Practice Essentials
Breast implants are designed for use in cosmetic enhancement and reconstruction. [1] According to the American Society of Plastic Surgeons (ASPS), there were approximately 193,000 breast augmentation procedures performed in 2020, making this operation one of the top five cosmetic surgical procedures, after nose reshaping, eyelid surgery, facelift, and liposuction (see the image below). [2]
Saline breast implants
Saline breast implants are approved by the US Food and Drug Administration (FDA) for breast augmentation in women aged 18 years or older and for breast reconstruction in women of any age. These implants contain a silicone outer shell filled with sterile saline and have the following features:
-
May be empty initially (and filled during the procedure of implantation) or pre-filled
-
Available in different sizes
-
Have smooth or textured surfaces to their shells
-
Can be placed with integrated remote-fill ports - Also permit postoperative adjustment of implant saline volume
-
Less costly than silicone-filled products
-
Implant ruptures quickly detectable
-
Possible visible implant rippling on surface of augmented breast in women with thin breast tissue
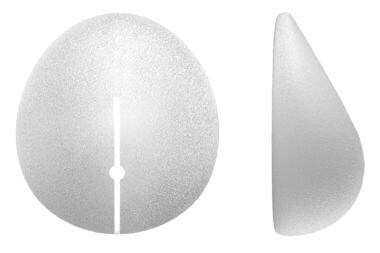
Silicone gel–filled breast implants
Silicone gel–filled breast implants are FDA approved for breast augmentation in women aged 22 years or older and for breast reconstruction in women of any age. These implants have a silicone outer shell filled with silicone gel of varying consistencies and feature the following:
-
Available in different sizes
-
Have smooth or textured surfaces to their shells
-
More costly than saline-filled implants
-
Have a more natural feel than saline-filled implants
-
Less noticeable rippling in thin-skinned augmentations
-
Typically cannot be placed through a transumbilical incision (unlike remote-fill ports) but can be implanted through periareolar, inframammary, and transaxillary incisions
The introduction of breast implants with cohesive silicone gel, that is, gel featuring a greater number of cross-links between molecules, was aimed at helping the implants retain their shape and inhibiting the gel from disseminating into adjacent tissues. So-called “gummy bear” implants contain a form of silicone called highly cohesive gel. [1, 3]
Surgical incisions and dissection planes
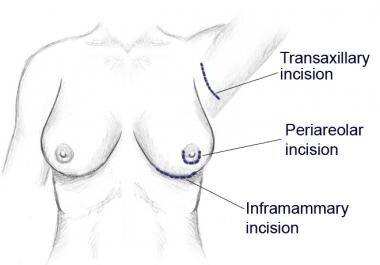
The 5 surgical approaches to placing breast implants include inframammary, periareolar, transareolar, transaxillary, and transumbilical incision.
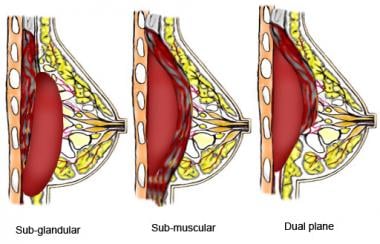
Breast implants can be placed either subglandular, submuscular (underneath the pectoralis muscle), or in a dual plane with the superior part of the implant being covered by muscle and the inferior part under the gland [4, 5]
Postoperative monitoring
In general, most companies guarantee breast implants for 10 years in case of rupture. According to FDA recommendations, asymptomatic patients with silicone gel implants should undergo their first ultrasonogram or magnetic resonance imaging (MRI) scan to screen for rupture 5-6 years after surgery, with screening repeated every 2-3 years. An MRI scan is recommended for patients who are symptomatic or have equivocal ultrasonographic results. [6]
With saline implants, patients should proceed with their recommended mammography protocol for breast cancer screening. Moreover, they can develop capsular contracture over time, and women should return to the plastic surgeon regarding any concerns or questions regarding this.
