Practice Essentials
The prepatellar bursa is a superficial bursa with a thin synovial lining located between the skin and the patella. In cadaveric studies, a trilaminar prepatellar bursa was found in 78-93% of people, and a bilaminar bursa was found in 7-22% cases. [1] Normally, the prepatellar bursa does not communicate with the joint space and contains a minimal amount of fluid; when it becomes inflamed, however, there is a marked increase of fluid within its space. It is clinically very important in prepatellar bursitis to differentiate between chronic nonseptic bursitis (NSB) and acute septic bursitis (SB). [2, 3]
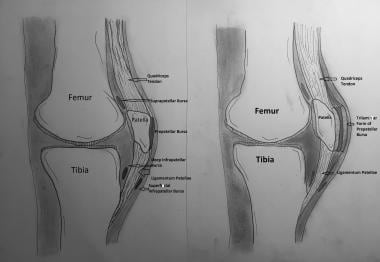
Prepatellar bursitis is historically called "housemaid's knee," although it is also known as "coal miner’s knee" [4] and "carpet layer’s knee." [5] In the literature, the earliest reference to the condition and its management occurred in 1861. [6] (See the image below.)
Signs and symptoms of prepatellar bursitis
The physician may note any of the following signs and symptoms during physical examination:
-
Tenderness of the patella to palpation
-
Fluctuant edema over the lower pole of the patella
-
Erythema of the knee
-
Crepitation of the knee
-
Decreased knee flexion secondary to pain
Workup in prepatellar bursitis
Laboratory studies are not usually indicated to diagnose prepatellar bursitis. However, aspiration of prepatellar bursa fluid may be indicated to differentiate NSB from SB. Evaluate the aspirated fluid for white blood cell (WBC) count, protein, lactate, glucose, crystals, and Gram stain results.
Plain radiographs may show soft tissue swelling; however, radiographs are necessary only if other conditions are suggested (eg, fracture and/or dislocation).
Computed tomography (CT) scanning and magnetic resonance imaging (MRI) are reserved for cases that have been difficult to manage (eg, failure of initial treatment for septic prepatellar bursitis). [7, 8] Ultrasonography may be a useful technique for evaluating synovial fluid in the knee.
Management of prepatellar bursitis
Conservative Management:
Conservative management consists of protection, rest, ice, compression, and elevation (PRICE); nonsteroidal anti-inflammatory drugs (NSAIDs); and bursal aspiration. Intrabursal steroid injection may be indicated for the treatment of chronic NSB. For acute SB, antibiotic therapy is the key treatment and should be started as soon as infection is suspected after the bursal fluid aspiration. Transient immobilization of the knee in the neutral position with a posterior splint may be needed in cases of acute prepatellar SB. [9]
Physical therapy
After the initial period of rest, the goal of physical therapy is to regain any loss of range of motion (ROM) while increasing the flexibility of the quadriceps and hamstrings. Use of therapeutic modalities can be helpful to assist stretching in this period.
Occupational therapy
The role of the occupational therapist in this scenario is to address modifications of activities in patients diagnosed with prepatellar bursitis secondary to overuse. Emphasize patient education, avoidance of kneeling, and use of kneepads if kneeling is necessary.
Surgical intervention:
Incision and drainage of the prepatellar bursa usually is performed when symptoms of acute SB have not improved significantly within 36-48 hours of antibiotic administration. Surgical removal of the bursa (ie, bursectomy) may be necessary for chronic or recurrent prepatellar bursitis. [10] Arthroscopic or endoscopic excision of the bursa has been reported to have satisfactory results, with less trauma than open excision. [11, 12]
Pathophysiology
The prepatellar bursa is a flat, round, synovial-lined structure; its main function is to separate the patella from the patellar tendon and skin. This bursa is superficial, suggesting that it is undeveloped at birth. Within the first few months to years of life, the bursa arises from direct pressure and friction. It reduces friction between the skin and the patella and allows maximal range of motion (ROM).
Nonseptic bursitis
Nonseptic bursitis (NSB) is a sterile inflammation that develops secondary to occupational or athletic trauma, crystal deposition (gout, pseudogout), or systemic disease, such as rheumatoid arthritis, systemic lupus erythematosus, systemic sclerosis, [13] or uremia. Most cases of NSB result from chronic microtrauma caused by repetitive friction. Particularly vulnerable are individuals continually exposed to compressive and sheer forces between the skin and the patella bone, including members of occupational groups whose job requires frequent kneeling or crawling (eg, carpenters, gardeners, roofers) and athletes participating in sports such as ice hockey, volleyball, and wrestling. The inflammatory response causes an overproduction of bursal fluid and subsequent bursal swelling, resulting in NSB. [14, 15]
Septic bursitis
Septic bursitis (SB) results from infection of the bursal sac, which is frequently caused by skin lesions but can also arise from secondary spread of infection from initial cellulitis into a pretraumatized superficial bursa or, in rare cases, from hematogenous seeding. Infection is commonly caused by bacteria (most often Staphylococcus aureus) but can in rare cases result from fungi. [16] The prepatellar bursa is the bursa most commonly involved in Brucella infection. [17, 18, 19] In addition, tuberculosis of the patella may present as prepatellar bursitis. [20]
Up to 50% of all SB cases occur in immunocompromised patients. Other risk factors include chronic rheumatic inflammatory diseases.
Hemorrhagic bursitis
Hemobursa is a rare cause of acute prepatellar bursitis, except in cases of trauma or anticoagulation.
Epidemiology
Frequency
Prepatellar bursitis is the second most common superficial bursitis after olecranon bursitis.
Mortality/Morbidity
Mortality associated with prepatellar bursitis is rare. Morbidity usually is secondary to pain and limited function. [21] In the case of septic prepatellar bursitis, failure to diagnose in a timely manner may lead to increased morbidity secondary to infectious etiology.
Sex
Prepatellar bursitis is more common in males than females.
Age
Prepatellar bursitis can affect all age groups; however, in the pediatric age group, it is likely to be septic and to develop in an immunocompromised host.
Prognosis
The prognosis in prepatellar bursitis is generally good with prompt diagnosis and treatment.
-
Prepatellar bursa in normal (left) and inflamed (right) state; trilaminar form.