Facial Injuries
One of the most vulnerable and important parts of the human body is the face. Typically, the face is considered to be bounded superiorly and laterally by the hairline and ears and inferiorly by the lower edge of the jaw. The most common mechanisms for facial injury are motor vehicle accidents, domestic accidents, work-related accidents, violence, and sports. The causes vary in association with age, sex, race, socioeconomic status, and geographic location. [1, 2, 3, 4, 5] Sports-related facial injuries account for 8% of all facial soft tissue injuries, with approximately 11-40% of all sports injuries involving the face. Injuries are most often due to direct hits with a ball or player-to-player contact. [6, 7] In younger age groups, sports accidents have risen due to increases in free time, the popularity of sports, and the introduction to more dangerous sports (eg, mixed martial arts). [3] Health care providers for athletes should be familiar with the anatomy of the facial region, the most common types of facial injuries, how to assess for injuries, the initial management of facial injuries, and protective equipment and education for players.
The most common types of sports-related facial trauma are soft tissue injuries and fractures of the nose, zygoma, and mandible, as well as dentoalveolar trauma; [8, 9, 10] these injuries often occur in combination. Depending on the extent and type of trauma, some injuries can be managed at the sporting event site, with the athlete resuming play immediately. Other injuries may demand transfer to an urgent care setting and management by a specialist.
A study by MacIsaac et al examined the incidence, causes, and demographics of nonfatal, sports-related craniofacial fractures in pediatric patients presenting to the emergency department of a Pittsburgh children’s hospital between 2000 and 2005. The incidence of sports-related injuries was greatest in children aged 13-15 years, accounting for 40.7% of the study’s 167 injuries. Baseball and softball were associated with the highest incidence of craniofacial fractures (44.3%), while basketball and football were associated with 7.2% and 3.0% of such injuries, respectively. Fractures most often resulted in connection with throwing, catching, or hitting a ball (34.1% of cases) and from collision between players (24.5% of cases). The incidences of specific fractures were as follows [11] :
-
Nasal: 35.9%
-
Orbital: 33.5%
-
Skull: 30.5%
-
Maxillary: 12.6%
-
Mandibular: 7.2%
-
Zygomaticomaxillary complex: 4.2%
-
Naso-orbitoethmoid complex: 1.2%
A Dutch study suggested that a relationship exists between specific sports and the type of associated maxillofacial fractures. In the study, of 108 patients (128 sports-related maxillofacial fractures), only soccer players suffered coronoid process fractures, while mandibular angle fractures tended to occur more often in rugby players. [12]
In a study of female athletes aged 5-24 years, using the National Electronic Injury Surveillance System, Kim et al found that sports-related craniofacial injuries most commonly occurred between the ages of 10 and 19 years. Among all of the females in the study, the majority of craniofacial injuries were related to softball (34.9%), basketball (28.1%), and soccer (15.6%), with contusions, abrasions, and lacerations being the most frequent presenting craniofacial traumas. [5]
Proper initial assessment and management of facial injuries may prevent unfavorable long-term results and permanent facial deformities. The ultimate goals are for the athletes to recover functionally and aesthetically from the facial injury and to return to competition in a timely manner.
For patient education resources, see the Back, Ribs, Neck, and Head Center; Breaks, Fractures, and Dislocations Center; Eye and Vision Center; and Teeth and Mouth Center, as well as Broken Nose, Facial Fracture, Black Eye, and Eye Injuries.
Basic Anatomy of the Face
The soft tissues
The soft tissues of the face are among the most vascular tissues of the body. Their blood supply is derived from contributions of both the external and internal carotid arteries. Because of the abundant blood supply to these tissues, ischemic tissue flaps and infections are uncommon. The underlying facial muscles account for the tension lines and rhytides of the skin. These skin tension lines become more prominent with age and with loss of skin elasticity and should be observed during the repair of soft tissue injuries to avoid unnatural scarring.
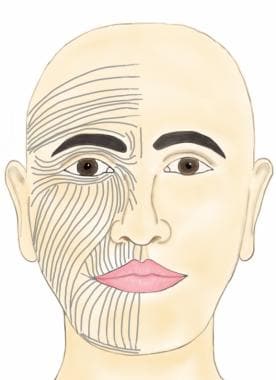 Skin tension lines of the face. An incision or a wound parallel to these lines results in better cosmesis. The directions of the skin tension lines are perpendicular to the underlying facial muscle orientation.
Skin tension lines of the face. An incision or a wound parallel to these lines results in better cosmesis. The directions of the skin tension lines are perpendicular to the underlying facial muscle orientation.
Contained within the facial soft tissues are adipose tissue, motor and sensory nerves, arteries, veins, lymphatics, the lacrimal system, and the parotid gland and duct. The sensibility of the face is supplied mainly by the three branches of the trigeminal nerve (ophthalmic [V1], maxillary [V2], mandibular [V3]). The muscles of mastication that control the opening and closing of the jaw are also innervated by the motor division of the trigeminal nerve. The muscles of facial expression are innervated by the five branches of the facial nerve (frontal/temporal, zygomatic, buccal, marginal mandibular, cervical). The lacrimal system is located in the medial eye region, and the parotid gland is located in the preauricular cheek region, with the parotid duct traveling through the buccinator muscle and entering the oral cavity through a papilla in the buccal mucosa opposite the second maxillary molar. The course of the parotid duct generally follows a line drawn from the tragus to the midportion of the upper lip.
See the images below.
