Practice Essentials
Trauma to the hand is common, with resultant fractures of the metacarpals and phalanges accounting for approximately 10% of all fractures. Most of these injuries are treated with splinting followed by early motion. For information on splinting hand injuries, see the Medscape Drugs and Diseases articles Volar Splinting, Radial Gutter Splinting, Ulnar Gutter Splinting, and Sugar-Tong Forearm Splinting.
The vast majority of metacarpal fractures occur in persons aged 10-40 years, with a predilection for males. These fractures typically result from trauma sustained in sports, motor vehicle accidents, or work-related injuries. [1]
Although most metacarpal fractures can be successfully treated with closed management, certain fractures and dislocations require surgical intervention to ensure optimal restoration of function.
Signs and symptoms of metacarpal fractures and dislocations
Point tenderness or visible deformity may provide the earliest clinical indicator of metacarpal base fractures. Later signs include edema and ecchymoses.
Problems associated with metacarpal fractures of the shaft and neck relate primarily to foreshortening, rotation, and angulation. Inspection for loss of knuckle prominence and the presence of scissoring often lead to an accurate focus prior to radiographic review.
Pain, swelling, and loss of motion, often accompanied by soft tissue trauma, are the key clinical indicators of injury to the metacarpophalangeal (MCP) joint. Crepitus or joint locking may be present on attempted ranging with intra-articular injuries.
MCP dislocations are identified by local pain and positional deformity.
Workup in metacarpal fractures and dislocations
The primary means of evaluating hand injuries beyond the history and physical examination is through plain radiographs.
Significant injury to the hand should be assessed first with posteroanterior (PA), lateral, and oblique views.
The Roberts view is helpful in more fully assessing the first metacarpal base, while the Brewerton view aids in detailing the anatomy of fractures and chips of the metacarpal heads. The clenched fist view can reveal ligamentous injuries at the metacarpal bases and intercarpally.
Imaging of specific areas also includes the following:
-
Carpometacarpal (CMC) injuries - The key to radiographic diagnosis lies in the subtle loss of joint space, as seen on AP projections; this often appears as a "broken saw tooth" sign at the CMC joint; this sign may be accompanied by displacement noted on the lateral or oblique views; tomograms may be necessary to accurately diagnose these injuries
-
Metacarpal shaft and neck injuries - AP, lateral, and oblique radiographs typically will demonstrate the fracture and displacement
-
Metacarpal head fractures - Evaluation of these injuries may require additional imaging studies, such as Brewerton view radiography, tomography, or computed tomography (CT) scanning, to evaluate for fracture and displacement
-
MCP dislocations - AP radiographs show overlap of the metacarpal head and base of the proximal phalanx; lateral radiographs are diagnostic with the presence of dorsal displacement of the proximal phalanx
Plain tomography or CT scanning can be helpful in diagnosing intra-articular injuries to determine fracture alignment and displacement.
Management of metacarpal fractures and dislocations
Medical therapy
Most injuries to the metacarpals can be managed nonoperatively. Management usually begins by administering sedation, local anesthesia, or both, followed by closed reduction of the fracture or dislocation.
After satisfactory reduction, a forearm-based splint is applied and held in place by a lightly applied compressive wrap. The goal of nonoperative management is to obtain reasonable alignment with stability, which will permit early range of motion of the fingers and wrist.
While most fractures and dislocations can be treated nonoperatively, closed reduction is conveniently performed in a setting where percutaneous pinning may be used, since acceptable reductions may be unstable without such fixation.
Surgical therapy
Although closed management is generally acceptable, certain fractures and dislocations require operative intervention to ensure satisfactory restoration of function. [2]
Surgical treatment includes the following:
-
CMC injuries - Fracture-dislocations of the metacarpal in which the dorsal portion of the hamate is fractured should be treated with open reduction and internal fixation (ORIF)
-
Metacarpal fractures - Most fractures can be stabilized with simple Kirschner wire (K-wire) fixation; the K-wire can be placed longitudinally or transversely into the adjacent metacarpal
-
Metacarpal head fractures - Fixation of head fractures can be accomplished with K-wires, cerclage wiring, or interfragmentary screws; fixation should be stable enough to allow early motion
-
MCP dislocations - Complex dislocations are difficult to reduce and usually require open reduction; they are most common in the index and small fingers
Epidemiology
Frequency
Fracture of the metacarpals and phalanges comprises approximately 10% of all fractures. Metacarpal fractures account for 30-40% of all hand fractures; fractures of the first and fifth metacarpals are the most frequent. Fractures of the fifth metacarpal neck (boxer fractures) alone account for 10% of all fractures of the hand. Lifetime incidence of metacarpal fractures is approximately 2.5%. [3]
Etiology
Injury to the metacarpals is the result of either direct or indirect trauma. The nature and direction of the applied force determines the resultant fracture or dislocation. Specific injury patterns that occur from commonly seen trauma are as follows:
Carpometacarpal injuries
Metacarpal base fractures and dislocations of the carpometacarpal (CMC) joint commonly result from a fall or other stress on the hand with the wrist flexed.
