Overview
Despite increased attention to the nasal component of primary cleft lip reconstruction, repair of secondary cleft lip and/or nasal deformities remains challenging and often frustrating. The literature describes many techniques; their success is inversely proportional to the severity of the deformity. For information on various cleft lip and cleft nasal reconstruction, see the Craniofacial section of eMedicine’s Plastic Surgery journal. [1]
Regardless of the method used, a reconstructive surgeon's treatment plan should aim at the closest approximation to normal appearance using the least number of surgical stages with the fewest possible donor site deformities. Surgeons always should consider the normal ethnic variables in nasal form. For example, in Asian patients, achieving nasal tip projection is less important than in Caucasian patients. In black patients, a horizontally oriented nostril is more acceptable as normal. In unilateral deformities, the goal should be symmetry relative to the normal side. In bilateral deformities, the aim should be for more tip projection and dorsal height. [2]
In the author's opinion, achieving an approximately normal appearance in significantly deformed noses is virtually impossible without adding extra structural materials or moving skeletal segments. Weakening the nasal skeletal framework with cartilage reductive maneuvers is not helpful with this surgery. The sources of these materials, as well as their relative advantages and disadvantages, are discussed in this article.
Timing of Surgery
The nose undergoes a rapid, although late, growth spurt during puberty and early adolescence. A child's "cute" button nose suddenly begins to take on an adult form when the child is aged 11-14 years. Girls usually achieve physical maturity much earlier than boys. Rapid change occurs in size, shape, and skin thickness. Suddenly, the familial genes that have been lying dormant assert themselves and not always with a welcome result.
Nasal deformities are due not so much to the growth of the nasal bones as to the sudden upsurge of the nasal process of the maxilla, which is the route through which the osteotomy chisel must pass during reconstructive rhinoplasty. The growth center in the lower portion of the septal cartilage should be spared during the early years of development.
During this period of life, a young person undergoes radical emotional and hormonal changes. Although emotional maturity has no linear relationship to age, the key to success in any nasal surgery is not physical but emotional maturity of the patient. Psychological stability is mandatory for successful surgery. Therefore, postponing these operations until the nose has achieved its full growth is preferable; this generally is in girls aged 13-15 years and in boys aged 14-16 years.
Nonetheless, caring surgeons often are caught in a dilemma. In some children, postcleft deformities are associated with a heavy emotional burden. Developing normally at an age when peer approval is so needed is not easy for a stigmatized child. Thus, a fine balance of judgment is required in deciding whether to postpone the surgery and risk permanent psychic scars or to operate early and possibly compromise eventual results.
Pathologic Anatomy
The typical unilateral deformity usually consists of 10 identifiable components that may exist in varying degrees, as follows:
Nose deviates to affected side.
Affected dome is lower.
Lateral crus is crimped or distorted.
Edge of cartilage and nostril is tipped caudally.
Tendency toward bifidity is present.
Columellar nostril angle is obtuse.
Bony floor is depressed or missing.
Nostril angle is acute, and nostril axis is horizontal.
Nostril sill is missing.
Septum is shifted toward normal side.
In bilateral deformities (although the septum may not be deflected), 3 additional problems are encountered: (1) the columella is very short; (2) a marked lack of nasal tip projection is present due to displaced or inadequate alar cartilage, and (3) both nostril axes are oriented much more horizontally than vertically.
Underlying fundamental deformities of the maxillary framework often must be addressed. Although these deformities are beyond the scope of this article, dramatic improvements can be achieved with recently developed craniofacial surgery techniques. To achieve radical improvements, one must resort to radical surgery.
Consider the following simple analogy. If an A-frame cabin was constructed on uneven ground and an earthquake split the underlying ground and dropped it away under one wall, the whole house would sag on that side. The main weight-bearing wall (the septum) dividing the house also would twist badly. Obviously, the house cannot be rebuilt properly until the sagging support is corrected. This may require mobilization of maxillary segments or bone grafting.
Types of Repair
Unit rotation using external incisions
With unit rotation using external incisions, the deformed nostril is approached through external skin incisions extending onto the dorsal skin of the nostril, and the deformed portion is rotated cephalad as a unit of skin cartilage and sometimes mucosa. The principal advocates of this approach do not consider the external scar a drawback and demonstrate good results with well-healed, acceptable, but nonetheless visible scars on the columella and the dorsal skin of the nasal tip. If any way exists to achieve the stated goals without an external scar, no matter how unobtrusive, the author prefers to do so, even if this approach is technically more difficult.