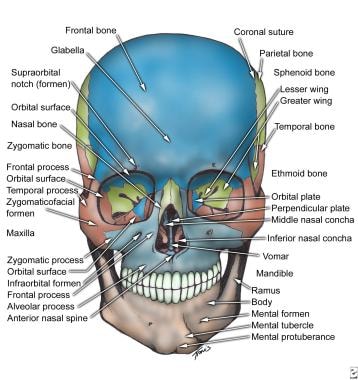
The facial bones
The facial skeleton is composed of a series of horizontal and vertical bony buttresses that support the architecture of the face against internal and external applied forces. The facial buttresses are designed to withstand forceful impacts in order to protect the underlying vital elements, such as the brain, the eyes, and other neurovascular structures.
The facial skeleton can be divided into thirds. The upper third consists of the frontal bone and ends at the level of the supraorbital ridge. Fractures in this area involve the frontal bone, frontal sinus, or orbital roof.
The middle third of the face is the most prominent and complex. It extends from below the supraorbital rims to the incisal edges of the upper teeth. This region consists of the orbits, the nasal bones, the zygoma, and the maxillary bones. The cone-shaped orbital space is composed of 7 bones: frontal, zygomatic, sphenoid, lacrimal, maxillary, palatine, and ethmoid. The periorbital bony rim serves as an attachment for the suspensory ligaments of the eye and the protective framework of the globe and optic nerve. The zygoma, along with the maxilla, gives the malar projection of the midface anteriorly. Laterally, it articulates with the temporal bone to form the zygomatic arch. The nose projects from the midface and is composed of both cartilage and bone to give it its characteristic shape. The midface experiences the highest incidences of fracturing because of its increased projection from the face.
The lower third of the face is the mandible and the teeth it supports. The condylar processes are considered a part of the lower third, even though they articulate with the temporal bone to form the temporomandibular joint.
Evaluation of Facial Injury
Initial evaluation of sports-related facial injuries should follow the Advanced Trauma Life Support (ATLS) principles of trauma evaluation and should begin with airway, breathing, circulation, and disability. A thorough history should be obtained from the patient, which should include previous facial injuries. During the primary evaluation, the athlete’s cervical spine should be immobilized until adequately assessed and cleared.
After the initial assessment and stabilization, the facial examination is then performed in a systematic manner, with particular attention paid to important bony landmarks, neurovascular structures, and soft tissues.
Universal precautions
Because of the marked vascularity of the face, many facial injuries involve blood and other secretions. Although the risk of disease transmission from contact between blood and intact skin is minimal, universal precautions must be followed whenever possible. When contact with blood or body fluids is likely, gloves, eyewear, and gowns represent standard protective equipment and should be used. Moreover, medical personnel who render care must strive to establish a clean area for treatment in the midst of the contaminated environment associated with a sports arena.
Airway
Patients with sports-related facial injuries are usually able to maintain protective oral and pharyngeal reflexes and can clear their own airway of saliva, blood, or vomitus. However, dislodged tooth fragments, dental appliances, or mandibular structural collapse may compromise the airway and should be noted. Emergent tracheostomy is seldom needed, even in severe facial fractures, unless a concomitant injury to the cranium, neck, or chest exists.
Control bleeding
Extensive arterial hemorrhage from facial wounds usually results from injury to the maxillary artery, the superficial temporal artery, or the angular artery. Direct pressure is usually sufficient for initial hemostasis, followed by ligation of the bleeding vessel through the wound if it is clearly visible. If no clear source of bleeding is identified, the airway should be protected, a compressive facial dressing applied, and the athlete transferred to the nearest acute care center.
Epistaxis caused by nasal injury can be a source of profuse bleeding. Most cases of simple epistaxis involve disruption of the Kiesselbach plexus in the anterior chamber of the nose. This is usually expediently controlled with direct pressure (ie, pinching the nares together) or the application of a vasoconstrictive spray (eg, oxymetazoline hydrochloride [Afrin], phenylephrine hydrochloride [Neo-Synephrine]). Brisk nasopharyngeal bleeding may occur from disruption of the sphenopalatine artery as it enters the lateral wall of the nasal cavity. This posterior epistaxis requires nasal packing and transfer to an emergency center for further treatment.
Neurologic evaluation
Every maxillofacial injury should be considered a head injury, and patients with such injuries should be given the appropriate neurologic evaluation. The unconscious athlete is assumed to have head and neck injuries, and proper immobilization of the neck and spine should be applied immediately. Mulligan et al reported that in patients with an isolated facial fracture there was an associated 4.9-8% rate of cervical spine injury, 28.7-79.9% rate of head injury, and 2.8-5.8% rate of concomitant cervical spine and head injury. [13]
Detailed examination
After the secondary survey is performed and potentially life-threatening injuries are excluded, any soft tissue injuries and obvious asymmetries of the facial contour (suggesting underlying bony fractures) should be documented. Each health care provider should develop a systematic routine in order to provide a thorough examination. A common approach is to start at the scalp and work down. The following is a guide to evaluating the face; however, it should be noted that facial injuries can have extensions to the scalp and neck, which should not be neglected. The patient should be transferred to an acute care facility and fully worked up and assessed by specialists if there are findings that suggest facial fracture or visual compromise or if the patient has a severe wound in which hemostasis cannot be achieved.