Types of complications
In general, complication rates are almost always higher in breast reconstruction than in primary cosmetic surgery. A retrospective study by Theunissen et al indicated that in patients undergoing post-mastectomy implant-based breast reconstruction (IBBR), the complication and tissue expander/implant explantation rates of the one-stage procedure were comparable to those for the two-stage operation. However, patients who underwent prophylactic, as opposed to therapeutic, mastectomy were an exception, with the explantation rate after one-stage IBBR surgery being higher than for the two-stage procedure (odds ratio = 4.49). [7]
Capsular contractures
Studies offer contrasting findings regarding the risk of capsular contracture with different breast implant design features. For example, some reports indicate decreased capsular contracture rates with textured implants relative to smooth implants, such as in cases of macro-textured implants [8, 9] (including subglandular textured implants), [10] but not in cases of medium- or micro-textured ones [8] or submuscular textured implants. [11]
Other studies, however, found no significant difference between smooth and textured implants in the subglandular plane [12] or between smooth and large-pore textured saline implants. In addition, in the setting of irradiated, reconstructed breasts, the capsular contracture rate remained quite high, even with textured implants. [13]
Other complications
In addition to capsular contractures, the following complications may arise following breast implant procedures:
-
Hematoma: Blood collection within the breast that often causes localized swelling and pain necessitates evacuation
-
Seroma: Thin fluid collection around the implant
-
Wound infection: Most commonly due to Staphylococcus aureus from the skin or lactiferous ducts but also owing to more rare pathogens such as Candida albicans, Curvularia spp , Aspergillus niger, mycobacteria, and Clostridium perfringens
-
Changes in nipple and/or breast sensation: Hypersensitivity or hyposensitivity
-
Implant rupture: Incidence of about 5-10% at 10 years
-
Issues with lactation: Difficulty breastfeeding in up to 20% of women [14]
-
Anaplastic large T-cell lymphoma of the breast: Rare [15]
-
Pain
-
Implant displacement [16]
-
Implant rippling
Products
Breast implants are designed for use in cosmetic enhancement and reconstruction. They come in many different shapes, sizes, projections, and textures and with different fill materials.
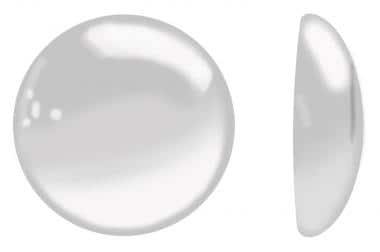
Saline breast implants contain a silicone outer shell filled with sterile saline. Certain implants are empty and thus are filled during the procedure of implantation; others come pre-filled. Saline-filled implants come in different sizes and have either smooth or textured surfaces to their shells. Integrated remote-fill ports can be used and permit postoperative adjustment of implant saline volume. These devices are FDA approved for breast augmentation in women aged 18 years or older and for breast reconstruction in women of any age.
Silicone gel–filled breast implants have a silicone outer shell filled with silicone gel of varying consistencies. They come in different sizes and come with either smooth or textured shells. Silicone gel–filled breast implants are approved for breast augmentation in women aged 22 years or older and for breast reconstruction in women of any age.
The surgeon and patient can select from various implant projection profiles depending on their cosmetic goals.
In 2020, according to the ASPS, silicone gel implants were used in 84% of breast augmentations, and saline implants were used in 16%. [2]
Category
Breast implants are FDA class III devices (ie, they require premarket approval).
Device Details
US manufacturers of breast implants include Mentor Worldwide (Irvine, CA), Allergan (Irvine, CA), Sientra (Santa Barbara, CA), and Ideal Implant (Dallas, TX). [17, 18] (See the images below.)
Design Features
Saline versus silicone gel
Saline implants have the advantage of decreased cost compared with silicone-filled products. Some products can also be filled from a distant port, which enables a surgeon to place them through a transumbilical approach. Moreover, if implant rupture occurs, this is usually more quickly recognizable. In patients with thin breast tissue, however, a higher chance exists that implant rippling will be visible on the surface of the augmented breast.
In contrast, silicone implants cost more but are widely believed to have a feel that is more natural, and rippling in thin-skinned augmentations is less noticeable. While placement of silicone implants through a transumbilical incision has been reported, the fact that they are pre-filled typically discourages such an approach, although they can still be implanted through periareolar, inframammary, or transaxillary incisions.
A literature review by Balk et al indicated that evidence for the long-term health effects of silicone gel breast implants is still inconclusive, with the evidence in many studies applying to breast implants in general and not specifically to the silicone gel type. However, a possible relationship was seen between silicone gel implants and a decreased risk for primary breast and endometrial cancers, as well as an increased risk for lung cancer, rheumatoid arthritis, Sjögren syndrome, and Raynaud syndrome. [19, 20]
Textured versus smooth
Textured versus smooth relates to the implant surface type and is a highly debated topic with regard to its effect on capsular contracture. In theory, textured surface implants may decrease capsular contracture. The mechanism is thought to be the byproduct of breast capsule growth onto the implant surface, which, because of its texture, encourages disorganization of capsular fibres and thus also the resultant force vectors of contracting fibers.