Metacarpal shaft and neck injuries
Metacarpal shaft fractures typically are produced either by axial or rotational loading or direct trauma. Metacarpal neck fractures, the most common metacarpal fractures, usually result from striking a solid object with a clenched fist.
Metacarpal head injuries
Metacarpal head fractures are intra-articular injuries and result from axial loads or direct trauma.
Metacarpophalangeal (MCP) dislocations
MCP dislocations usually are the result of forced hyperextension of the proximal phalanx on the MCP. [4]
Pathophysiology
Metacarpal base injuries
Injuries to the metacarpal base include fractures, dislocations, or a combination of these (fracture-dislocations). The CMC joints, with the exception of the thumb, are generally stable joints, with the metacarpal bases held in position by dorsal and volar CMC ligaments. The individual metacarpal bases are also strongly bound together by interosseous ligaments. The most common injuries seen in this region of the metacarpal are impaction fractures caused by excessive axial loading, avulsion fractures from tendinous loading, and combinations of abnormal axial and tendinous loading.
Carpometacarpal dislocations and fractures
Carpometacarpal dislocations may occur with or without fracture. Commonly, either avulsion (chip) fractures of the metacarpal base, or fracture of the dorsal hamate accompanies CMC dislocations. A dislocation and fracture at the base of a single metacarpal should signal the examiner to look for fractures or dislocations of the adjacent metacarpals, as the strong interosseous ligaments at the base of the metacarpals very typically associate adjacent injury.
Fracture-dislocation of the base of the fifth metacarpal is a common intra-articular injury; dorsal and proximal fragment displacement is due to extrinsic extensor carpi ulnaris (ECU) and flexor carpi ulnaris (FCU) tone and is the corollary to the Bennett fracture of the thumb. [5] Thus, this injury has been termed the reverse Bennett fracture. The fourth and fifth metacarpals are the most mobile about the CMC interface, their bases articulating with two distinct, ridge-separated, concave facets on the hamate. While direct blows to the ulnar border of the hand tend to create extra-articular fractures of the metacarpal base, intra-articular fractures are usually the result of an axial load. The intra-articular fracture pattern usually leaves one third to one fourth of the radial articular base seated on the hamate with the remaining ulnar fragment displaced dorsally and proximally.
Other commonly seen base fractures include the Bennett and Rolando patterns; each of these is classically described for the first metacarpal. [5, 6] Both may develop as fracture dislocations of the first metacarpal because of extrinsic and intrinsic muscular forces acting on the fragments. While the Rolando fracture, a tripartite intra-articular T or Y pattern, was described for the first metacarpal, it has, by convention, become commonly used for this pattern seen involving other metacarpal bases. The Roberts radiographic view is especially helpful in fully assessing the first metacarpal base.
Metacarpal shaft/neck fractures
Axial loading, direct blow, or torsional loading can cause metacarpal shaft fractures. These fractures are appropriately described by location, fracture pattern, and displacement. Transverse, oblique, and spiral are the accepted terms used to describe the patterns most commonly seen. Importantly, fracture pattern can often ascribe a mechanism of injury. Direct blows often result in a transverse pattern, while axial and torsional loads typically form oblique and spiral fractures, respectively. [7]
Fractures of the metacarpal neck are among the most frequent fractures of the hand; in these fractures, the fifth metacarpal is most likely to be fractured. Such fractures are usually caused by striking a solid object with a closed fist and have been commonly named boxer fractures.
Metacarpal head injuries
Fractures of the metacarpal head are rare injuries. These fractures are intra-articular and, if displaced, usually require open reduction and internal fixation (ORIF). The etiology is usually direct trauma to the joint or an avulsion injury of the collateral ligaments. Injuries caused by direct trauma are often comminuted. Penetration into the metacarpophalangeal joint by teeth or other objects is a common cause of injury to the articular surface of the metacarpal head. These contaminated penetrating injuries carry a special risk of destructive joint sepsis if not recognized. The Brewerton view radiograph can help in revealing occult fractures and joint surface injuries.
MCP dislocations
Almost all MCP dislocations occur with the proximal phalanx displaced dorsally on the metacarpal head. No specific dorsal restraint spans the joint other than the relatively diaphanous dorsal joint capsule and extensor mechanism. The collateral ligaments usually remain intact, and the weaker proximal insertion of the volar plate avulses from the metacarpal chin. Simple dislocations can be reduced without operative intervention under local anesthesia or a combination of local anesthesia and sedation by wrist flexion and application of dorsal pressure at the base of the proximal phalanx; however, some special exceptions are worthy to note.
