Practice Essentials
Piriformis syndrome, caused by a neuritis of the proximal sciatic nerve, results from compression or irritation of the sciatic nerve by the piriformis muscle due to spasm and/or contracture, with patients characteristically suffering hip and buttock pain. There is no definitive method to accurately diagnose piriformis syndrome, but treatment with a home stretching program is among the therapies that should be provided to the patient. [1, 2]
A controversial diagnosis since its initial description in 1928, piriformis syndrome, which can mimic a diskogenic sciatica, is also referred to as pseudosciatica, wallet sciatica, and hip socket neuropathy.
In many musculoskeletal practices, piriformis syndrome can be considered a reasonable primary or secondary diagnosis if the symptoms, history, and physical examination are supportive. Due to the traumatic etiology of most cases, however, piriformis syndrome usually is associated with other, more proximal causes of low back pain, sciatica, or buttock pain (thereby further clouding the diagnosis).
Piriformis syndrome signs and symptoms
These include the following:
-
Piriformis muscle spasm often is detected by careful, deep palpation
-
The reproduction of sciatica-type pain with weakness results from resisted abduction/external rotation (Pace test) [3]
-
The Freiberg test is another diagnostic sign that elicits pain, upon forced internal rotation of the extended thigh [4]
-
The Beatty maneuver reproduces buttock pain by selectively contracting the piriformis muscle [5]
-
A painful point may be present at the lateral margin of the sacrum
-
Shortening of the involved lower extremity may be seen
-
The patient may have difficulty sitting due to an intolerance of weight bearing on the buttock
-
The patient may have the tendency to demonstrate a splayed foot on the involved side when in the supine position
Piriformis syndrome workup
Diagnostic imaging of the lumbar spine may be helpful in excluding associated diskogenic and/or osteoarthritic contributing pathology should conservative treatment of clinically diagnosed piriformis syndrome fail to provide therapeutic benefit. Diagnostic ultrasonographic imaging of the piriformis muscle for the assessment of muscle morphology has demonstrated a significant correlation of piriformis muscle morphology abnormality.
Piriformis syndrome management
Because there is no definitive method to accurately diagnose piriformis syndrome, treatment regimens are controversial and have not been subjected to randomized, blind clinical trials.
In most cases, conservative treatment (eg, stretching, manual techniques, injections, activity modifications, natural healing, modalities such as heat and ultrasound) is successful in managing the condition.
Consider the use of ultrasound and other heat modalities prior to physical therapy sessions. Before piriformis stretches are performed, the hip joint capsule should be mobilized anteriorly and posteriorly to allow for more effective stretching. Soft-tissue therapies for the piriformis muscle can be helpful, including longitudinal gliding with passive internal hip rotation, as well as transverse gliding and sustained longitudinal release with the patient lying on his/her side. Addressing sacroiliac joint and low back dysfunction also is important.
A home stretching program should be provided to the patient. These stretches are an essential component of the treatment program.
Surgical management is the treatment of last resort for piriformis syndrome. Surgery for this condition involves resection of the muscle itself or of the muscle tendon near its insertion at the superior aspect of the greater trochanter of the femur (as described by Mizuguchi). [6]
Pathophysiology
The piriformis muscle is flat, pyramid-shaped, and oblique. [7] This muscle originates to the anterior of the S2-S4 vertebrae, the sacrotuberous ligament, and the upper margin of the greater sciatic foramen. Passing through the greater sciatic notch, the muscle inserts on the superior surface of the greater trochanter of the femur. With the hip extended, the piriformis muscle is the primary external rotator; however, with the hip flexed, the muscle becomes a hip abductor. Branches from the L5, S1, and S2 nerve roots innervate the piriformis muscle, as demonstrated in the image below. Due to this innervation, a lower lumbar radiculopathy may cause secondary irritation of the piriformis muscle, which may complicate diagnosis and hinder patient progress.
A cadaver study by Iwanaga et al indicated that the superior gluteal nerve is another important source of piriformis muscle innervation. Of 20 sides from 10 cadavers studied, the investigators found that in 80%, the piriformis muscle was innervated by 2-3 nerves. Nerves originated from the superior gluteal nerve on 14 sides (70%); from the inferior gluteal nerve on one side (5%); from the L5 ventral ramus on one side (5%); from the S1 ventral ramus on 17 sides (85%); and from the S2 ventral ramus on 14 sides (70%). [8]
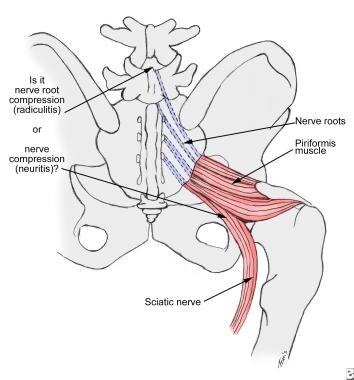 Nerve irritation in the herniated disk occurs at the root (sciatic radiculitis). In piriformis syndrome, the irritation extends to the full thickness of the nerve (sciatic neuritis).