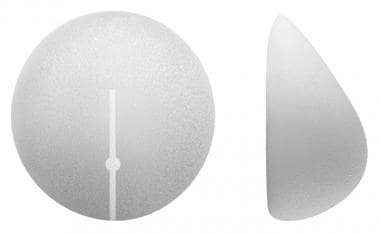
Round versus anatomic
Experience with anatomically shaped implants is evolving. Theoretically, these implants may provide a more natural shape to the augmented or reconstructed breast. Thus far, there does not appear to be a large cosmetic advantage to the use of teardrop-shaped implants in the breast reconstruction patient, but they might be more useful in certain cosmetic cases. The potential disadvantage to these implants is that they can rotate within the breast capsule and leave the patient with an inferior cosmetic outcome.
Adjustable implants
The novel advantage of these devices is that they permit surgeons to adjust the implant size up to 12 months postoperatively (see the image below). This is particularly helpful if a woman is unsure about what size breast she desires. Size change is accomplished via saline injection into a subcutaneous injection port or through an exteriorized injection port. The exteriorized port needs to be inserted by way of a long subcutaneous tunnel to prevent retrograde infection and should be removed within 1 week postoperatively.
Indications
Saline implants are indicated for breast augmentation in women aged 18 years or older and for breast reconstruction in women of any age.
Silicone implants are indicated for breast augmentation in women aged 22 years or older and for breast reconstruction in women of any age.
Clinical Evidence
A study in the English literature has shown decreased capsular contracture rates with macro-textured implants but not with medium- or micro-textured ones. [8] In a clinical meta-analysis of subglandular implants, textured implants were associated with less capsular contracture at 1 year (relative risk, 4.16; 95% CI, 1.58 to 10.96), 3 years (relative risk, 7.25; 95% CI, 2.42 to 21.69), and 7 years (relative risk, 2.98; 95% CI, 0.86 to 10.37) of follow-up. [10]
Another meta-analysis noted an 81% risk reduction for contracture with textured implants, except in the case of submuscular implants, which showed no statistically significant difference. [11] In the international literature, a meta-analysis of textured versus smooth implants indicated a lower capsular contracture rate with the former at 1 or 10 years after breast augmentation. [9] A literature review by Liu et al also reported that textured implants reduce the likelihood of capsular contracture. [21]
Despite these studies, literature that describes no significant difference between smooth and textured implants in the subglandular plane also exists. One particularly convincing article showed no significant contracture difference at 7.5 years between smooth and fine-textured implants. Both devices were placed simultaneously in different breasts of the same patient. [12] In fact, slightly more patients in this study preferred the smooth implants over the textured ones. A similar study by the same group showed no difference between smooth and large-pore textured saline implants. In the setting of irradiated, reconstructed breasts, the capsular contracture rate remains quite high, even with textured implants. [13]
Smooth Spectrum implants have an extremely low rupture rate of 1.1% over 7 years, which is likely due to the valve competence. This is compared with 2-3% for other smooth saline implants and 12% for textured saline implants. [22] In a study of 322 cases using the smooth Spectrum implant for breast reconstruction over 14 years, 19% developed capsular contracture, 5% had seroma or hematoma, and 2% had periprosthetic infection. [23]
In a study evaluating the cosmetic use of Spectrum implants, 9% of patients had saline volume reduced, and 79% had volume added postoperatively. [24] Patients were grateful to be able to continue to participate in the size decision-making process after surgery. The only difficulty noted in this study was a periprosthetic seroma that caused confusion as to whether volume should be added, removed, or left alone. For this reason, all patients should have drains when using the exteriorized port, since the breast size decision must be made within a week after surgery, before the port is removed.
Clinical Implementation
Surgical incisions
Breast implants can be placed surgically through a variety of incisions, each with associated advantages and disadvantages. The approaches include inframammary, periareolar, transareolar, transaxillary, and transumbilical incisions.
Inframammary approach
The inframammary (IM) approach uses an incision at the inferior fold of the breast. The incision is hidden under the breast mound but can be visible. It enables the surgeon good control and flexibility with implant pocket creation and device placement of all sizes.
Periareolar approach
The periareolar (PA) approach involves an incision along the inferior half of the outer circumference of the nipple. This incision can be better hidden than that of the inframammary method but can potentially lead to some hypopigmentation compared with the darker color of the areola. If this occurs and is bothersome, a medical tattoo can be used to change the color. This incision provides good access to adjust the inframammary fold and can be incorporated into a simultaneous mastopexy procedure (see the images below).