Examination of the upper third of the face
Examination of the upper third of the face aims at confirming the integrity of the frontotemporal branch of the facial nerve, assessing the stability of the supraorbital rims, and assessing the contour of the forehead. Having patients elevate their eyebrows is sufficient to confirm the integrity of the frontotemporal nerve and the frontalis muscle. Lightly touch the forehead to test for ophthalmic division of the trigeminal nerve. Palpation over the supraorbital rims and forehead that elicits pain, crepitus, or the presence of a step-off suggests underlying fractures. Additionally, examine for laceration and hematoma of the scalp that may indicate underlying skull fracture or the source of profuse bleeding.
Examination of the middle third of the face
The eyes, nose, zygoma, and maxilla make up the middle third of the face. [14] The examination of the eyes is extremely important, as injuries such as hyphema, ruptured globe, or retrobulbar hematoma are ophthalmologic emergencies. [15] Initial determination of vision is imperative; practical methods are to ask the athletes to read the scoreboard or any printed material. Gross discrepancy of visual acuity is highly indicative of the presence of an injury. The athletes should be able to close their eyes tightly, which tests for facial nerve and orbicularis oculi muscles. Have the patients gaze in all directions in an "H" pattern to test the extraocular muscles. Limitation of or diplopia with upward gaze often suggests orbital floor fractures. Use a penlight to look for pupillary symmetry and light response, as well as for an afferent pupillary defect. Epiphora, pain, or photophobia may indicate corneal abrasion.
Palpate the infraorbital rims for stability. Look for discrepancy of globe position in the bony orbit (exophthalmos, enophthalmos, hypoglobus, telecanthus), which suggests a fracture involving the orbit.
Gently press over closed eyelids to feel for the turgidity of the globes. A flaccid globe may indicate rupture, while a tense or proptotic globe may indicate retrobulbar hematoma; both findings mandate immediate evaluation by an ophthalmologist. The globe should be protected with an eye shield during the transfer.
Assess for lacerations around the eye. Medial lacerations may involve the lacrimal system, which can lead to epiphora. Superior lacerations may involve the levator palpebrae superioris muscle, which can lead to ptosis. Any laceration involving the upper and lower eyelids should be assessed by a specialist.
The examination of the nose includes the nasal bone, the septum, and the cartilage. The prominence of the nose leads to frequent injury. Therefore, discerning preexisting deformities from acute injuries is important. Deviation of the nasal dorsum, epistaxis, and edema should prompt the examiner to look for septal dislocation and septal hematoma. Failure to identify a septal hematoma may result in necrosis of the septal cartilage and subsequent perforation and collapse leading to a “saddle-nose deformity.” [16, 17]
The examination of the zygoma for a zygomaticomaxillary complex (ZMC) fracture should evaluate for flattening of the zygomatic arch and widening of the midface. Viewing the midface from an inferior or worms-eye view facilitates the detection of these asymmetries, although edema may make this assessment difficult. Lightly touch the malar and nasal sidewall region to test for dysesthesia of the trigeminal nerve infraorbital branch. Trismus or difficulty opening the mouth can be an indication of a zygomatic arch fracture impinging on the coronoid process of the mandible. Subconjunctival hemorrhage of the lateral sclera is a hallmark of a lateral orbital wall fracture, which is a component of a ZMC fracture
Abnormal mobility of the maxilla or hard palate can be detected by grasping the anterior maxillary teeth and firmly attempting to move the maxilla in all directions while stabilizing the forehead. Examination of oral occlusion is combined with examination of the mandible.
Examination of the lower third of the face
The lips, tongue, and cheeks are very susceptible to lacerations when compressed against the dentition. Lacerations involving the vermillion border of the lip require delicate reapproximation to avoid a visible cosmetic defect. (For more information, see Complex Laceration, Lip.) Ask patients to pucker their lips, grin, and show their teeth to test the facial nerve branches. The oral cavity must be cautiously inspected for loose/missing/fractured dentition, lacerations, and the presence of sublingual ecchymosis, which is the pathognomic sign of a mandibular fracture.
Mandibular injuries are often accompanied by pain, numbness of the jaw and teeth, trismus, and malocclusion. The inability of an injured athlete to close his or her mouth should alert the examiner to the possibility of temporomandibular joint dislocation or fracture.
Examination of the ears
Often, when a cervical collar is in place, injuries to the ears are missed. The health care provider should not forget to include the ears during evaluation. The external ears are susceptible to hematoma formation when punched or compressed. If this hematoma is not evacuated, long-term "cauliflower" deformation occurs. [18] Gross hearing should be intact to a mere whisper near the ear. The external auditory canals and tympanic membranes should also be otoscopically inspected for the presence of blood, cerebrospinal fluid, canal laceration, or tympanic membrane perforation. Any fluid collection in the ear canal or behind the tympanic membrane may be indicative of underlying fractures of the skull base.
Soft Tissue Injuries
Sports-related facial trauma generally results when direct contact occurs with another player or a piece of equipment, including a projectile or contact against a playing surface. These blunt traumas often result in contusions, abrasions, and burst lacerations. In addition to treating the soft tissue injuries, the Centers for Disease Control and Prevention (CDC) recommendations for tetanus immunization should be followed. Antibiotic prophylaxis should be given for wounds that involve animal or human bites.
