Practice Essentials
The maxilla represents the bridge between the cranial base superiorly and the dental occlusal plane inferiorly. Its intimate association with the oral cavity, nasal cavity, and orbits and the multitude of structures contained within and adjacent to it make the maxilla a functionally and cosmetically important structure. Fracture of these bones is potentially life-threatening as well as disfiguring. [1] Timely and systematic repair of these fractures provides the best chance to correct deformity and prevent unfavorable sequelae. [2]
Signs of maxillary fractures
In general, patients with facial fractures have obscuration of their bony architecture with soft tissue swelling, ecchymoses, gross blood, and hematoma. Nonetheless, observation alone may be informative. Focal areas of swelling or hematoma may overlie an isolated fracture. Periorbital swelling may indicate Le Fort II or III fractures. A global posterior retrusion of the midface creates a flattened appearance of the face. The so-called dish-face or pan-face deformity may occur after an extensive Le Fort II or Le Fort III fracture. The maxillary segment is displaced posteriorly and inferiorly. This may cause premature contact of the molar teeth, resulting in an anterior open bite deformity. In severe cases, the upper airway may be compromised.
Workup of maxillary fractures
Computed tomography (CT) scanning is the imaging modality of choice for facial fractures. [3] CT scans are superior to plain films for delineating multiple fractures, evaluating associated cartilaginous or soft tissue injury, and assessing for the presence of impingement into the optic canal.
Management of maxillary fractures
Fixation of unstable fracture segments to stable structures is the objective of definitive surgical treatment of maxillary fractures.
In general, attempt to complete restoration of dental occlusion with maxillomandibular fixation (MMF) prior to reduction and fixation of other segments of the maxilla. MMF accurately restores the position of the base of the maxilla, allowing for correct reconstruction from inferior to superior. If the mandible is also fractured, reduction and fixation of the mandible must be completed first, followed by MMF and then definitive repair of maxillary fractures.
Epidemiology
Frequency
Maxillary fractures account for approximately 6-25% of all facial fractures. In a retrospective study of pediatric midface fractures, Kao et al found that maxillary fractures were the most common. Out of 410 total pediatric midface fractures (218 patients), 125 (30.5%) were maxillary, with 34 of the maxillary fractures being of the nasal/frontal process alone, with no sinus involvement. [4]
A retrospective study by Moffitt et al at a level 1 trauma center found that 69 out of 1274 pediatric patients (5.4%) with facial fractures presented with Le Fort fractures. [5]
Regarding patient environment, a study by Cohn et al indicated that, compared with the overall US population, urban patients who sustain maxillofacial trauma have less tendency to suffer maxillary and multiple fractures and are more likely to experience mandibular and orbital fractures. [6]
Etiology
Maxillary fractures often result from high-energy blunt force injury to the facial skeleton. Typical mechanisms of trauma include motor vehicle accidents, altercations, and falls. [7] With increased legislation requiring seat belt use, injuries from driver impact with the steering wheel have shifted from chest trauma to facial trauma.
In the above-mentioned study by Moffitt et al of pediatric patients with facial fractures, odds ratios (ORs) for Le Fort fractures were higher in association with increased age (OR 1.1) and concomitant orbital fracture (OR 8.33), with motor vehicle collisions also being an associated factor. [5]
Pathophysiology
Much of the understanding of patterns of fracture propagation in midface trauma originates from the work of René Le Fort. In 1901, he reported his work on cadaver skulls that were subjected to blunt forces of various magnitudes and directions. He concluded that predictable patterns of fractures follow certain types of injuries. Three predominant types were described. [8]
-
Le Fort I fractures (horizontal) may result from a force of injury directed low on the maxillary alveolar rim in a downward direction. The fracture extends from the nasal septum to the lateral pyriform rims, travels horizontally above the teeth apices, crosses below the zygomaticomaxillary junction, and traverses the pterygomaxillary junction to interrupt the pterygoid plates. See the image below.