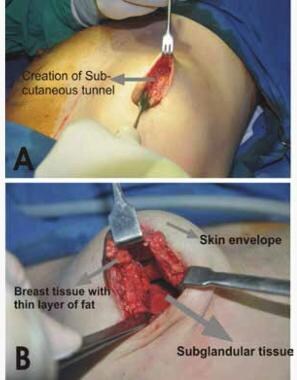 These images of the periareolar approach to breast implant surgery demonstrate the creation of a subglandular pocket. Courtesy of the World Journal of Plastic Surgery (https://wjps.ir/article-1-71-en.html).
These images of the periareolar approach to breast implant surgery demonstrate the creation of a subglandular pocket. Courtesy of the World Journal of Plastic Surgery (https://wjps.ir/article-1-71-en.html).
Compared with the IM approach, however, the periareolar incision can limit exposure for pocket dissection as well as the size of the silicone implant that can be placed. The latter potential difficulty can be abetted with the use of a funnel system. Moreover, the proximity of the incision to the incised lactiferous ducts raises the bacterial contamination risk for the implant. This might, in turn, raise the risk of capsular contracture and implant infection, although the data regarding these problems are controversial.
Some controversy exists regarding changes in nipple sensation in terms of both hypersensitivity and hyposensitivity, following breast augmentation. The nipple and areola are innervated by the lateral and anterior cutaneous branches of the second to fifth intercostals nerves, which subsequently join the subdermal plexus. Many surgeons have had more concern with the PA incision, theoretically because of the proximity of the incision to the nipple. However, a study has shown that the only difference between the IM and PA incisions is a decreased sensation at the inferior pole of the breast. When changes occur, sensation usually returns after 6 months. Patients who were most affected by sensory changes were over age 35 years. [25]
Transareolar approach
The transareolar approach has similar advantages and disadvantages to the PA approach. This incision can be hidden well in a wrinkle within the nipple-areola complex.
Transaxillary approach
The transaxillary technique involves a short transverse incision in the axilla (see the image below). Although some surgeons may use this approach routinely, it might be best suited for patients with a poorly defined inframammary fold and small areolar diameter. Although the incision is hidden well, the disadvantages of this technique are that implants can tend to ride high on the chest wall, placing large silicone implants without the use of a funnel device can be challenging, and controlling the inframammary fold precisely can be difficult. With the assistance of endoscopic equipment, however, one study noted a decrease in the incidence of implant malposition from 8.6% to 2%. [26]
Tebbetts also showed that his Baker 3/4 capsular contracture rates (see Complications) were lower, with 4.2% versus 1.3% for blunt and endoscopic dissection, respectively. [27] If any revision surgery needs to be done in the future, the surgeon usually needs to place an incision in a different location on the breast. This approach also carries the risk of injury to the intercostobrachial and medial brachial cutaneous nerves, which supply sensation to the distal medial portion of the arm.
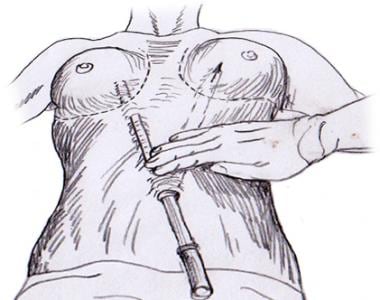
Transumbilical approach
The transumbilical approach hides the incision remotely through the umbilicus. Access to the breasts is gained with long, blunt dissection instruments without the ability to visualize the breast pockets. Saline implants are subsequently inserted through tubes into the breasts and filled to the desired sizes. The major disadvantages of this approach compared to other methods are that control of the inframammary fold position is unreliable, silicone implants are unable to be placed, and a second incision is needed when revision breast surgery is required. This technique is also not ideal for patients who are extremely thin or who have abdominal scars or hernias (see the image below).
Surgical dissection planes
Implants can be placed either subglandular, submuscular (underneath the pectoralis muscle), or in a dual plane with the superior part of the implant being covered by muscle and the inferior part under the gland.
Subglandular (prepectoral) augmentation does an excellent job of restoring breast shape and, compared with subpectoral dissection, may be a more powerful tool to correct minor breast ptosis. The disadvantage is that, in patients with little breast tissue or soft tissue cover, a higher incidence of visualization of the external contour and rippling of the implant may occur.
