Background
Fractures of the frontal sinus pose certain treatment dilemmas to the facial trauma surgeon. Their mismanagement may lead to potentially life-threatening intracranial complications, most commonly meningitis, encephalitis, and brain abscess. Other complications include frontal osteomyelitis, frontal bone non-union, cavernous sinus thrombosis, cerebrospinal fluid (CSF) leak, mucopyocele, and meningoencephalocele. [1, 2]
These injuries are currently managed by various medical specialists, including otolaryngologists/head and neck surgeons, maxillofacial surgeons, plastic surgeons, and neurosurgeons. As a result, consensus does not exist regarding the timing, indications, and treatment modality of these injuries. The series reported in the literature have relatively few subjects and, as might be expected, mostly limited follow-up periods.
In the past, roentgenograms were used for diagnosing frontal sinus fractures, although the sensitivity of plain films was well-recognized as not very high. [3] Roentgenography can result in underdiagnosis and is not particularly useful in examining the severity of damage to the posterior table and the nasofrontal duct region. [4]
The use of high-resolution, 1.5-mm axial and coronal thin-cut computed tomography (CT) scanning provides improved diagnostic power for assessing injuries to the frontal sinus and midface [4, 5, 6] and has become invaluable in the diagnosis of frontal sinus fractures. Involvement of the nasofrontal duct is not easily discernible with CT imaging and, as a result, decisions regarding management of the nasofrontal duct and frontal sinus are frequently made during surgical exploration. However, nasofrontal duct injury is strongly suggested when the CT scan demonstrates involvement of the base of the frontal sinus, the anterior ethmoid complex, or both. [4] The nasofrontal duct complex should be evaluated in both the axial and coronal planes.
History of the Procedure
The progression of frontal sinus surgery stems from the first ablative procedure described by Reidel in 1898. [7] He described total exoneration of the sinus by removing the anterior table and floor of the sinus, allowing the skin to overlay the posterior table. This technique created an obvious marked cosmetic defect. In 1904, Killian described a similar procedure, but this procedure left a 10-mm rim of supraorbital bone, improving the cosmetic result. [8]
In 1921, Lynch described the first frontoethmoidectomy, leaving the anterior table intact but completely removing the ethmoid sinuses and the frontal sinus floor. [9] An indwelling catheter was inserted for prolonged drainage.
In 1951, Bergara and Itoiz devised the osteoplastic flap procedure. [10] They described exposure of the sinus by removing the anterior table, but, unlike Reidel, it was left hinged to an inferiorly based pedicle of pericranium. The flap was replaced at the end of the procedure. This technique resulted in a marked improvement in the overall aesthetic result.
In the late 1950s and 1960s, Goodale and Montgomery first described the ablative frontal sinus procedures that are the basis for current surgical obliterative management of frontal sinus fractures. [11, 12, 13] They took the osteoplastic flap procedure one step further, describing methods of ablating the frontal sinus by grossly removing all sinus mucosa and packing it with autogenous fat, essentially eliminating the sinus as a functional unit.
Later work described the involvement of the nasofrontal ducts in chronic complications of frontal sinus trauma, presumably secondary to duct stenosis. [3] It then became clear that simple obliteration as described by Goodale and Montgomery was insufficient to completely prevent the occurrence of late sequelae. The importance of removing any retained mucosa in the region of the nasofrontal duct was stressed. [3, 14] Failure to remove all sinus mucosa and subsequent reepithelialization of the sinus was demonstrated to result in late complications such as mucoceles and mucopyoceles.
Donald and Bernstein described the first cranialization procedure in 1978. [15] It involved stripping the sinus of all mucosa, plugging the nasofrontal ducts, and removing the posterior table, allowing the brain to expand into the frontal sinus space; the procedure thus incorporated the previous frontal sinus space into the anterior cranial vault. This procedure is still used today, but it is usually reserved for patients with severe comminution of the posterior table.