Volar plate or, in the case of the thumb, sesamoid, interposition into the MCP may prevent reduction. Index and small finger MCP dislocation reductions, in particular, may be inhibited by MCP entrapment of lumbrical and flexor tendons. Dislocations that cannot be easily reduced by closed means are termed "complex" and warrant open reduction. Moreover, inappropriate MCP hyperextension attempts at closed reduction may lead to sesamoid or soft tissue interposition into the MCP joint, thereby converting simple dislocations to complex.
Presentation
Injuries to the metacarpal base
Most fractures of the metacarpal base are impaction fractures, often associated with other injuries. These fractures are rare and often go undiagnosed. Diagnosis, while directed by clinical examination, is usually confirmed with radiography. Point tenderness or visible deformity may provide the earliest clinical indicator of injury. Later signs include edema and ecchymoses.
Beyond obtaining a good history of events from the patient, the most useful clinical examination in the context of metacarpal base fractures is inspection. Taking particular note of mechanism, along with position of external lacerations, abrasions, and contusions, can help guide the examination. Specific areas of injury can be difficult to isolate by more directed means because of patient pain and swelling. The author has found it extremely helpful, in cogent patients who may have closed fractures, to ask them to point, with one finger only, to the area of maximal tenderness. Radiographs are required in suspected injury. The author prefers hand position and alignment (P/A), lateral, oblique, clenched fist (augmenting any base fragment lucency and highlighting intermetacarpal base ligamentous instability) and Roberts (first metacarpal base) views.
Fractures of the metacarpal shaft and neck
Problems associated with metacarpal fractures of the shaft and neck relate primarily to foreshortening, rotation, and angulation. Of these, malrotation is the most functionally important, as a minor rotational deformity can cause the fingers to overlap or "scissor" when the hand is closed. This malrotation can result in a weakened grip and a constant annoyance for the patient. Inspection for loss of knuckle prominence and the presence of scissoring often lead to an accurate focus prior to radiographic review. High energy and penetrating trauma may result in comminution, bone loss, or both; specialized surgical considerations include a possible need for bone grafting or specialized means of fixation. The fourth and fifth metacarpals are the most commonly fractured. Radiography of suspected injury is required. The author prefers hand P/A, lateral, and oblique views to fully assess these injuries.
Injuries to the metacarpal head
Pain, swelling, and loss of motion, often accompanied by soft tissue trauma, are the key clinical indicators of injury to the MCP joint. Crepitus or joint locking may be present on attempted ranging with intra-articular injuries. The Brewerton view radiograph can be quite helpful in assessing these injuries without the delays typically associated with obtaining tomograms.
MCP dislocations
MCP dislocations are identified by local pain and positional deformity and can be confirmed by plain lateral radiographs.
Indications
Most injuries to the metacarpal are managed with closed reduction and external splint immobilization. Indications for operative treatment include failure to achieve or maintain acceptable reduction, open fractures, multiple fractures in the hand, complex injuries, displaced intra-articular injuries, and fractures with serious soft tissue injury requiring a stable skeletal support. Specific indications are described below.
Fractures and dislocations of the metacarpal base
Impaction fractures of the metacarpal bases that are not significantly displaced can be treated with splinting, followed by early mobilization.
CMC fracture-dislocations usually are unstable. Although historically these fractures were treated with closed reduction and immobilization, frequently with good results, current literature supports closed reduction and pin fixation as closed management leads to residual pain and weakness of grip.
Fracture-dislocations of the metacarpal in which the dorsal portion of the hamate is fractured and displaced should be treated with ORIF.
Open reduction with pin fixation is often required with multiple CMC joint injuries, especially when there is a large hamate fracture or the dislocation is irreducible.
Fractures of the metacarpal shaft
Metacarpal shaft fractures tend to angulate apex dorsally, with the head displaced volarly. This is due to the tendency of axial forces to focus energy on the concave volar cortex of the metacarpal shaft, coupled with the volar dominant tone of the intrinsic musculature as a deforming force during and after impact. Foreshortening is also a product of intrinsic muscular force and is illustratively seen when oblique fractures slide at the fracture line. Only a small amount of angulation (< 10°) is acceptable in the second and third metacarpals because of their limited CMC motion. The fourth and fifth finger metacarpals are much more mobile, and volar angulations of 30° and 40° can be accepted, respectively. The more proximal the fracture, the more amplified the effect of angulation; thus, the more proximal the fracture, the less angulation should be tolerated by the treating physician.
Indications for surgery include open fractures, unstable fractures, nonreducible fractures, multiple fractures (inherently unstable patterns), or fractures that represent early malunion from poor anatomic alignment.