Submuscular (subpectoral) augmentation carries the advantage of lower capsular contracture rates and thicker soft tissue coverage to minimize the appearance of ripples. The down side is that patients who have well-developed pectoralis muscles may show animation ("dancing") of the implants upon muscle flexion. The implant can also ride high or migrate laterally over time.
The dual plane technique combines the advantages of the above two dissection methods. Soft tissue coverage is improved at the superior pole of the breast, with an associated low contracture rate and with less of a problem with implant animation and the "double bubble" deformity that occurs when the gland slides inferiorly off of the implant (see the image below).
Follow-up / Monitoring
Breast implants are not lifetime devices, but most companies guarantee them for 10 years in case of rupture. Saline implant rupture is often more easily detected on physical examination than silicone implant rupture. Therefore, according to FDA recommendations, asymptomatic patients with silicone gel implants should undergo their first ultrasonogram or magnetic resonance imaging (MRI) scan to screen for rupture 5-6 years after surgery, with screening repeated every 2-3 years. An MRI scan is recommended for patients who are symptomatic or have equivocal ultrasonographic results. [6] With saline implants, patients should proceed with their recommended mammography protocol for breast cancer screening. Moreover, they can develop capsular contracture over time and should return to the plastic surgeon regarding any concerns or questions about this.
Complications
Capsular contracture
With capsular contracture, a shell develops around the breast implant as healing occurs; over time, it may become firm and even painful. The Baker scale is a grading system from 1 to 4, as follows.
-
Grade 1 - Soft breast in which the implant and capsule are not noticeable
-
Grade 2 - Minimally palpable implant and capsule
-
Grade 3 - Firm breast and capsule, in which the implant can be palpated and distortion may be seen
-
Grade 4 - Firm, painful, and tender breast with significant visible breast distortion
See previous sections for more specific information related to breast implant techniques and types and their effects on capsular contracture.
Hematoma
Hematoma is a blood collection within the breast that often causes localized swelling and pain, necessitating evacuation. This was reported to occur at a rate of anywhere from 3% in a study of 600 breast augmentations [28] to 0.9% of implants in a review of 3474 breasts. [29] The incidence of this problem is not associated with any particular surgical approach, patient characteristic, or implant type.
Seroma
Seroma refers to a thin fluid collection around the implant. These usually resolve by themselves in a few days. When they do not, they can be aspirated under ultrasonographic guidance, but this procedure can carry a risk of damaging the implant. Closed suction drains should be used when implants are placed in conjunction with acellular dermal matrix as the hematoma rate is significantly greater in this setting.
Seromas rarely occur more than 1 year postoperatively (in 0.1% of cases). [30] They are noticeable by asymmetrical breast swelling and may be due to mechanical friction between prosthesis and capsule or implant biofilm formation. Seromas can also occur in the setting of infection, so fluid should be aspirated under ultrasonographic guidance and sent for culture. In a patient with a history of breast cancer, the appearance of a late seroma should raise particular concern for tumor recurrence, and fluid should be sent for cytologic analysis.
Wound infection
Wound infection is most commonly due to Staphylococcus aureus bacteria from the skin or lactiferous ducts. Infection can also be caused by more rare pathogens such as Candida albicans,Curvularia spp ,Aspergillus niger, mycobacteria, and Clostridium perfringens. One study reported the infection rate to be 2.2% in 899 breast augmentation cases. [31]
Changes in nipple sensation
Hypersensitivity and hyposensitivity of the nipple and breast can occur after breast implant placement. The incidence of this varies based on different literature series. For more information, please see the section on clinical implementation.
Implant rupture
Saline implant rupture has been reported at 5-10% at 10 years. Silicone implants are often found to have been ruptured at the time of implant exchange for other reasons. One study determined from 478 explanted prostheses a 34% overall rupture rate: 33% for first-generation implants, 65% for second-generation implants, and 9% for third-generation implants. [32] In the case of suspected rupture, imaging studies can be performed to confirm this occurrence, and the implant can subsequently be replaced (see the image below).
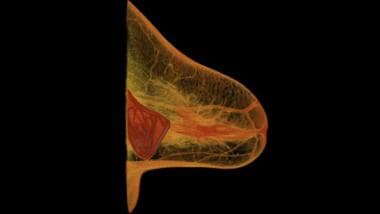 A computed tomography (CT) scan reveals a breast implant rupture. Courtesy of Wikimedia Commons (author Rsmskns) (https://commons.wikimedia.org/wiki/File:Implant_rupture.png).