Problem
Frontal sinus fractures can be classified into fractures of the anterior table, the posterior table, or both. Isolated fractures of the posterior table are rare. The fractures may be simple, comminuted, displaced, or nondisplaced. Displacement of anterior table fragments, especially when through the inferior and/or base half of the sinus, can cause obstruction of the nasofrontal duct. [3] Displacement of the anterior table can also lead to depression of the forehead and a cosmetic deformity (see following images).
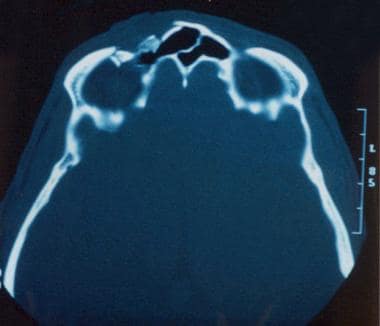 CT scan showing frontal sinus fracture with comminution injury to the anterior table and supraorbital rim. However, the posterior table appears to be intact.
CT scan showing frontal sinus fracture with comminution injury to the anterior table and supraorbital rim. However, the posterior table appears to be intact.
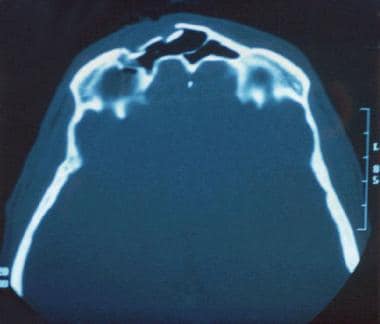 More superior cut of CT scan showing frontal sinus fracture with comminution injury to the anterior table and supraorbital rim. The degree of anterior table displacement was sufficient to cause significant aesthetic deformity. Although the fracture spares the base of the frontal sinus and the posterior wall, the sinuses were explored for nasofrontal duct injury. The ducts were found to be intact. The anterior table was repaired, and no obliteration was performed.
More superior cut of CT scan showing frontal sinus fracture with comminution injury to the anterior table and supraorbital rim. The degree of anterior table displacement was sufficient to cause significant aesthetic deformity. Although the fracture spares the base of the frontal sinus and the posterior wall, the sinuses were explored for nasofrontal duct injury. The ducts were found to be intact. The anterior table was repaired, and no obliteration was performed.
Posterior table fractures usually occur in combination with fractures of the anterior table and are frequently associated with intracranial trauma. When the posterior table is displaced more than the width of the table, the incidence of CSF leak and dural tears is high. Impinged sinus mucosa between fracture segments may lead to the formation of mucoceles. [16] The frequency of nasofrontal duct injury is proportional to the severity and comminution of the frontal sinus fracture. Injuries to the duct are likely when the fracture is medial to the supraorbital notch and involves the base of the frontal sinus and/or the anterior ethmoid complex (see following images). Unrecognized injury to the nasofrontal duct may lead to frontal sinus drainage and aeration obstruction and, eventually, the formation of mucoceles, mucopyoceles, meningitis, and intracranial abscess.
 Fracture of the frontal sinus involving the anterior table and both supraorbital rims, medial to the supraorbital notch.
Fracture of the frontal sinus involving the anterior table and both supraorbital rims, medial to the supraorbital notch.
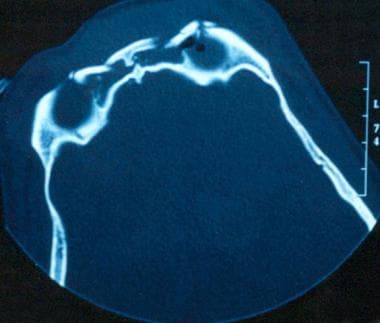
 Lower cut of CT scan in a patient with fracture of the frontal sinus involving the anterior table and both supraorbital rims, medial to the supraorbital notch. Note the fracture extension through the base of the frontal sinus and involvement of the anterior ethmoid complex. Even though the fracture spares the posterior table, damage to the nasofrontal ducts is highly likely.