-
Le Fort II fractures (pyramidal) may result from a blow to the lower maxilla or midmaxilla. Such a fracture has a pyramidal shape and extends from the nasal bridge at or below the nasofrontal suture through the frontal processes of the maxilla, inferolaterally through the lacrimal bones and inferior orbital floor and rim through or near the inferior orbital foramen, and inferiorly through the anterior wall of the maxillary sinus; it then travels under the zygoma, across the pterygomaxillary fissure, and through the pterygoid plates. See the image below.
-
Le Fort III fractures (transverse), also termed craniofacial dysjunctions, may follow impact to the nasal bridge or upper maxilla. These fractures start at the nasofrontal and frontomaxillary sutures and extend posteriorly along the medial wall of the orbit through the nasolacrimal groove and ethmoid bones. The thicker sphenoid bone posteriorly usually prevents continuation of the fracture into the optic canal. Instead, the fracture continues along the floor of the orbit along the inferior orbital fissure and continues superolaterally through the lateral orbital wall, through the zygomaticofrontal junction and the zygomatic arch. Intranasally, a branch of the fracture extends through the base of the perpendicular plate of the ethmoid, through the vomer, and through the interface of the pterygoid plates to the base of the sphenoid. See the image below.
In reality, the Le Fort classification is an oversimplification of maxillary fractures. The amount of force impacted during a motor vehicle accident is much greater than Le Fort took into consideration during his work in the late 19th century. In most instances, maxillary fractures are a combination of the various Le Fort types. Fracture lines often diverge from the described pathways and may result in mixed-type fractures, unilateral fractures, or other atypical fractures. [9] In addition, in very high-energy blows, maxillary fractures may be associated with fractures to the mandible, cranium, or both (ie, panfacial).
A retrospective study by Roumeliotis et al of 39 Le Fort fractures indicated that Le Fort I fractures caused by a high-velocity impact (ie, impact from a fall from more than 1 story or a motor vehicle collision) occur higher on the lateral buttress than do those caused by a low-velocity impact (ie, impact from a fall from stranding height or an assault with a blunt weapon or closed fist). [10]
Two types of non–Le Fort maxillary fractures of note are relatively common. First, limited and very focused blunt trauma may result in small, isolated fracture segments. Often, a hammer or other instrument is the causative weapon. In particular, the alveolar ridge, maxillary sinus anterior wall, and nasomaxillary junction, by virtue of their accessibility, are common sites of such injury. Second, submental forces directed superiorly may result in several discrete vertical fractures through various horizontal bony supports such as the alveolar ridge, infraorbital rim, and zygomatic arches.
Unlike with fractures in other bones, muscle forces do not play a significant role in the final position of the broken bony segments. While several muscles attach to the maxillary framework, they typically insert to skin and therefore do not lead to additional deformity. Instead, the basis for the patterns of maxillary fractures depends on 2 predominant factors.
First, as Le Fort described, the location, direction, and energy of the impact result in different injuries. Second, the anatomy of the midface is oriented to provide strength and support to protect against injury. Vertical and horizontal bony bolstering in the face absorbs the energy of traumatic force. This serves to protect the more vital intracranial contents from damage during trauma. Knowledge of the characteristics of the traumatic blow combined with an understanding of the anatomic bolstering in the face can help the clinician approach such injury in a logical and systematic fashion. A detailed description of the bony maxillary framework is presented in Relevant Anatomy.
A retrospective study by Mundinger et al indicated that Le Fort I fractures, as well as complex midface fractures, subcondylar fractures, and bilateral fractures in any facial third, increase the risk for blunt internal carotid artery injuries. The study, which included 4398 patients, found this to be especially true for those fractures associated with basilar skull fractures. [11]
A literature review by Kelts et al indicated that mandibular and Le Fort fractures are the isolated craniomaxillofacial (CMF) injuries that are most regularly associated with blunt cerebrovascular injury (BCVI). The investigators found that in patients with BCVI, mandibular and maxillary fractures made up 12.5% and 11.8% of CMF fractures, respectively. [12]
Presentation
History
Information regarding the mechanism of the injury may assist in determining a diagnosis. In particular, knowing the magnitude, location, and direction of the impact is helpful. High-energy trauma should cause concern about other possible concomitant injuries. A history of mental status changes or loss of consciousness should cause concern regarding intracranial injury. The presence of any functional deficiencies, such as those related to airway, vision, cranial nerves, occlusion, or hearing, may provide clues to fracture location and resultant adjacent nonosseous injury.