A computed tomography (CT) scan reveals a breast implant rupture. Courtesy of Wikimedia Commons (author Rsmskns) (https://commons.wikimedia.org/wiki/File:Implant_rupture.png).
Lactation
Up to 1 out of every 5 women may have difficulty breastfeeding after implant-based augmentation. [14]
Current evidence does not support causality between breast implants and breast cancer or connective tissue diseases. Moreover, no evidence shows an increased risk of health problems for breastfeeding children. In fact, one study demonstrated that the mean silicon level in cow’s milk and commercially available infant formulas was significantly higher than in silicone implant associated breast milk. [33]
Anaplastic large T-cell lymphoma
Anaplastic large T-cell lymphoma of the breast has been identified as having a potential association with breast implants. [15] (By early January 2020, 733 cases of breast implant–associated anaplastic large T-cell lymphoma had been identified worldwide. [34] ) Fortunately, this disease is not only rare but can often be treated with less complexity than primary breast cancer. Current recommended treatment for implant-associated anaplastic large T-cell lymphoma is capsulectomy and implant removal.
The risk of anaplastic large T-cell lymphoma has been found to be higher with textured breast implants than with smooth ones. [35] In a survey sent to active and candidate members of The Aesthetic Society (470 responses), Frojo et al determined that with regard to patients with textured implants who are asymptomatic but have concerns about the lymphoma, 11.2% of surgeons recommend that the implant be removed, while 88.8% respond by educating the patient, with clinical follow-up and/or imaging included. [36]
In 2019, at the FDA’s request, Allergan issued a voluntary recall of its Biocell textured breast implants and tissue expanders, with the FDA having found evidence that the risk of breast implant–associated anaplastic large T-cell lymphoma was about six times greater with the recalled implants than with other textured implants being marketed in the United States. [37]
Pain, implant displacement, and implant rippling
As previously described in this article, pain, implant displacement, and implant rippling can occur.
Breast implant illness
In a small number of cases, women have experienced what has come to be known as breast implant illness, the signs and symptoms of which can include, but are not limited to, the following [38, 39, 40, 41, 42, 43] :
-
Anxiety or depression
-
Brain fog
-
Chronic fatigue
-
Dry mouth and dry eyes
-
Gastrointestinal problems
-
Hair loss
-
Headaches
-
Joint or muscle pain
-
Rashes and skin problems
-
Weight changes
As an entity, however, the existence of breast implant illness remains to be proven, with the literature concerning this condition being, to a great extent, observational and descriptive. [44]
A study by Magno-Padron et al found that in women who, as surveyed, suffered from apparent breast implant illness and had their implants removed, 97% experienced complete (23%) or partial (74%) symptom relief. [45]
A study by Peters et al of 100 women with breast implants showed that, after explanation, patients with more generalized complaints like fatigue improved. However, those who had rheumatologic complaints either did not improve or improved only for a short period of time. This could be interpreted to mean either that the rheumatologic symptoms were too strong at that point to be overcome by explantation or that those symptoms were unassociated with the implants. The patients in this report underwent explantation for a variety of reasons, with, for example, 76% suspecting that they were experiencing silicone-related health problems, 59% being anxious over possible implant rupture, 36% suffering from breast pain, and 23% experiencing musculoskeletal pain. [46]
This study was performed in the 1990s and so involved a different generation of implants, not those with the newer, more cohesive gels. Plastic surgeons are working hard on more detailed studies regarding the symptoms that can occur, albeit infrequently, in persons who receive breast implants, including which cases might have a connection to the implants themselves and what treatment plans can best help patients. [46]
-
Sientra teardrop-shaped implant.
-
Sientra round, smooth implant.
-
Shaped oval implant.
-
Shaped classic implant.
-
Textured round implant.
-
Periareolar, inframammary, and transaxillary approaches to breast augmentations.
-
Subglandular, submuscular, and dual-plane breast implant placement.
-
Transumbilical approach to breast augmentation.
-
Mentor Spectrum adjustable saline implant with associated fill port.
-
A computed tomography (CT) scan reveals a breast implant rupture. Courtesy of Wikimedia Commons (author Rsmskns) (https://commons.wikimedia.org/wiki/File:Implant_rupture.png).
-
These images of the periareolar approach to breast implant surgery demonstrate the creation of a subglandular pocket. Courtesy of the World Journal of Plastic Surgery (https://wjps.ir/article-1-71-en.html).