Lower cut of CT scan in a patient with fracture of the frontal sinus involving the anterior table and both supraorbital rims, medial to the supraorbital notch. Note the fracture extension through the base of the frontal sinus and involvement of the anterior ethmoid complex. Even though the fracture spares the posterior table, damage to the nasofrontal ducts is highly likely.
A study by Garg et al indicated that vertical frontal bone fractures that extend into the frontal sinus and orbit or into the middle or posterior cranial fossa have greater complication and mortality rates than do nonvertical frontal sinus fractures. The study involved 149 frontal bone fractures, including 51 nonvertical frontal sinus fractures and 98 vertical fractures with or without frontal sinus involvement. [17]
Epidemiology
Frequency
Frontal sinus fractures comprise 5-12% of maxillofacial traumas. [3, 18] The incidence appears to be approximately 9 cases per 100,000 adults. [19]
Etiology
Fractures of the frontal sinus occur most commonly as a result of blunt trauma from a motor vehicle accident; the next most common cause is high-impact sports-related injury. [20, 19, 21, 22] Frontal sinus fractures may result from low-velocity, high-velocity, blunt, or penetrating trauma. With low-velocity impact, the anterior table may confer some protection to the posterior table and may be the only table to fracture. Conversely, high-velocity or penetrating trauma may cause severe damage to both the anterior and posterior tables, with comminution and significant displacement. [23]
Pathophysiology
The force required to fracture the frontal sinus has been reported to be 800-2200 lb of force and is usually sufficient to cause significant associated injuries. [24] There is no association between age and the fracture force required. [25]
Presentation
Patients presenting with this type of injury usually have associated craniofacial trauma, which must be treated in an appropriately triaged fashion. Patients may present in a coma 20-76% of the time, depending on the series studied. [19, 22, 23] As many as 93% of patients present with multiple associated facial fractures, skull fractures, or both. [19, 23] In one series, 20% of patients presented with CSF rhinorrhea. [22]
A fracture of the frontal sinus should be considered clinically when a gross depression or laceration is found over the supraorbital ridge, glabella, or lower forehead, as this is the most common finding on clinical examination. [4] Lacerations should be examined gently to determine if any bony step-offs are present. As many as 59% of these patients may present with orbital trauma. [14] Prompt ophthalmologic evaluation may be necessary. A large percentage of patients also may have associated fractures of the naso-orbito-ethmoid complex and midface, which may also suggest involvement of the nasofrontal duct. Gross CSF rhinorrhea may occur if the posterior table of the frontal sinus and the dura are involved in the injury.
Indications
Although the management of frontal sinus fractures is somewhat controversial, certain treatment principles exist that are generally accepted. [26] Surgical treatment, if indicated, should be instituted within the first 12-48 hours after the injury, if this is compatible with the patient's overall clinical condition. Early treatment reduces the incidence of long-term complications [27] and is especially important for patients with CSF rhinorrhea because a significant increase in the rate of infection has been reported in patients in whom CSF leak persisted for more than 8 days. [28]
Isolated anterior table fractures are the most common type of frontal sinus injury (see following images).
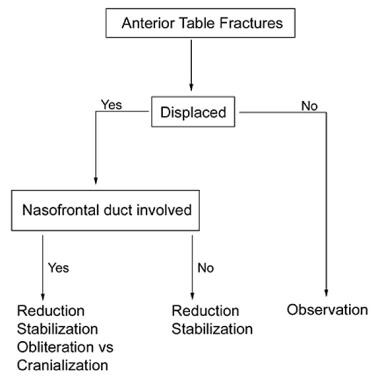 A proposed algorithm for the management of anterior table fractures. Note that in the case of a displaced anterior table fracture with involvement of the nasolacrimal duct, some have also proposed recannulation of the duct.