Anatomic rearrangements using internal incisions
During anatomic rearrangements using internal incisions, various intranasal or nostril margin incisions are used to expose the abnormal cartilage, which then is rearranged into quasi-normal relationships. They are held in position to the upper lateral cartilage directly above, the contralateral upper lateral cartilage, or the normal opposite alar dome with a variety of fixation techniques. McIndoe, Erich, Potter, Stenstrom and Oberg, Rees and colleagues, Spira, Cosman and Crikelair, Reynolds and Horton, and others have demonstrated good results. [3, 4, 5, 6, 7, 8] These procedures avoid an external scar, and the early results are pleasing. However, most such procedures depend on suture fixation alone. With the passage of time, these types of repairs always tend to show significant loss of improvement.
Anatomic rearrangements using internal incisions with additional structural support
During anatomic rearrangements using internal incisions with additional structural support, a combination of incisions is used to reposition or equalize the existing cartilage of the nasal tip. In addition, the repair is reinforced with other autogenous structural supports or onlays. Typical of these techniques are those of Millard, Gorney and Falces, Musgrave, Cosman and Crikelair, Nishimura and Ogino, and Dibbell. [9, 10, 7, 11, 12, 13]
Some authors have shown gratifying results using alloplastic materials. However, in the author's experience, alloplastic materials, regardless of how well fabricated or innocuous, eventually cause more problems than they solve; many eventually extrude.
State-of-the-Art Techniques
If the deformity is minimal, modified tip rhinoplasty techniques with reduction of the normal side and mobilization of the abnormal side to a more superior medial position may be sufficient. When the structural elements of the tip of the nose are largely present but are malpositioned, they can be rearranged using inconspicuous incisions inside the rim of the nostrils. If external support is to be added, an open rhinoplasty approach can be performed, which involves lifting the skin of the columella to expose the entire tip anatomy. This technique leaves a barely visible scar, usually an inverted V that connects to bilateral marginal incisions, at the base of the columella.
If external scars are to be avoided and the deformity involves some underdevelopment of the maxillary support on the cleft side, surgical repair must be designed around the addition of adequate structural support for the nasal tip. This support preferably should be autogenous cartilage or bone. If the maxillary support is mildly deficient, an onlay bone graft may suffice. If the support is significantly deficient, consider maxillary advancement (at a previous stage) with or without a bone graft.
Unilateral Deformities
Graft materials
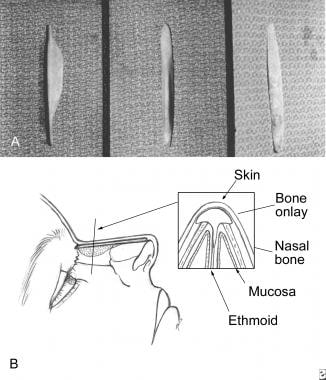
If the surgical plan calls for structural materials, obtain these first. The sources of such material are shown in the image below. When possible, the author's preferred donor source is the nose; however, the septum is often twisted, inadequate, or insufficient. In that situation, split calvarium is preferred for bone, and the ear is preferred for cartilage (the ear has amazing potential as a donor site with minimal secondary deformity). The author prefers to fabricate the graft differently.
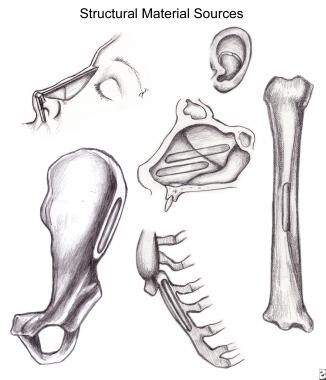 Sources of structural support material (in order of preference): A, septum; B, ear cartilage; C, rib cartilage; D, tibial crest; E, pelvic rim crest.
Sources of structural support material (in order of preference): A, septum; B, ear cartilage; C, rib cartilage; D, tibial crest; E, pelvic rim crest.
Incisional approach
The structural anatomy of the nasal tip is easily accessible through an open rhinoplasty approach. Marginal incisions are connected across the columella in an inverted V. The excellent circulation in the area makes this approach extremely safe, even if the rest of the rhinoplasty procedure is performed through it (see the image below).
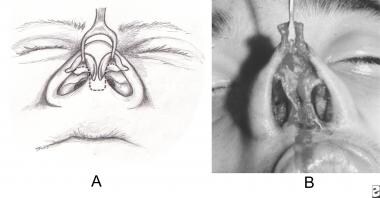 A. Nostril and columellar rim incision for complete tip cartilage exposure. B. Surgeon's view after dissection and elevation.
A. Nostril and columellar rim incision for complete tip cartilage exposure. B. Surgeon's view after dissection and elevation.
