Background
The lips have important functional and aesthetic roles in daily living. [1] They are the focal point of the lower face, with several aesthetic units intricately controlled by a complex series of muscles. Several key factors make reconstruction of the lip especially challenging. The lack of any substantial fibrous framework increases the risk of anatomic distortion through wound contraction and, hence, leads to poor functional and aesthetic outcomes. The quality (ie, color, texture, elasticity) of the skin and mucosa of the lips are difficult to match with distant flaps. Hence, local tissues provide the best results. However, with larger oncologic resections and more extensive traumas, an appropriate donor site might be difficult find. This is further complicated by the lack of any satisfactory prosthesis in aid of reconstruction.
Goals of reconstruction
Lip reconstruction is driven by restoration or preservation of function and aesthetics. [2, 3]
Functional considerations include oral continence, mobility that allows for sound formation and facial expression, adequate oral access, and sensation. Oral continence is critical in the ingestion of food and the confinement of salivary fluids within the oral cavity. The lips are also essential in forming many sounds, especially those of B, F, M, P, and V. Though microstomia may become an unavoidable adverse effect in some cases of lip reconstruction, it may cause functional impairment and should be avoided when possible. Furthermore, preservation of sensation is preferred both socially and functionally, as insensate lips are more prone to repeat injury.
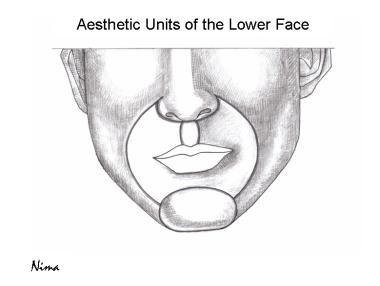
Aesthetic considerations include appropriate symmetry and normal anatomic proportions, presence of a philtrum, normal oral commissures, and establishment of a vermilion-cutaneous white border. The image below illustrates the aesthetic units of the lower face.
History of the Procedure
The first evidence of lip reconstruction is seen as far back as 3000 BC in Hindu writings, as well as in the Sanskrit writings of Susruta in 1000 BC. Many modern techniques are newer renditions of methods first described by Dieffenbach, Sabatini, Abbe, and Estlander in the 19th century. [4, 5, 6, 7, 8, 9] In 1834, Dieffenbach first described the check advancement flap technique based on an inferior-lateral pedicle. In 1838, Sabattini first described the cross-lip flap transfer of a lower lip midline wedge to a philtral defect. [6] This technique was modified and further popularized by Abbe and Estlander toward the end of the century.
To this day, the Abbe-Sabattini flap is commonly used in philtral reconstruction. Bernard [10] and von Burow [11] later described a bilateral full-thickness triangular cheek advancement flap that allowed for correction of total and subtotal lip defects. In the 1920s, Gillies described a fan flap technique using full-thickness pedicles; however, these flaps were denervated and did not allow for functional restoration.
Karapandzic improved on this technique with an oral circumference advancement flap with preservation of underlying musculature and neurovascular structures. [12] Most recent techniques incorporate principles that attempt to maximize both functional and aesthetic outcomes.
Epidemiology
Frequency
The frequency with which a reconstructive surgeon encounters the need for lip reconstruction is related to social and environmental issues of the practice setting. Since the most common causes of lip loss are trauma and oncologic resection, frequency is greater in trauma-related and oncologic practices. Earlier detection and attention to tumors, knowledge of sun protection, and better passenger protection in motor vehicle accidents have lessened the overall frequency of major lip reconstruction. The frequency of congenital deformities and major lip loss from gunshot injuries have not changed significantly.
Etiology
Oncologic excision, trauma, and congenital deformities are the major etiologies that require lip reconstruction.
More than 80% of cancers of the lip are of the squamous cell carcinoma type, perhaps due to tobacco use or anatomic exposure to solar radiation. Less commonly, adenocarcinomas and mucoepidermoid tumors can be found. Cancer of the lip is considered a readily visualized cancer and, as such, has a relatively lower mortality rate than other head and neck cancers. In the past 25 years, the incidence of lip cancer has decreased dramatically, and new surgical and medical treatments have contributed to a nearly 38% decrease in mortality. However, the functional and aesthetic ramifications of local wide excision of cancer of the lip make reconstruction of the lip imperative to the complete treatment and restoration of health and functioning.