A proposed algorithm for the management of anterior table fractures. Note that in the case of a displaced anterior table fracture with involvement of the nasolacrimal duct, some have also proposed recannulation of the duct.
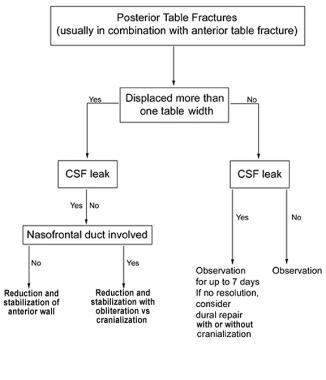 A proposed algorithm for the management of frontal sinus posterior table fractures. In patients with cerebrospinal fluid leak and displacement, obliteration or cranialization is usually indicated. If no cerebrospinal fluid leak is present, the fracture can be reduced and the algorithm for anterior table fractures can be followed. See Image 7.
A proposed algorithm for the management of frontal sinus posterior table fractures. In patients with cerebrospinal fluid leak and displacement, obliteration or cranialization is usually indicated. If no cerebrospinal fluid leak is present, the fracture can be reduced and the algorithm for anterior table fractures can be followed. See Image 7.
Displacement of the fracture and depression of the anterior table are indications for surgical exploration and internal fixation. These fractures can result in cosmetic deformity and mucocele formation, and many consider them to be an absolute indication for surgery, especially if the displaced fracture involves the base of the frontal sinus or the anterior ethmoid complex, as such involvement is associated with a higher likelihood of nasofrontal duct obstruction. The nasofrontal duct can be explored through the existing fracture line or through a frontal trephination with sinus endoscopy. If the nasofrontal duct is involved, sinus obliteration is generally required. [22] If the nasofrontal duct is not involved, internal fixation is performed, and the patient is observed. Isolated, depressed anterior table fractures without nasofrontal duct injury may be percutaneously reduced using a specialized bony tapper device or simply using screws, forceps, and manual traction. This technique may be less invasive and more cosmetically favorable in patients with this simple type of fracture. [29, 30]
Most nondisplaced anterior table fractures can be managed expectantly and nonsurgically, [31] since these fractures are typically not associated with mucocele formation, although they may still result in cosmetic deformity.
Posterior table fractures are commonly associated with anterior table fractures. Treatment is usually dictated by the presence or absence of nasofrontal duct involvement, CSF leak, or both. In the case of posterior table fractures, most would advocate surgery in the presence of displacement more than one table width, and especially in the presence of gross CSF leak and associated dural tears not responding to conservative therapy (eg, bed rest). Many authors elect to closely observe patients presenting with posterior table fractures and CSF leak for 7 days. If observation and conservative management fail, exploration and repair are suggested. [22] Neurosurgical consultation for craniotomy and dural closure would then need to be obtained. Sinus obliteration or cranialization is concurrently performed. [32] Cranialization of the frontal sinus is usually reserved for severely displaced or comminuted fractures of the posterior table. [15, 21] However, a recent 10-year study by Choi et al demonstrated successful, nonoperative management of a majority of comminuted, displaced fractures with or without CSF leak. [33]
Newer protocols involving sinus preservation with endoscopic management of the nasofrontal duct have been described for specific cases. Proponents argue that sinus preservation may decrease morbidity, operative time, and risk of bone devitalization, as well as allowing the surgeon to endoscopically evaluate the sinus postoperatively. Larger studies are needed to evaluate these claims. [34]
The management of nondisplaced posterior sinus wall fractures is more controversial. Some authors suggest that all posterior table fractures should undergo exploration and be examined directly via sinuscopy or otherwise. Others treat these injuries with close observation and explore if complications (persistent CSF leak) develop.
Surgical indications are summarized in the above images.