Table 1. Tetanus Wound Management* (Open Table in a new window)
|
Clean, Minor Wounds |
All Other Wounds** |
||
Vaccination History |
Tdap or Td† |
TIG‡ |
Tdap or Td† |
TIG |
Unknown or < 3 doses |
Yes |
No |
Yes |
Yes |
≥3 doses |
No§ |
No |
No|| |
No |
*Adapted from the Centers for Disease Control and Prevention [19] **Including, but not only, wounds contaminated with dirt, saliva, soil, and feces; puncture wounds; avulsions; and wounds produced by missiles, crushing, burning, and frostbite. †The use of Tdap (tetanus, diphtheria, and pertussis) vaccine is preferred to Td (tetanus-diphtheria) vaccination in adults who have never received Tdap vaccine. Single-antigen tetanus toxoid (TT) can no longer be obtained in the United States. ‡TIG = tetanus immunoglobulin §Yes, if over 10 years since the last tetanus toxoid–containing vaccine dose. ||Yes, if over 5 years since the last tetanus toxoid–containing vaccine dose. |
||||
Contusions and abrasions
Contusions represent injury of the soft tissue layers between the underlying facial skeleton and the overlying skin and are associated with varying degrees of tenderness, swelling, and ecchymosis. Keeping the head elevated and applying ice to the affected area for 15-20 minutes every 2 hours is the mainstay of treatment for facial contusions. These injuries can be expected to resolve over several days to weeks.
Abrasions are partial-thickness losses of skin caused by shearing forces within the compressed epidermal and dermal layers. Adequate cleansing with an antiseptic or antibacterial soap and saline should be performed soon after injury with particular care to remove any foreign material in order to avoid "tattooing." These injuries can be very painful, and the use of a topical anesthetic can help to achieve proper debridement. The wound can be dressed with a sterile, nonadherent dressing and treated with twice-daily topical antibiotic ointment. Patients who have abrasions that do not heal after 14 days or that appear to be full thickness should be referred to a specialist for further treatment. Wounds should be closely monitored for signs of infection.
Lacerations and avulsions
Lacerations represent the most common type of facial injury encountered in the athletic setting. When blunt trauma occurs over a bony prominence of the facial skeleton, a linear or stellate laceration may result. The latter is termed a burst-type laceration and, with its jagged skin edges, repair and a good aesthetic outcome are more challenging.
Because of the abundant blood supply to the facial soft tissues, bleeding from a laceration may be brisk and profuse. Immediate management is directed toward achieving hemostasis by applying direct pressure over the involved area with a sterile gauze pad. Once hemostasis is obtained, underlying structures can be seen more easily and should be examined carefully. Facial lacerations should be cleaned with sterile saline to adequately remove bacteria and debris from the wound.
After appropriate cleansing, superficial lacerations without separation of the wound edges may be closed using adhesive bandages (eg, Steri-Strips) or by applying a skin adhesive. For deeper lacerations with separated or jagged wound edges, precise alignment and reapproximation by a plastic surgeon ensures the best functional and aesthetic outcome.
Intraoral lacerations are treated much like skin lacerations. Following thorough irrigation, the intraoral mucosa can be reapproximated with absorbable suture material. Because delayed healing and excessive scar tissue may occur, primarily repair mucosal lacerations, including those of the tongue, whenever possible. (For more information on repairing intraoral lacerations, see Complex Laceration, Lip.)
Avulsed or missing tissue of notable size, especially involving the nose, ear, or lip, should be recovered, if possible, and then wrapped in a saline-moistened gauze and placed in a bag, which should be placed on ice. Transfer to a tertiary care facility may be needed to replant the avulsed tissue. If the wound consists of a small amount of missing tissue, the wound should be cleansed with saline and gently debrided; it should be dressed with an occlusive dressing in order to avoid desiccation.
Although the routine use of antibiotics is not warranted, contaminated wounds may require them. Determine tetanus immunization status, and administer tetanus toxoid when indicated (see table 1). For athletes who plan to return to contact sports with a repaired laceration, an adhesive and adequately padded bandage must be applied to prevent wound disruption.
Hematomas
A collection of blood within the muscle, fascial, and dermal layers represents hematomas, which are generally seen over the zygomatic and periorbital regions. These generally resolve with the application of ice and compression; however hematomas should be monitored for expansion, overlying skin necrosis, or infection, which would warrant immediate medical attention.
Auricular and septal hematomas deserve special attention because of their potential for perichondral injury and subsequent necrosis. A septal hematoma appears as a purple, grapelike swelling from the nasal septum. Incision and drainage followed by anterior nasal packing may prevent the possibility of septal necrosis, impaired breathing, and altered cosmesis.
An auricular hematoma may result from blunt trauma as might be sustained in a boxing or wrestling match. It is noted as a firm, ecchymotic collection in the anterior portion of the ear, which obscures the auricular architecture. Treatment is by incision and drainage of the hematoma, closure of incision with fine monofilament interrupted sutures, and a compressive dressing conforming to the helix and antihelix. For an illustrated demonstration of auricular hematoma drainage, see Drainage, Auricular Hematoma.
Facial Fractures
General Guidelines and Initial Evaluation
Most athletes who sustain facial bones fractures should not return to the game. A second impact to a facial bone that is already fractured may compound the fracture and convert a simple, nonoperative fracture into a complex and disfiguring surgical challenge.
When evaluating an athlete with a potential facial fracture, the care provider should maintain a high index of suspicion and promptly refer the patient to a facility that can adequately image and manage the injury. The following fractures discussed are those most commonly encountered in sports-related facial trauma.