The lower lip is most commonly affected by squamous cell carcinoma, whereas most basal cell carcinomas affect the upper lip. Based on the type of cancer, the excisional margin size may be smaller, with squamous cell carcinomas requiring larger margins than basal cell carcinomas.
Traumatic lesions of the lip are also common etiologies requiring reconstructive surgery. Frequently, gunshot wounds or motor vehicle accidents result in defects that affect functioning and aesthetic appearance of the lips. These injuries often require total or subtotal repair. Congenital defects such as cleft lip, vascular malformations, fistulae, and nevi frequently require lip reconstruction. These defects are not discussed in this article.
Pathophysiology
The tumor biology of cutaneous malignancy is relevant to the pathophysiology of much of lip reconstruction. This is discussed in Medscape Reference article Head and Neck Cutaneous Squamous Cell Carcinoma. Other relevant pathophysiology is scar contracture, which is discussed in Medscape Reference article Skin Wound Healing.
Presentation
Patients usually present for lip reconstruction immediately following lip loss. In oncologic lesions and hemangioma resections, the reconstruction is usually performed under the same anesthetic or after a short period needed for confirmation of completeness of cancer resection. In trauma, the reconstruction is also performed immediately after presentation or when the management of associated injuries allows anesthesia with maximum safety and when bacteriologic control of the wound is achieved. A short delay of a few days poses no particular barrier to successful reconstructions. However, long delays with wounds left open to heal by contraction and scar deposition substantially complicate subsequent reconstruction.
Indications
Indications for lip reconstruction are straightforward: they are the presence of a significant defect and available donor tissues. Contraindications arise when local control of the tumor cannot be achieved, which is a relatively rare occurrence. Unavailability of donor tissue generally does not prevent reconstruction but changes the technique to procedures that are more complex, that use donor tissue with less satisfactory properties, and that produce outcomes of lesser quality. Because many of the reconstructions can be performed under local or regional anesthetic, contraindications from systemic conditions such as advanced cardiopulmonary disease are rare.
Relevant Anatomy
Superficial anatomy
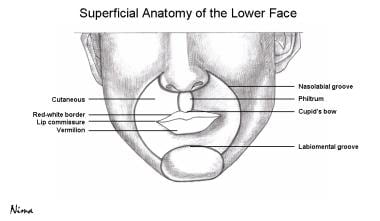
The lower third of the face is dominated by the lips, which can be further divided into 3 components: cutaneous, vermilion, and mucosal (see image below).The cross-sectional anatomy of the lips consists of the epidermal, dermal, subcutaneous, muscular (orbicularis oris), submucosal, and mucosal layers. Neurovascular, lymphatic, and glandular structures mainly run between the muscular and submucosal layers. At the vermilion, a rich neural and vascular plexus lies beneath a layer of specialized squamous epithelium, making the vermilion highly sensate and giving it its characteristic red appearance.
The red-white vermilion-cutaneous border is best defined in the upper lip, creating a shape referred to as Cupid's bow, the center of which is contributed by the philtral ridges and groove. Though the lower lip does not have as well defined a central groove, many individuals have a minor central notch. The dry vermilion transitions into the wet vermilion, which, in turn, has a smooth transition into the mucosa of the internal lips.
Perioral surface anatomy, including the nasolabial and labiomental grooves, as well as individual-specific shadows and tension lines, is important in the design of flaps with imperceptible incisions.
Muscular anatomy
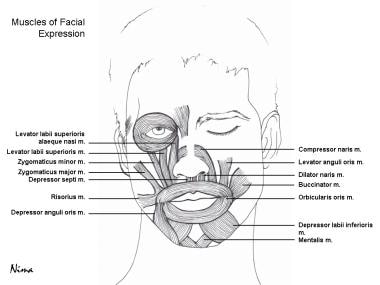
Relevant muscular anatomy along with origins, insertions, neural innervation, and action is summarized in Table 1 below and is illustrated in the image below.