Relevant Anatomy
The frontal sinuses are not developed at birth. They begin as an invagination of the anterior ethmoid air cells, which can be first appreciated radiographically in individuals aged 6-8 years. [35] Their pneumatization is usually asymmetric and may range from partial to incomplete in approximately 20% of the population. [35] They do not achieve full size until late adolescence. For this reason, fractures of the frontal sinuses are nearly twice as common in the adult population as in the pediatric population. [19]
The frontal sinuses are usually highly variable in size and shape. They are usually characterized by 2 asymmetric sinuses that are separated by a thin, bony septal plate. Hypoplasia of the frontal sinus is relatively common, with 2-20% of the population demonstrating some degree of underpneumatization. The nasofrontal ducts are situated posteromedially in the sinus and are the only drainage pathways of the frontal sinus. These may be absent in as much as 80% of the population; these persons simply have a large opening into the middle meatus.
When present, the ducts usually run caudally for up to 2 cm. Large anterior ethmoid cells, also known as the agger nasi cells, may bulge into the floor of the frontal sinuses and the nasofrontal ducts. Chronic inflammation in the adjacent thin-walled spaces of both the ethmoid and frontal recess air cells may lead to chronic edematous changes in the nasofrontal ducts, causing frontal sinus drainage problems. For this reason, patients with a history of recurrent anterior ethmoid sinusitis may be at higher risk of developing recurrent frontal sinus infections after trauma to the nasofrontal ducts.
Due to the proximity of important anatomic structures, early recognition and treatment of frontal sinus fractures is necessary. Inferiorly and posteriorly, the sinuses are in close apposition to the dura mater, frontal lobes, crista galli, and cribriform plate, usually separated only by a thin, bony plate. The anterior-superior portion of the sinuses is composed of the sturdier frontal bone.
Contraindications
Contraindications to surgical repair of a frontal sinus fracture include patient inability to undergo general anesthesia secondary to intracranial injuries, decreased mental status, hemodynamic instability, and pending treatment of other, more potentially life-threatening injuries. Often, many of these contraindications are present in patients with trauma to the frontal sinuses. Definitive surgical treatment of frontal sinus fractures is often delayed for these reasons.
-
CT scan showing frontal sinus fracture with comminution injury to the anterior table and supraorbital rim. However, the posterior table appears to be intact.
-
More superior cut of CT scan showing frontal sinus fracture with comminution injury to the anterior table and supraorbital rim. The degree of anterior table displacement was sufficient to cause significant aesthetic deformity. Although the fracture spares the base of the frontal sinus and the posterior wall, the sinuses were explored for nasofrontal duct injury. The ducts were found to be intact. The anterior table was repaired, and no obliteration was performed.
-
Fracture of the frontal sinus involving the anterior table and both supraorbital rims, medial to the supraorbital notch.
-
Lower cut of CT scan in a patient with fracture of the frontal sinus involving the anterior table and both supraorbital rims, medial to the supraorbital notch. Note the fracture extension through the base of the frontal sinus and involvement of the anterior ethmoid complex. Even though the fracture spares the posterior table, damage to the nasofrontal ducts is highly likely.
-
Coronal views of a CT scan in a patient with fracture of the frontal sinus involving the anterior table and both supraorbital rims, medial to the supraorbital notch. Note the injuries to the frontal recesses. Injury to the nasofrontal ducts is expected.
-
More anterior view of a coronal CT scan in a patient with fracture of the frontal sinus involving the anterior table and both supraorbital rims, medial to the supraorbital notch. Note associated orbital blowout fracture.
-
A proposed algorithm for the management of anterior table fractures. Note that in the case of a displaced anterior table fracture with involvement of the nasolacrimal duct, some have also proposed recannulation of the duct.
-
A proposed algorithm for the management of frontal sinus posterior table fractures. In patients with cerebrospinal fluid leak and displacement, obliteration or cranialization is usually indicated. If no cerebrospinal fluid leak is present, the fracture can be reduced and the algorithm for anterior table fractures can be followed. See Image 7.