Nasal Fractures
Because of its prominent location on the face, the nose is the most commonly fractured facial structure associated with sports-related facial injuries. [10] Nasal fractures account for approximately 50% of sports-related facial fractures; 15% of those fractures are recurrent. The common perception of the broken nose as innocuous may account for its high rate of undertreatment. However, a poorly managed acute nasal fracture leads to chronic nasal deformities and, sometimes, breathing difficulties that may impair the performance of competitive athletes.
Examination and diagnosis
The diagnosis of a nasal fracture is made clinically. The most common findings in a nasal fracture include epistaxis, swelling and tenderness of the nasal dorsum, bruising around the eyes, and an obvious nasal deformity. Widening of the nasal bridge or telecanthus may indicate a naso-orbitoethmoid (NOE) fracture pattern. [20] Palpation of the nasal bones can demonstrate mobility, irregular surface, or crepitus. If the injured athlete reports a nasal obstruction during inspiration, the examiner should strongly consider a nasal/septal fracture or dislocation.
The intranasal examination should be conducted under proper lighting with a nasal speculum. The examiner can spray the intranasal structures with a vasoconstrictor, such as phenylephrine or oxymetazoline, to allow for better visualization.
Treatment
The indications for treatment of nasal/septal injuries by a physician are persistent bleeding and obvious nasal deformity. Treat any open wounds with copious irrigation, and apply ice to minimize swelling.
Swelling that occurs over time obscures the deformity and makes acute closed reduction difficult. If considerable swelling has occurred, waiting at least 4-7 days for the swelling to subside before treating the nasal fracture is prudent. Treatment can be limited to a simple closed reduction of the nasal bones using topical and local anesthesia in a physician's office setting or can be a more involved reduction of a fractured or severely dislocated septum in the operating room. The realigned septum or nasal bones are then splinted externally and internally. The splints are usually removed in 7-10 days. For an illustrated demonstration of nasal fracture reduction, see Nasal Fracture Reduction.
Carefully consider the decision to return the athlete to competition and the need for nasal protection. The nasal bones generally heal sufficiently within 4-8 weeks, allowing the athlete to return to competition in contact sports. If the athlete resumes competition soon after repair, strongly recommend that he or she use a protective facial device of sufficient strength to prevent further injury.
Orbital Fractures
One third of all orbital fractures are secondary to sports injuries [8] and can almost always be prevented with the use of protective eyewear. The risk of injury to the eye is highly related to the type of sport. High-risk sports are those with high-speed projectile objects, clubs, or aggressive body contacts.
Examination and diagnosis
When an injury occurs near the eye, a thorough eye examination should be performed, as previously described. A circumferential bony framework protects the vital structures of the orbital complex. The aperture of the circumferential bony rim does not allow objects with a radius greater than 5 cm to penetrate to the globe. During the examination, the circumferential bony rim should be palpated. Fractures of the orbital rim can occur at any point on the rim; however, fractures of the inferior rim are most common. These fractures can occur independently or in combination with orbital wall fractures; orbital wall fractures can also occur alone.
A blow to the eye can cause an increase in intraorbital pressure, with or without fracturing of the orbital rim. The thin bones of the orbital floor actually fracture to increase the volume of the orbit and dissipate the pressure that would otherwise rupture the globe. This protective fracturing is called an orbital blowout fracture. It can manifest with ecchymosis, enophthalmos, hypoglobus, periorbital emphysema, and numbness of the area on the ipsilateral cheek supplied by the infraorbital nerve.
Diplopia upon upward gaze can be due to a restriction of movement of the eye because of herniation of orbital fat and the inferior rectus muscle through the orbital floor or due to swelling or contusion of the muscle. A facial bone CT scan with coronal views evaluating the floor of the orbit can help to differentiate the causes. Forced duction test is also helpful in differentiating the causes of diplopia and gaze limitation. In the forced duction test, the affected eye is anesthetized with a topical anesthetic, the sclera is grasped with a fine-toothed forceps at the level of the insertion of the inferior rectus muscle, and the eye is gently moved in a superior and inferior direction. If the globe moves easily, entrapment of the ocular contents can be excluded. Entrapment of the inferior or medial rectus is more likely to be seen in pediatric patients and warrants immediate evaluation by an ophthalmologist.
Treatment
Absolute indications for surgical repair include noticeable enophthalmos, limitation in extraocular movements, and persistent diplopia due to entrapment of the orbital contents in the fracture line.
For details regarding surgical repair of orbital blowout fracture, please visit the Medscape Drugs & Diseases topic Facial Trauma, Orbital Floor Fractures (Blowout).
If an orbital fracture is suspected, the patient should avoid any nose blowing or Valsalva maneuvers to prevent periorbital emphysema. After the injury, if the player returns to competition before 4-8 weeks have passed, strongly recommend protective facial devices sufficient to prevent reinjury. When protective eyewear has been used in racquet sports and face protection devices have been used in hockey, eye injuries have been virtually eliminated. [21]
Zygomaticomaxillary Complex Fractures
The bones of the zygomaticomaxillary complex (ZMC) make up the prominences of the face known as the cheekbones. Fractures of this bony complex account for approximately 10% of sports-related facial fractures. The zygomatic bone articulates with the frontal bone, maxilla, temporal bone, and the wing of the sphenoid, and fractures of this complex usually involve several of these articulations. This type of fracture typically occurs when significant force is directed at the prominence of the cheekbone. The bony complex is forced posteriorly and rotates laterally and inferiorly.
