Background
Alloplastic facial implants offer the reconstructive surgeon certain advantages over autogenous tissue, including availability of material, simplification of operative procedure, and limited donor site morbidity. Depending upon the desired surgical result, the implant must be chosen based upon its physical properties. In order to prevent extrusion or infection, proper preoperative planning and operative technique are essential.
History of the Procedure
The use of alloplastic implantable materials to achieve improved facial contours has been noted for centuries. Early implants consisted of naturally occurring materials (eg, gold or ivory), while modern implants are complex materials such as ceramic, silicone or carbon-based polymers. [1] The search for the perfect implant material is still under way.
Problem
The appearance of the malar aesthetic unit is a strong component of western youth and beauty. A round, more prominent malar area conveys a youthful, healthy appearance. As aging occurs, the malar soft tissues atrophy and descend, creating an aged face.
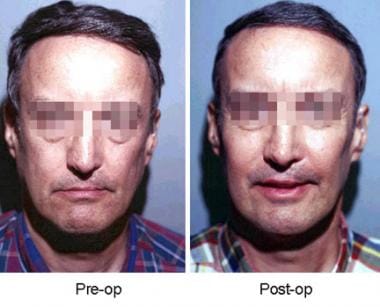
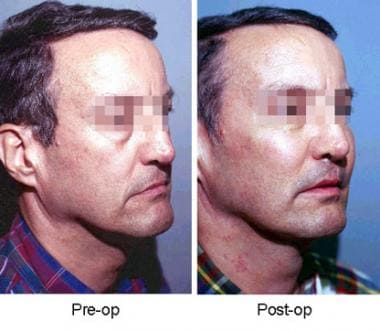
Malar deficiencies can be classified as congenital or acquired, Bony deficiencies or asymmetries are typically treated with osteotomies (possibly requiring bone grafts) or implants. Soft tissue deficiencies can be corrected with soft tissue resuspension, injectables (eg, fat injection), or implants. [2, 3] See the images below.
Etiology
Malar deficiencies and asymmetries can be classified as congenital or acquired. Examples of congenital defects include Treacher Collins Syndrome, hemifacial microsomia, and familial inheritance of physical attributes. Acquired deficiencies can be due to trauma, radiation, or aging. Aging, smoking, and sun exposure lead to atrophy and sagging of the soft tissues overlying the zygoma, giving the face a less youthful appearance.
Ethnic differences in malar position, symmetry, size, and definition should be considered when contemplating alloplastic implantation. For example, people of Asian descent typically have flatter, wider malar areas than people of Northern European decent.
Presentation
A thorough and critical analysis of a patient’s face is required prior to embarking upon malar augmentation. [4] The analysis should consist of bony and soft tissue abnormalities. Noting asymmetries of the face preoperatively and pointing them out to the patient is critical. Having the patient look into a mirror while pointing out asymmetries can be exceedingly useful, as can photographic analysis (postoperatively, the patient will see himself in the mirror and in photographs, and through these formats he will judge the surgical outcome).
For congenital deformities, make certain that skeletal maturity has been reached. For acquired deformities, make certain that no other functional impairments need correction (eg, enophthalmos). Although various authors propose differing techniques for facial analysis, the most important aspect of malar augmentation remains matching the patient to the correct type of implant. Since malar deficiencies vary, the proper implant, placement, and location also vary.
General anesthesia is typically preferred, but, depending upon the size of implant and amount of required dissection, malar implants can be placed using local or general anesthesia. General anesthesia allows a more liberal dissection for patient comfort. A thorough history and physical examination should be performed for each patient, with specific focus on medications or supplements that can cause bleeding, smoking history, and wound healing issues.
Indications
Several general categories of candidates for malar augmentation include the following:
-
Posttraumatic
-
Congenital deformities
-
Midface hypoplasia
-
Very long, narrow face
-
Aged face with atrophy and ptosis of soft tissues
-
Very round, full face
-
Unbalanced aesthetic triangle
The first two categories can be identified by a proper history. If midface hypoplasia is considered, the occlusion should be properly examined and a cephalogram evaluated. Patients in all of these categories may benefit from malar augmentation. (The first three categories are treated more with bony augmentation; the other four use more soft tissue augmentation.)
Malar augmentation in aged, thin, round, or familial unbalanced faces can create a more aesthetically pleasing appearance. Inferior descent of the malar fat pads (as typically seen in aging) can be improved with implants and proper soft tissue resuspension. [5]
Relevant Anatomy
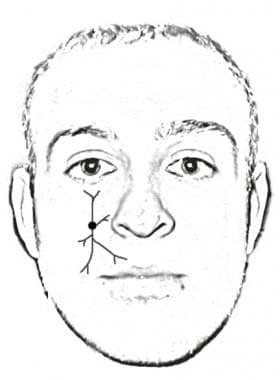
Knowing the location of the infraorbital nerve is critical when performing malar implantation. The nerve is typically located along a plumb line from the patient's medial limbus of the eye. See the image below.
Preservation of the nerve during dissection is paramount. Hypoesthesia can occur following malar implant placement.
Contraindications
A history of radiation, bleeding disorders, problems with healing, or anticoagulant medications are considered strong relative contraindications. Active infection is an absolute contraindication.
-
Frontal view of patient before and after insertion of malar implants.
-
Side view of patient before and after insertion of malar implants.
-
Infraorbital nerve.