Physical examination
Evaluation of the maxilla and facial bones should be undertaken only after the patient has been fully stabilized and life-threatening injuries have been addressed. In particular, airway considerations and intracranial injuries must take immediate priority.
In general, patients with facial fractures have obscuration of their bony architecture with soft tissue swelling, ecchymoses, gross blood, and hematoma. Nonetheless, observation alone may be informative. Focal areas of swelling or hematoma may overlie an isolated fracture. Periorbital swelling may indicate Le Fort II or III fractures. A global posterior retrusion of the midface creates a flattened appearance of the face. The so-called dish-face or pan-face deformity may occur after an extensive Le Fort II or Le Fort III fracture. The maxillary segment is displaced posteriorly and inferiorly. This may cause premature contact of the molar teeth, resulting in an anterior open bite deformity. In severe cases, the upper airway may be compromised. In such a situation, disimpaction forceps may need to be placed into the nasal floor and hard palate to pull the bony segment forward to restore airway patency.
The face and cranium should be palpated to detect for bony irregularities, step-offs, crepitus, and sensory disturbances. Mobility of the midface may be tested by grasping the anterior alveolar arch and pulling forward while stabilizing the patient with the other hand. The size and location of the mobile segment may identify which type of Le Fort fracture is present. If only an isolated segment of bone is mobile, a small alveolar or nasofrontal process chip fracture may be present. With high-impact force, the maxilla may be comminuted or impacted, in which case the bony framework is displaced or crushed but immobile.
A thorough nasal and intraoral examination should be completed. The nasal bones are typically quite mobile in Le Fort II fractures, along with the rest of the pyramidal free-floating segment. Intranasal examination may reveal fresh or old blood, septal hematoma, or cerebrospinal fluid rhinorrhea. The intraoral examination should assess occlusion, overall dentition, stability of the alveolar ridge and palate, and soft tissue. Finger palpation of the maxillary contour intraorally may provide additional information about the integrity of the nasomaxillary buttress, anterior maxillary sinus wall, and zygomaticomaxillary buttress.
During examination of the eyes and orbit, search for integrity of the orbital rims, orbital floor, vision, extraocular motion, position of the globe, and intercanthal distance. Unlike Le Fort II fractures, Le Fort III fractures are associated with lateral rim and zygomatic breaks. Visual changes may signify a disturbance of the optic canal, problems within the globe or retina, or other neurologic lesions. Disturbances of extraocular motion or enophthalmos may signify a blowout in the orbital floor. An increased intercanthal distance implies displacement of the frontomaxillary or lacrimal bones or avulsion of the medial canthal ligament. For extensive involvement of the orbit or globe, consultation with an ophthalmologist is appropriate.
Tools that may assist the examiner in the evaluation of maxillofacial trauma include a headlamp or mirror, tongue blades, a suction device, a nasal speculum, an otoscope, and a ruler. Early photographs may be helpful in preoperative planning and patient counseling.
Indications
Extensive maxillary fractures are usually associated with significant cosmetic and functional sequelae. Expeditious definitive therapy is needed to best correct these problems. Thus, most significant maxillary fractures should be reduced and repaired surgically. Exceptions may apply to very localized fractures that do not present significant deformity or functional disturbance (eg, small anterior maxillary wall fracture).
Relevant Anatomy
The maxillary bones are paired pyramidal bones that in many ways serve as the cornerstones of the facial skeleton. In a superoinferior direction, the maxilla bridges the cranial-frontoethmoid complex above to the mandible and to the occlusal plate below. In a transverse plane, it bridges the 2 zygomaticoorbital complexes.