Examination and diagnosis
A thorough examination of the head and neck should be conducted when a ZMC fracture is suspected. Clinical findings commonly associated with ZMC fractures are periorbital ecchymosis, numbness in the distribution of the infraorbital nerve over the cheek, enophthalmos, restriction of movement of the eye upon upward gaze, lateral subconjunctival hemorrhage, and depression of the cheekbone with an associated downward slant of the eye. The medial and lateral canthal tendons that support the eye attach to the medial and lateral orbital rims, respectively, so that any change in the position of the orbital rim changes the axis of the intercanthal line. Any combination of these signs and symptoms may be evident. The most accurate and most commonly used radiologic examination to diagnose ZMC fractures is a computed tomography (CT) scan, which is also used to aid surgical planning.
If a ZMC fracture is suggested, the player should not return to competition, and a specialist should be consulted.
Treatment
Treatment varies depending on the severity of the fracture. If surgical repair is needed, perform it within 7-14 days to prevent early fracture consolidation. Rigid fixation of these fractures is usually obtained with titanium miniplates and screws specifically designed to be used on the facial bones, using surgical approaches that minimize facial scars.
The use of rigid fixation has decreased the need for extended intermaxillary fixation and resulted in more predictable, stable, long-term results. However, research has shown that rigid internal fixation is not as strong as the patient's own intact facial skeleton. A similar blow to the repaired fracture site before the bones have healed puts the athlete at risk for a more severe fracture pattern than the initial injury, and the risk of damage to the underlying vital structures is significant. Therefore, strongly recommend that the athlete refrain from practice or competition for at least 6-8 weeks to allow the fractured bones to heal. Protective facial devices, if properly constructed, may allow the athlete to return to competition earlier.
For details regarding surgical repair of ZMC fractures, please visit the Medscape Drugs & Diseases topic Zygomaticomaxillary Complex Fractures.
Mandibular Fractures
Fractures of the mandible make up approximately 10% of all sports-related facial fractures. Results from a study in Austria indicate that sports accidents are the most common cause of mandibular fractures, occurring in 31.5% of the patients in that series.
The mandible is a horseshoe-shaped structure that articulates with the base of the skull at the temporomandibular joints. It is a strong cortical bone that has several weak areas. It is thin at the angles, at the neck of the condyles (subcondylar area), and at the distal body where the long root of the canine tooth and the mental foramen are located. Because of the mandible's U-shape and several weak, thin areas, the mandible commonly fractures in more than one place.
The tongue is attached to the lingual surface of the anterior mandible; therefore, the anterior segment of a bilateral fracture in the parasymphyseal region has the potential to shift posteriorly, causing the tongue to block the airway. The simple act of pulling the tongue or the anterior jaw forward can open the airway. The tongue or jaw should be stabilized in this position, and the athlete should be transported to the emergency department, with proper cervical spine immobilization if necessary.
Examination and diagnosis
Malocclusion, pain, swelling, difficulty opening the mouth, and intraoral bleeding are the most common signs and symptoms of a lower jaw fracture. Palpation of the mandible, visible step-offs between the teeth, and pain upon stressing the mandible also aid in the diagnosis of a fracture. Panorex view or facial bone CT scan is a reliable image modality for diagnosing most mandibular fractures.
The subcondylar regions are the most commonly fractured areas of the lower jaw. These areas are thinner than the rest of the mandible, and forces generated at impact are transmitted to these areas. The condylar region of the lower jaw is considered a growth center. Fractures of this region in a younger athlete who has not completed growth can result in altered growth of the mandible with associated occlusal problems. Injuries to this region can also result in hemorrhage into the temporomandibular joint spaces and lead to fibrosis and possibly ankylosis with associated inability to move the joint.
Treatment
For details regarding the nonoperative and operative management of mandibular fractures, please see the Medscape Drugs & Diseases topic Facial Trauma, Mandibular Fractures.
Special referral may be required for adolescent athletes. Prior to the full eruption of permanent dentition, referral to a craniofacial or pediatric plastic surgeon may be warranted, since the unerupted teeth are vulnerable to damage with conventional fixation techniques.
Athletes with fractured jaws should not be allowed to return to play until healing has occurred and they are out of maxillomandibular fixation (which generally takes 4-6 weeks). A protective cage or helmet with a jaw extension can allow athletes in selected sports to return to competition earlier.
Dentoalveolar Injuries
Dentoalveolar fractures are fractures of the alveolar bone and the associated teeth. Injuries to the mouth are particularly common in team sports. Any trauma to the lower face can result in an injury to the dentoalveolar complex. Lacerations of the lips and intraoral mucosa are frequently associated with injury to the teeth and their supporting structures. The most commonly injured teeth are the maxillary central incisors.
Examination and diagnosis
When assessing dentoalveolar injuries it is important to take into account the age of the patient and the presence of primary dentition. The normal adult has 28-32 permanent teeth (8 incisors, 4 canines, 8 premolars, and 8-12 molars). However, children under age 5 years have primary dentition, and those aged 6-12 may have mixed dentition. It is often helpful to ask parents about their child’s dentition status when performing an examination. [9] As reported by Ranalli, signs and symptoms of dentoalveolar trauma include intraoral bleeding, tooth malposition, malocclusion, mobility of the affected structures, pain, and altered sensation of the teeth. [22, 23]
The examiner should always count the athlete's teeth after an injury. If any teeth are missing, every effort should be made to retrieve them. Teeth may lodge in the surrounding soft tissues, such as the lips and tongue. Teeth also may be lodged in the airway or aspirated into the lungs. Appropriate airway precautions should be taken and radiographs obtained to exclude these possibilities. The potential for permanent loss of a tooth is high in more severe injuries.