Addressing asymmetry
Significant asymmetry can be addressed accurately. [14] In unilateral deformities, the normal alar cartilage has a lateral crus significantly wider than the opposite side. [15] To correct this asymmetry, the relative excess on the normal side is resected and saved for later use. Having achieved dimensional parity, the degree of positional disparity on the left side can be assessed and corrected in one of several ways. If the end of the lateral crus curls into the nostril and the genu is displaced inferiorly, it may have to be dissected, scored, and reattached in a more normal attitude to the next higher stable point. This point may be the dome of the opposite normal side or, more likely, the lowest point of the opposite normal upper lateral cartilage. Either way, such repositioning is more likely to achieve dramatic improvement and permanent results if a stabilizing cartilage strut is installed between the medial crura.
This strut must sit on the maxillary spine and must be thin enough to avoid making the columella too wide, yet strong enough to act as a support. Stability can be achieved by making it wide enough in the dorsal-ventral dimension. However, if this strut is allowed to protrude above the level of both alar domes, it will project under the skin as an abnormal white bump. Even if both domes are moved well above the tip of the strut and are fixed through both domes and the strut, the protrusion may become visible over time. Also, often insufficient material is present with which to build enough definition to achieve a normal appearance of the nasal tip.
The problems of strut camouflage and tip projection can be corrected by creating a cartilage tip graft. Preferably, it should be made of septal cartilages. If this material is not available, the concha caval ear cartilage is best. The tip graft must be sutured in position accurately, which is accomplished most easily when the whole tip assembly is exposed with an open rhinoplasty approach (see the image below).
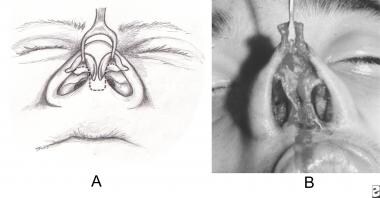 A. Nostril and columellar rim incision for complete tip cartilage exposure. B. Surgeon's view after dissection and elevation.
A. Nostril and columellar rim incision for complete tip cartilage exposure. B. Surgeon's view after dissection and elevation.
Nostril floor, sill, and nasal pyramid
The nostril floor must match the width and altitude of the opposite side. If sufficient soft-tissue coverage is available, use an onlay bone graft. If the deficiency is profound, consider maxillary reconstruction.
Once the tip of the nose has been balanced, the problem of the nasal pyramid must be addressed. If adequate structural integrity exists, perform standard osteoplastic rhinoplasty with midline and lateral osteotomies. If the nasal pyramid appears inadequate after the tip deficiency is corrected, a dorsal graft of sandwiched septal cartilages or a calvarial bone graft often must be used.
Bone Grafts
If a bone graft is to be used to build up an inadequate profile, bridge a supratip depression, or camouflage a crooked nose, it can come from the pelvis, ulna, tibia, or cranium. The author has found that calvarial bone provides the straightest and most reliable bone.
Once harvested, the graft must be fashioned and installed to be stable. Although all bone grafts undergo some reabsorption over time, bone-to-bone contact promotes direct healing, stability, and durability. To maximize such contact, the author fashions grafts with a keel on the undersurface (see the image below). This keel fits directly in the midline osteotomy, thus giving the desired contact, stability, and profile elevation. Countersinking the graft to the superior aspect of the nasal bones with a titanium screw further maximizes contact. Naturally, the graft must be fitted so that its caudal end sits higher than the reconstructed tip.
Bilateral Deformities
The approach to bilateral stigmata also must vary according to the degree of existing deformity, but more difficult problems may exist, as follow:
A short, tight columella
Flaring, horizontally directed nostrils
Completely inadequate nostril floors
Unstable central maxillary segment (premaxilla)
Two vertical scars on upper lip, which may be insubstantial, too tight, or too long
If the nostril orientation is relatively normal, the author's general approach is as described. When faced with problems 1 and 2, a different solution is preferred.
The problem of a short columella has been discussed extensively in the literature. The author believes that if the columella is to be lengthened, the extra tissue must come from the skin of the upper lip. The extra tissue must be in direct proximate continuity with the columella. In boys, particularly if a Millard's forked flap is to be used, advancing hair-bearing skin onto the nose must be avoided. In all cases the forked flap leaves a very unnatural nasolabial angle.
If the lip is extremely tight, an Abbe flap transfer into the center of the lip recreates the philtrum and frees the tethered nasal tip to allow lip tissue to be used as additional columella.