Fractures of the metacarpal neck
Metacarpal neck fractures usually can be managed closed without operative intervention. Although the degree of angulation acceptable is controversial, higher degrees of angulation can be accepted with little or no functional deficits in fractures of the neck, especially in the fourth and fifth digits.
Patients should be informed of the cosmetic change to the appearance of the hand, but overall good function is the rule rather than an exception with closed treatment.
Fractures and dislocations of the metacarpal head
Metacarpal head fractures are intra-articular. Displacement of a metacarpal head fracture should be treated with ORIF to ensure a stable, anatomic reduction and allow for early motion. Simple dislocations are best treated by wrist flexion and dorsal application of pressure to the P1 base. Inappropriate MCP hyperextension to recreate the position of injury should be avoided in order to prevent the creation of complex from simple dislocations. Complex nonreducible dislocations require operative reduction.
Relevant Anatomy
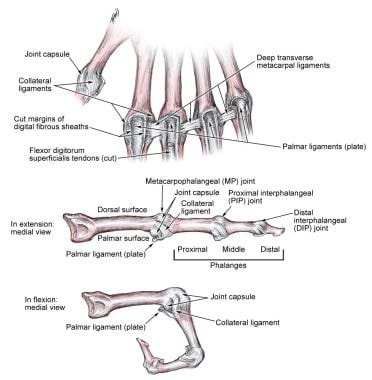
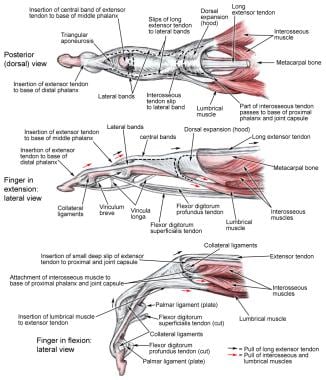
Common patterns of injury to the hand result both from recurring etiologic patterns and the unique anatomy of the hand. See the images below.
The metacarpals are long, tubular bones with an intrinsic axial and a collective transverse arch. The bones have a volar arc when viewed from their lateral aspect and have a oblong, closed "V" shape viewed cross-sectionally with relatively thicker volar cortices. They are joined proximally and distally by ligamentous attachments. The second and third metacarpals are fixed rigidly in their CMC seats, while the fourth and fifth metacarpals are capable of 15° and 25° of motion at their respective CMC rests. The thumb is highly mobile, and its unique motion and injury patterns are addressed in a separate chapter. The arc of motion at the MCP joints ranges from 85-105°.
The cam-shape of the metacarpal heads leads to relaxation of the collateral ligaments in extension, permitting adduction and abduction of the fingers. With flexion of the MCP joints, the collateral ligament becomes taut and acts to stabilize the fingers for power pinch and grip. Increased tension in the collateral ligaments with MCP flexion can be used by the clinician to stabilize the metacarpal head while reducing a metacarpal neck fracture and then to maintain stability through immobilization.
The volar aspects of the cross-sectional metacarpal closed V shape noted earlier are the site of origin for both dorsal and volar interossei muscles. These muscles are important deforming forces in metacarpal shaft fractures and, because of their volar positioning, contribute to angulation as well as foreshortening.
Joint congruency, collateral ligaments, and volar plate each act to provide stability to the MCP. The volar plate is a cartilaginous ligament on the volar aspect of each MCP joint. Volar plates are interconnected via the deep transverse intermetacarpal ligaments, which provide additional stability. The plates are thicker at their insertions on the proximal phalanges and weaker at their metacarpal origins.
Contraindications
The treatment of metacarpal fractures has few absolute contraindications. Most are amenable to either closed versus open reduction with internal versus external fixation or cast immobilization. However, placing internal fixation, such as miniplates or screws, in either infected or clean wounds that cannot be closed primarily is inadvisable. If internal fixation in this setting is planned, any soft tissue defects should be immediately reconstituted by means of soft tissue mobilization or transposition at the time of fixation.
-
Displaced fourth and fifth metacarpal fractures, anteroposterior view.
-
Displaced fourth and fifth metacarpal fractures, lateral view.
-
Fourth and fifth metacarpal fractures, oblique view.
-
Fourth and fifth metacarpal fractures after intramedullary pinning, anteroposterior view.
-
Fourth and fifth metacarpals after intramedullary pinning, lateral view.
-
Complex second metacarpophalangeal dislocation in a skeletally immature patient. Note the position of the finger and dimpling of skin on volar hand.
-
Radiograph of the hand of the patient in Image 6.
-
Intraoperative photo of the second metacarpophalangeal joint of the patient in Images 6 and 7. Note the displaced volar plate between the metacarpal head and the proximal phalanx.
-
Metacarpophalangeal ligaments.
-
Metacarpophalangeal musculoskeletal structure.
-
Brewerton view.
-
Roberts view.