Nerve irritation in the herniated disk occurs at the root (sciatic radiculitis). In piriformis syndrome, the irritation extends to the full thickness of the nerve (sciatic neuritis).
Many developmental variations of the relationship between the sciatic nerve in the pelvis and piriformis muscle have been observed. [9, 10, 11] In approximately 20% of the population, the muscle belly is split, with 1 or more parts of the sciatic nerve dividing the muscle belly itself. In 10% of the population, the tibial/peroneal divisions are not enclosed in a common sheath. Usually, the peroneal portion splits the piriformis muscle belly, although in rare cases, the tibial division does so.
In a study of 200 pairs of sacral roots (100 patients, none of whom had piriformis syndrome) by Russell et al, T1-weighted magnetic resonance imaging (MRI) scans revealed that 199 of the S1 nerve roots (99.5%) were positioned above the piriformis muscle, while 150 of the S2 nerve roots (75%) traversed the muscle and 50 of them (25%) were located above it. The images also showed that 194 S3 nerve roots (97%) traversed the muscle and that 190 S4 nerve roots (95%) were below it. The piriformis muscles had an average size of 1.9 cm; in 19% of the study's patients, the muscle was asymmetrical by more than 3 mm. [12]
Involvement of the superior gluteal nerve usually is not seen in cases of piriformis syndrome. This nerve leaves the sciatic nerve trunk and passes through the canal above the piriformis muscle.
Blunt injury may cause hematoma formation and subsequent scarring between the sciatic nerve and short external rotators. Nerve injury can occur with prolonged pressure on the nerve or vasa nervorum.
The etiology of piriformis syndrome can be divided into the following categories:
-
Hyperlordosis
-
Muscle anomalies with hypertrophy
-
Fibrosis (due to trauma)
-
Partial or total nerve anatomical abnormalities
Other causes can include the following:
-
Pseudoaneurysms of the inferior gluteal artery adjacent to the piriformis syndrome
-
Bilateral piriformis syndrome due to prolonged sitting during an extended neurosurgical procedure
-
Total hip arthroplasty
-
Vigorous physical activity
-
Leg length discrepancy [13]
Piriformis syndrome remains controversial because, in most cases, the diagnosis is clinical, and no confirmatory tests exist to support the clinical findings.
Papadopoulos and colleagues proposed the following classifications for piriformis syndrome [14] :
-
Primary piriformis syndrome - This designation would apply to piriformis syndrome resulting from intrinsic pathology of the piriformis muscle itself, such as myofascial pain, anatomic variations, and myositis ossificans.
-
Secondary piriformis syndrome (pelvic outlet syndrome) - This classification would encompass all other etiologies of piriformis syndrome, with the exclusion of lumbar spinal pathology.
In an imaging study of 74 patients who demonstrated pathologies associated with piriformis syndrome, Vassalou et al found a greater incidence of secondary causes than primary etiologies, with the condition most often caused by space-occupying lesions in the piriformis area. The study, which employed magnetic resonance imaging (MRI) and/or computed tomography (CT) scanning, reported the most frequent imaging finding to be piriformis muscle enlargement. [15]
Epidemiology
Frequency
United States
Given the lack of agreement on exactly how to diagnose piriformis syndrome, estimates of the frequency of sciatica caused by piriformis syndrome vary from rare to approximately 6% of sciatica cases seen in a general family practice. [3] More than 80% of adults have had at least 1 episode of disabling low back pain (LBP) in their lifetime. [16]
Mortality/Morbidity
Piriformis syndrome is not life-threatening, but it can have significant associated morbidity. The total cost of low back pain and sciatica is significant, exceeding $16 billion annually in direct and indirect costs.
Sex
Some reports suggest a 6:1 female-to-male ratio for piriformis syndrome.
-
Nerve irritation in the herniated disk occurs at the root (sciatic radiculitis). In piriformis syndrome, the irritation extends to the full thickness of the nerve (sciatic neuritis).