The teeth involved in dentoalveolar fractures may or may not have associated fractures of the crown or root, or they may be luxated or avulsed. Treat dentoalveolar fractures as open fractures. A specialist must address tetanus prophylaxis, antibiotic coverage, and reduction and fixation of the fracture. Referral to a dental specialist for outpatient follow up should be arranged.
Tooth Fractures
Tooth fractures can involve the crown or the root. The most common traumatic injury seen by the general dentist is the crown fracture (79%). [9] Fractures of the crown in which only the enamel is fractured do not usually require urgent attention. Treatment for this includes smoothing any sharp edges and relieving the occlusion of the athlete's tooth.
However, if the fracture involves the neurovascular tissue, it exposes the vital nerve center (pulp) of the tooth and can be quite painful. Pulp injury with pain to air exposure requires immediate dental referral. Treatment includes covering the exposed pulp of the tooth with calcium hydroxide within 24 hours and acid-etch bonding of the fractured piece of tooth with a composite resin. If the fractured piece of crown is retrieved, it may be saved by placing it in Hank’s balanced salt solution (Save-A-Tooth), saline or cold milk, and it may then be rebonded directly to the fractured tooth by means of acid-etch bonding or light-cured glass ionomer resin material. This treatment alleviates discomfort and allows healing to begin.
Root fractures can be more difficult to diagnose. They usually occur in teeth that are fully formed. Any mobility of a tooth or pain upon palpation suggests a root fracture. The athlete should be referred to a dentist for dental radiographs, definitive testing of the involved teeth, and management of these types of injuries.
Tooth Displacement
Luxation, or displacement of a tooth, occurs when the tooth is malpositioned in its bone socket. There can be subluxation (loosening), extrusion (partial avulsion), or intrusion of a tooth. Treatment for subluxation is occlusal adjustment, observation, and vitality testing. Treatment for extrusion is repositioning and splinting, periodic vitality testing, and possible root canal intervention. Treatment of luxation and extrusion usually requires the use of a local anesthetic because manipulation can be quite painful. Lastly, intrusion of a tooth with incomplete root development, as in a child, is treated by allowing the tooth to re-erupt, and manipulation should not be performed by a nondental health care provider. Teeth with complete root development that suffer intrusion are repositioned and possibly treated with calcium hydroxide root canal therapy. Patients with tooth displacement should be seen within 24 hours by a dental specialist. [9]
Tooth Avulsion
Avulsion is the complete separation of the tooth from the alveolus (socket), which is an urgent situation. The prognosis for viability of the tooth and successful replantation is inversely proportional to the length of time the tooth is out of the socket. Treatment principles are to replant and stabilize the avulsed permanent tooth as quickly as possible. According to the American Academy of Pediatric Dentistry 2001-2002 Reference Manual, pulp and periodontal healing are more likely to occur when the permanent tooth is replanted immediately (< 5 min).
Reimplantation of a tooth within 30 minutes has >90% chance to save the tooth; after more than 2 hours, the chance of survival is 5%. [24] The key to successful replantation is the continued nourishment and maintenance of the periodontal ligament of the tooth. If the periodontal ligament fibers become desiccated or necrotic or are removed as a result of rough handling, the tooth may undergo resorption or can ankylose to the surrounding bone and may ultimately be lost. Gentle handling of the root of the tooth at the point where the ligaments are attached is imperative (although handling of this area should be avoided altogether, if possible). The athletic trainer should not scrub or brush the root of the avulsed tooth; instead, he or she should gently handle the tooth by its crown and irrigate it with saline, if available. If the tooth cannot be immediately replanted into its socket, it should be cleaned gently and simply placed in the buccal vestibule of the mouth (between the cheek and gums), and the athlete should be immediately transported to a dentist.
If the athlete is unable to hold the tooth this way, the tooth should be placed in fresh, cold milk; sterile saline; Hank’s balanced salt solution (Save-A-Tooth); or saliva. Tap water should not be used, due to the low osmolality that can disrupt cells. According to the article "Best face forward: athletic facial injuries," published by the University of Pittsburgh Medical Center, milk is an ideal storage medium; mitotic activity in periodontal cells has been maintained for up to 6 hours when a tooth is stored in milk. [25, 9]
A diet of soft foods and analgesics should be prescribed for the management of pain. According to the American Academy of Pediatric Dentistry, antibiotic therapy should be considered and tetanus immunization status should be addressed. Additionally, often the tooth requires endodontic treatment (root canal therapy) for ultimate salvage.
Protective Facial Devices
Although restoring function and aesthetics is important, preventing injuries should be the primary focus. According to Johnsen and Winters, when use is enforced, protective facial devices decrease the incidence of facial injuries. [26] In 1959, face masks became mandatory for football players. Prior to 1960, 50% of football injuries involved the facial or dental regions. In a 1988 study by Welbury and Murray, the incidence rate for football-associated maxillofacial injuries dropped to approximately 1.4% due to protective head gear. [27] According to Sports Dentistry Online, the use of full-face protection and helmets has also decreased the rate of facial injuries in ice hockey. As mentioned earlier, when protective eyewear has been used, eye injuries have been almost totally eliminated.