Table 1. Muscles of Facial Expression (Open Table in a new window)
Muscle |
Origin |
Insertion |
Nerve |
Action |
Elevators |
|
|
|
|
Levator labii superioris |
Above and medial to the infraorbital foramen |
Skin and muscle of upper lip |
Buccal branch of facial nerve (VII) |
Elevates and everts upper lip |
Levator labii superioris alaeque nasi |
Frontal process of maxilla |
Skin of lateral nostril and upper lip |
Buccal branch of facial nerve (VII) |
Elevates upper lip and dilates nostril |
Levator anguli oris |
Canine fossa of maxilla below infraorbital foramen |
Outer end of upper lip and modiolus |
Buccal branch of facial nerve (VII) |
Elevates angle of mouth medially |
Zygomaticus major |
Zygomatic arch |
Modiolus at angle of the mouth |
Buccal branch of facial nerve (VII) |
Elevates and draws laterally the angle of the mouth |
Zygomaticus minor |
Lateral infraorbital margin |
Lateral skin and muscle of upper lip |
Buccal branch of facial nerve (VII) |
Elevates and everts upper lip |
Depressors |
|
|
|
|
Depressor labii inferioris |
Mandible below mental foramen along oblique line |
Orbicularis oris and skin of lower lip |
Mandibular branch of facial nerve (VII) |
Depresses and laterally draws lower lip |
Depressor anguli oris |
Oblique line of mandible |
Modiolus at angle of the mouth |
Mandibular branch of facial nerve (VII) |
Depresses and laterally draws angle of the mouth |
Miscellaneous |
|
|
|
|
Risorius |
Fascia over masseter |
Modiolus and skin at angle of the mouth |
Buccal branch of facial nerve (VII) |
Retracts angle of the mouth |
Buccinator |
… |
… |
Buccal branch of facial nerve (VII) |
… |
Mentalis |
Incisive fossa do mandible |
Skin of chin |
Mandibular branch of facial nerve (VII) |
Elevates and protrudes lower lip |
Neural anatomy
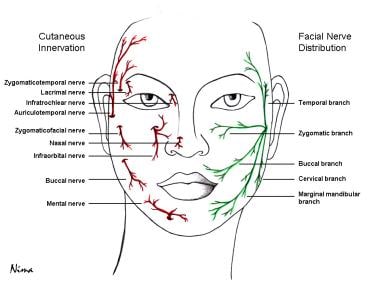
The motor innervation to the muscular anatomy is summarized in Table 1 above. The trigeminal nerve provides sensory innervation to the skin of the face. The maxillary division innervates the face below the level of the eyes and above the upper lip as the zygomaticotemporal, zygomaticofacial, and infraorbital nerves. The mandibular division innervates the face below the level of the lower lip via the buccal, auriculotemporal, and mental nerves. Refer to the image below for cutaneous innervation of the face and distribution of the facial nerve.
Vascular anatomy
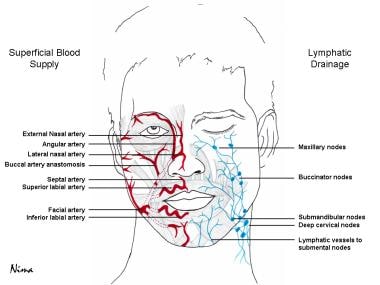
The main vascular supply to the lips comes from branches of the facial artery. The superior and inferior labial arteries supply the upper and lower lip respectively. The arteries originate deep to orbicularis oris and depressor anguli oris, and form a vascular ring around the mouth penetrating the orbicularis oris near the angle of the mouth and continue to run between the muscle and mucous membrane. Here, they communicate with the septal artery near the philtral ridges. The facial artery also gives rise to lateral nasal and angular arteries. The facial artery runs deep to the zygomaticus and levator labii superioris muscles, at which point it branches into the angular artery, which is embedded in the labii superioris, and then continues as the lateral nasal artery. Venous supply of the face runs with named arteries. Being familiar with the vascular supply around the lips allows for appropriate flap selection and preservation of neurovascular pedicles. See the image below.
Lymphatic anatomy
The lymphatic drainage of the lower face and lips plays a critical role in the spread of melanoma and squamous cell carcinoma. Both superficial and deep vessels of the central part of the lower lip drain to the submental lymph nodes, which, in turn, are drained by the submandibular and deep cervical lymph nodes. The upper lip, cheeks, side of the nose, and lateral portions of the lower lip are drained by the submandibular nodes. See the image above.