In severe cases in which the columella is too short, the tip is tethered tightly, and the nostril axis is horizontal, the author prefers the approach described by Gorney and Rosenberg in 1979. [16]
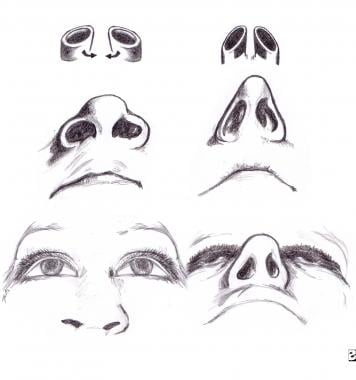
Concept of treatment
The basic concept of this procedure is explained by analogy: The nostril deformity in the double cleft is similar to 2 pipes, elliptical in cross-section, lying on their sides half buried in the ground. The objectives are to lift these pipes out of the ground and then rotate them centripetally 90° so that the central axis of the elliptical pipe is turned from a generally horizontal or oblique plane to a more nearly vertical one. Once this rotation is accomplished, the pipes must be held up in the desired position by a vertical support between them (see the image below).
History of technique
The addition of tissue to the columella from the nasal floor has proved to be a satisfactory technique for lengthening the columella without disturbing lip tissue. Cronin described this technique in 1958 but noted that others had suggested such an operation. [17] In describing his banked, forked flap, Millard noted that this secondary procedure is reminiscent of Cronin's technique but with more tissue available.
The use of cartilage grafts for nasal support dates back to Von Mangoldt in 1899. In discussing the bilateral cleft lip nose, Brown and McDowell recommended an L-shaped preserved or autogenous cartilage graft for patients with a deficient columella and poor septal support. [18] Marcks and colleagues elongated the columella using flap transfer and Z-plasty. [19] Cronin also suggested a cartilage post, particularly when the soft tissues of the newly lengthened columella do not support the tip. [17] Meade used auricular cartilage struts in conjunction with a composite auricular graft to augment the columella. [20]
Musgrave also recommended additional nasal tip cartilage support as a second stage following composite grafting, whereas Gorney and Falces devised a gull-wing autogenous auricular graft to provide columellar and alar support. [10, 9] Dibbell showed startling results with his "Bowie knife" columellar posts. Finally, Millard emphasized the advantages of autogenous septal cartilage for use in the columella, including strength, lack of bulk, and availability. Peer observed that septal cartilage grafts transplanted in human tissue maintain their structure. [21]
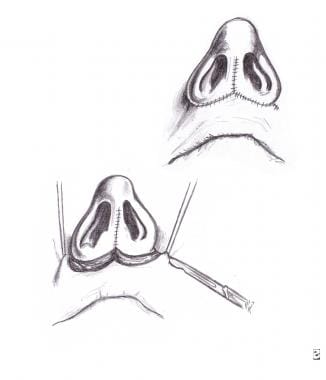
Technique
The surgery can be performed under either local or general anesthesia. The author prefers general anesthesia in younger patients and local anesthesia in more mature and stable ones. The incision design basically follows Cronin's pattern but with lateral extension of the incision around the base of the nostril and well up into the alar crease (see the image below).
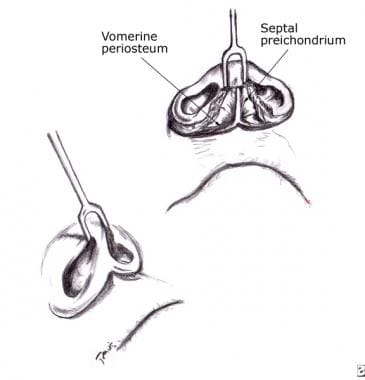 A. Degloving of soft tissues of nasal tip including septal perichondrium. B. Elevation of dissected tip soft tissue by upward traction.
A. Degloving of soft tissues of nasal tip including septal perichondrium. B. Elevation of dissected tip soft tissue by upward traction.
As the dissection of the nostril bases proceeds in depth, exert maximum traction on the tip of the nose with a dull, double-pronged hook. After making the initial skin and subcutaneous incision, proceed with the dissection obliquely downward to include the nostril bases and as much of the floor of the nose as possible. This technique may be difficult in the double cleft. The natural tendency is to perforate the nasal cavity at the floor of the nose. Make every attempt to have the perforation occur as far back in the nasal cavity as possible. Unlike the classic Cronin procedure, the cutaneous columella is not separated from the septal mucosa immediately contiguous to it.
As the dissection proceeds medially toward the septum, insert a small, sharp, submucous elevator under the periosteum of the vomer and the perichondrium of the cartilaginous septum, and continue elevation in the plane as far back as normally performed during standard septoplasty. It also should continue superiorly all the way to the skin of the dorsum of the nose, if possible.