Each individual maxilla can be conceptualized as a 5-sided structure, the base of which makes up the lateral nasal wall. The remaining 4 sides of the pyramid are composed of the orbital floor superiorly, the alveolar ridge inferiorly, the front wall of the maxillary sinus anteriorly, and the anterior face of the pterygopalatine fossa posterolaterally.
The maxilla and the associated bones of the midface are oriented to resist the vertical forces of mastication. This is accomplished through 3 paired vertical buttresses (from anteromedial to posterolateral): the nasomaxillary buttress, the zygomaticomaxillary buttress, and the pterygomaxillary buttress. An additional unpaired midline support is the frontoethmoid-vomerine buttress. These pillars serve to diffuse the vertical forces of mastication over the broad cranial base. They are also effective shock absorbers for a vertically oriented impact to the facial skeleton.
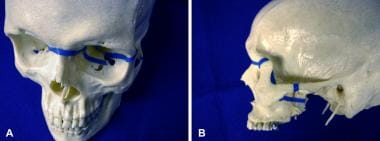
The nasomaxillary buttress transmits force from the maxillary canine area through the lateral pyriform rim and frontal process of the maxilla and to the superior orbital rim. The zygomaticomaxillary buttress transmits forces from the zygomatico-alveolar crest through the zygoma to the posterior aspect of the superior orbital rim and temporal bone. The pterygomaxillary buttress conducts force through the palatine bone to the pterygoid plates and sphenoid base. See the image below.
The superior and inferior orbital rims and alveolar ridge constitute a group of weaker horizontal buttresses. While these structures provide some protection against horizontal forces, they can withstand much less force than the vertical buttresses. Therefore, vertical impact tends to be better absorbed within the facial skeleton, which resists fracture, while horizontal impact tends to overcome the weaker horizontal buttresses and shear through the vertical pillars. In a surgical approach to maxillary fractures, attempts should be made to restore the continuity of these support buttresses. See the image below.
Several important nonosseous structures are closely associated with the maxilla and thus may be damaged during injury or repair.
-
The infraorbital nerve travels through the inferior orbital fissure and exits from the infraorbital foramen just below the inferior rim. Therefore, anesthesia of the cheek and upper teeth is commonplace in persons with extensive fractures.
-
Branches of the internal maxillary artery provide much of the vascular supply to the midface. In 2009, Bozkurt et al reported a case of pseudoaneurysm of this artery after a subcondylar fracture. [13] In patients with extensive epistaxis or bleeding, ligation of this artery may be necessary. [14] Redundant anastomoses from other branches of the internal and external carotid circulation ensure that vascular insufficiency of the maxilla is unlikely, even with internal maxillary artery ligation.
-
Orbital contents such as the lacrimal system, extraocular muscles, optic nerve, and globe are in close proximity to the maxilla and are therefore susceptible to injury.
Contraindications
Definitive surgery should not be undertaken until the patient has been stabilized regarding other life-threatening injuries. Patients with airway compromise should not be induced for general anesthesia and routine orotracheal intubation. Disimpaction of retrodisplaced facial bony segments or tracheotomy while the patient is awake should be considered before surgery. As for any procedure, the risks of general anesthesia and the stresses of surgery must be weighed against medical contraindications (eg, cardiac, pulmonary). Although treatment of maxillary fractures is not considered vital for survival, unrepaired fractures can potentially lead to significant functional and cosmetic complications.
-
Typical Le Fort I fracture pattern.
-
Typical Le Fort II fracture pattern.
-
Typical Le Fort III fracture pattern.
-
Vertical buttresses of facial skeleton.
-
Horizontal buttresses of facial skeleton.
-
(A) Axial CT scan. Note that determining whether the vertical buttresses have been compromised is difficult using the axial image. (B) Coronal CT scan. This view demonstrates fractures through the nasomaxillary and zygomaticomaxillary buttresses. (C) Coronal CT scan. This more posterior view demonstrates fractures through the pterygoid plates.
-
Cadaver demonstration of sublabial approach to rigid titanium plate and screw fixation of Le Fort I fracture.