See Lips and Perioral Region Anatomy for more information.
-
Aesthetic units of the face.
-
Superficial anatomy of the lower face.
-
Muscular anatomy of the face.
-
Cutaneous innervation of the face and facial nerve distribution.
-
Blood supply and lymphatic drainage of the face.
-
Wedge excision and primary closure.
-
Abbe flap technique.
-
Estlander flap technique.
-
Gillies fan flap technique.
-
Karapandzic flap technique.
-
Bernard-Burow flap technique.
-
A and B. Central upper lip defect reconstruction with the perialar skin crescent method that retains motor and sensory innervation to the advanced upper lip lateral elements and uses an Abbe flap for philtral reconstruction. Used with permission of WB Saunders Company.
-
Bilateral depressor anguli oris total lower lip reconstruction. A. Flap design shows the relationships of the incision, muscle, motor nerve (VII), and sensory nerve (V). B. Flap transposition reorients the depressor anguli oris to restore the lower lip oral sphincter. Vermilion is created by mucosal advancement. C. Flap insert and direct donor defect closure complete the reconstruction.
-
von Bruns nasolabial flap technique.
-
A and B. Lip reconstruction. Bilateral orbicularis oris composite flap reconstruction of a large central upper defect. The aesthetic qualities of this reconstruction are enhanced by an Abbe flap philtral reconstruction.
-
A bilateral levator anguli oris flap total upper lip reconstruction. A. Flap design shows the relationship of the incisions, muscle, and lower lip Abbe flap for philtral reconstruction. B. Flap transposition reorients the muscles to become the upper lip sphincter. Motor (buccal) and sensory (infraorbital) nerves entering the lateral flap border are carefully preserved in dissection and transfer. Mucosal advancement restores vermilion and an Abbe flap restores the philtrum. C. Donor defect is closed directly and the Abbe flap pedicle is divided at 2 weeks.
-
Left: A patient with midline and left lateral lesions each occupying less than one third of the lower lip. Right: Wedge excision of the lesions.
-
Left: W-closure with bilateral advancement flaps of midline defect along with mucosal advancement flap of left lateral defect. Right: Postoperative follow-up showing excellent aesthetic results.
-
Left: Excision of large lesion occupying greater than 85% of the upper lip. Center: Selection of regional temporal interpolated flap based on the temporal artery. In this case, significant involvement of the cheek as well as compromised vasculature secondary to Mohs surgery did not allow for an advancement flap such as the Karapandzic flap. Right: Postoperative follow-up showing good aesthetic reconstruction of the ala of the nose, upper and lateral lip, and cheek.
-
Left: A patient with a midline upper lip lesion. Right: Reconstruction of medium to large upper lip defect with a modified unilateral Karapandzic flap. The nasal defect was closed with an internal mucosal advancement flap, a cartilage graft from concha of the ear, and a paramedian forehead flap for external reconstruction.
-
Left: Mohs surgical excision of the upper lip lesion affecting the left ala of the nose and leaving a defect occupying approximately 50-60% of the upper lip. Right: Postoperative follow-up showing good aesthetic reconstruction of the left ala of the nose and upper lip.
-
Left: Superficial lower lip cancer. Center: Resection of cancer with margins including the entire segment of the dry and major segment of the wet portion of the lower lip. Right: Vermilion advancement flap after dissection intraorally to the gingivobuccal sulcus.
-
Left: Small lower left lip lesion. Center: Excision and primary closure. Right: Postoperative results.
-
Left: Full-thickness left upper lip defect. Center: Medial advancement of the upper lip along subunits lines leading to the final scar being placed along the philtral column of the upper lip. Right: Postoperative results.
-
Left: Near midline small upper lip defect. Right: Burow wedge excision with primary closure (A-to-T flap).
-
Upper left: Left upper lip defect (< 1/3). Upper right: Medial advancement of the upper lip along subunits lines, leading to the final scar being placed along the philtral column of the upper lip. Lower left: Early postoperative follow-up. Lower right: Late postoperative follow-up.
-
Left: Right upper lip defect (~1/3). Right: Primary closure of defect.