Helmets afford the athlete protection of the cranium and have been instrumental in decreasing the morbidity and mortality from cranial injuries. However, they afford little, if any, protection for the middle and lower face. Results of an Austrian study by Emshoff et al revealed a high prevalence of lower facial injuries in cycling and skiing, sports in which athletes often wear helmets. [28] Selig et al found that the majority of pediatric injuries in the Austrian Alps occurred while skiing. [29] Many professional skiers now wear racing helmets with an extension that covers the lower jaw, which may help to reduce the prevalence of facial fractures.
Medical professionals working with athletes should be aware of available protective devices and educate players regarding their use and benefits. In a study by Dursun et al, 78.3% of "weekend warrior" soccer players were unaware of available mouth guards and their benefit. [30]
Mouth protection
As reported by Rampton et al, the use of mouthpieces and the reduction of injuries to the orofacial region are well correlated. [21, 26]
The American Society for Testing and Materials classifies mouth guards as type I (stock), type II (mouth-formed), and type III (custom-fabricated over a dental model of the wearer).
Stock mouth guards are almost always readily available and inexpensive. However, they are considered the least retentive, the most bulky, and the most likely to interfere with breathing and speech. Some authors (ie, Welbury and Murray, Ranalli) consider them potentially hazardous and believe they should not be recommended. [27, 22]
Two types of mouth-formed mouth guards are manufactured. The thermoplastic variety uses the boil-and-bite technique. The second type of mouth-formed mouth guard is the soft-lined variety, which uses ethyl methacrylate in a more rigid shell. Ranalli demonstrated that unsatisfactory results occur when athletes attempt to fit these mouth guards themselves. [22] These types of mouth guards often do not cover the posterior teeth and are thin over prominent teeth.
Custom-fabricated mouth guards produced by a dentist reportedly have a predictable long-term fit that does not degenerate in thickness over time, resulting in better retention and comfort; however, these products are more expensive.
According to Sports Dentistry Online, a mouth guard must be properly fitted. It must be protective, comfortable, resilient, tear-resistant, odorless, tasteless, nonbulky, and cause minimal interference with speaking and breathing. However, possibly the most important criteria are that it must fit well, have excellent shape retention, and must be sufficiently thick in critical areas. As a general rule, Chapman recommends that a standard mouth guard be replaced after approximately 2-3 years, if not earlier. [31]
Eye protection
According to Easterbrook, appropriate, well-fitted eye protective devices have reduced the number of injuries to the eyes. [32] Additionally, Guyette suggests that protective eyewear should be constructed from a polycarbonate material that is shatterproof and lightweight. [33] It should also be constructed so that it does not interfere with the athlete's direct or peripheral vision.
A study by Kriz et al found that among female field hockey players, severe eye/orbital injuries fell by 67% and severe/medical disqualification head/facial injuries were reduced by 70% after the national mandate for protective eyewear was implemented for field hockey competitions sanctioned by the National Federation of State High School Associations. [34, 35]
Facial protection
Although protective eyewear can theoretically protect the immediate periorbital bony framework, it cannot afford protection for the midface, including the cheekbones, nasal region, and dentoalveolar structures. The most commonly used protective device for the prevention of injuries to the midface, particularly the nose, is a custom-made plastic face shield. When such a shield is used following an injury, it is typically designed to cover the injured area of the face while not touching it. Face-guard use results in a 35% reduction in facial injuries compared with nonuse. [7]
A patented face mask has been developed that is composed of 2 layers of protective materials, ie, a shatterproof outer shell of polycarbonate lined with an energy-absorbing and energy-dissipating viscoelastic polymer. This mask is custom fabricated to the individual's face and injury. The mask is designed to take advantage of the naturally protective design of the bony facial buttresses and reinforces them to further decrease the amount of energy that reaches the injured site. This mask design has been used by players in the US National Basketball Association for protection of nasal fractures and fractures of the orbit.
The designs of protective facial devices are improving in function and aesthetics. However, no matter how good the protection is, if the athlete will not wear the protective equipment, then the risk of injury has not been lessened. As reported by Ellis, noncompliant athletes have a higher recurrence rate of injury than those who are compliant. [36] All members of the sports health care team should educate athletes about the importance of protective equipment and encourage the use of all protective devices to ensure the athlete's safety.
-
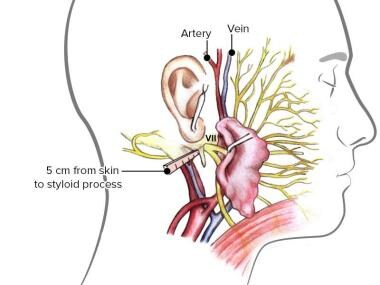
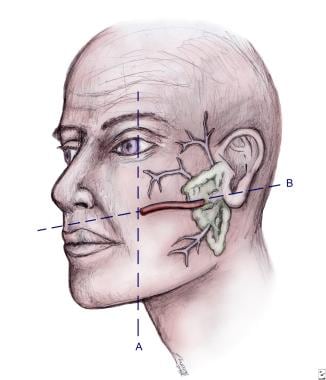
Location of parotid gland and duct system.
-
Skin tension lines of the face. An incision or a wound parallel to these lines results in better cosmesis. The directions of the skin tension lines are perpendicular to the underlying facial muscle orientation.
-
Major aesthetic subunits of the face. Illustrated by Charles Norman.
-
Motor and sensory facial innervation by the facial and trigeminal nerves.
-
Course of the facial nerve after exiting the cranial base and passing through the parotid gland.
-
Bones of the face and skull.