After this maneuver is completed (with continuing traction of the tip of the nose), deglove the soft tissue of the entire tip, including the alar cartilages and septal mucosa, from the cartilaginous septum as a unit (see the image above). At this point, the clearest possible view of the quadrilateral septal cartilages and vomer is available. As much cartilaginous material as necessary can be obtained from the septum for both the tip strut and the dorsum if required. Remove as much septal material as is compatible with remaining adequate dorsal support. Leaving sufficient dorsal support to prevent subsequent collapse is extremely important, as in all septal surgery.
If sufficient supportive material is not available, the next best source is the medial (cartilaginous) portion of the rib, which needs to be harvested. The best source of cartilage for nasal surgery that has no structural support function is the conchal cartilage of the ear. Virtually the entire conchal cartilage can be removed with little visible deformity except a setback of the ear position on the head. For structural support purposes, if septum or rib is not available, the outer table of the cranium in the parietal area or pelvic crest suffices. The material obtained from the septum now must be divided into several segments, depending on the amounts needed.
If no osteoplastic rhinoplasty is contemplated, a much greater illusion of narrowing can be obtained by adding dorsal height. This technique also creates a "light line" along the nose that greatly enhances appearance. This height is achieved by trimming and tailoring a section of the material obtained for insertion under the dorsal skin of the nose, either as a single spear or as a sandwich graft consisting of several stacked thin layers of cartilage tailored to fit and sutured together. Wrapping it in fascia helps to soften the edges. This also builds dorsal height.
The best and strongest segment of the septal material must be used as a strut between the medial crura of the liberated alar cartilages. The bottom of this strut should fit into the nasal spine by either a notch or mortise-and-tenon arrangement. Any suitable suturing material can be used to fix the medial crura of the ala to the cartilage strut. The base of the supporting strut may be fixed to the spine if desired. Any remaining material now can be used as a separate subcutaneous tip graft to give the blunted tip more definition and projection and to improve the profile.
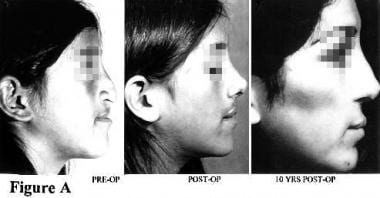
The centripetal rotation of the nostrils designed to change their axis and configuration leaves a significant defect at the donor site. To avoid creating any distorting pulls on the newly repaired area, close this defect using direct undermining and approximation superiorly and laterally; therefore, the resulting scars lie along the natural nasolabial creases (see the first image below). In many patients, the lip is too long, and not enough vermilion shows. A secondary advantage of this maneuver is that it lifts and shortens the lip repair. Closure of the defect tends to significantly improve this condition. Results that can be achieved with these techniques are illustrated in the second, third and fourth images below)
The author feels that repairing the lip alone or the nose alone is short sighted. Once the patient has achieved adequate adult proportions, the surgeon is obligated to consider the whole central face and be prepared to correct any deformity, whether bony or soft tissue. The ultimate objectives should be restoration to physical normality and more importantly, restoration of a positive body image that allows the stigmatized patient to function better in society.
-
Sources of structural support material (in order of preference): A, septum; B, ear cartilage; C, rib cartilage; D, tibial crest; E, pelvic rim crest.
-
A. Nostril and columellar rim incision for complete tip cartilage exposure. B. Surgeon's view after dissection and elevation.
-
A. Three views of carved dorsal "keel" implant: (1) lateral, (2) ventral, and (3) dorsal. B. Diagrammatic placement of implant. "Keel" must fit firmly into the dorsal edge or between separated nasal bones.
-
Centripetal rotation of nostril axes and fixation to vertical post.
-
A. Degloving of soft tissues of nasal tip including septal perichondrium. B. Elevation of dissected tip soft tissue by upward traction.
-
Centripetal rotation and fixation across septal post with sutures or soft tissues.
-
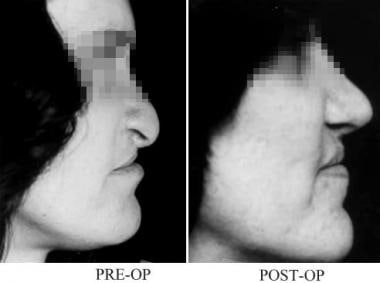
Preoperative view; immediate postoperative view.
-
Preoperative and 5-year postoperative views of surgical repair of cleft nasal deformity.
-
Preoperative and 5-year postoperative views of surgical repair of cleft nasal deformity.
-
Preoperative and 7-year postoperative views of surgical repair of cleft nasal deformity.