment ultimately relates to a decrease in strength during shoulder flexion, elbow flexion, and forearm supination. Distal ruptures also initially result in pain, followed by reduced strength in supination, elbow flexion, and grip strength. [5]
Race
No correlation exists between race and the incidence of biceps rupture.
Sex
Men suffer biceps rupture more commonly than do women, but this difference may result primarily from vocational or avocational factors. The dominant arm is involved more commonly, probably because it is used more often. At present, no evidence exists for a male or female predisposition to biceps rupture due to anatomic or genetic factors.
Age
Age in biceps rupture may vary considerably, depending on the location of the rupture. Distal biceps tears typically happen between the ages of 35-54 years and have a strong male predominance (95%). [12, 2] In contrast, proximal biceps tendon tears commonly occur in the elderly.
-
Biceps muscle and tendons