Background
The brow lift operation aims to correct the loss of soft tissue elasticity in the upper third of the face, which may lead to ptosis of the brow and hypertonicity of the frontalis, corrugator supercilii, and procerus muscles with subsequent wrinkling of the forehead (see the image below). This confers a look often described as tired. Several techniques are available to correct this occurrence depending on the individual patient's needs and desires. [1, 2]
The operative nomenclature describes the incision employed or the level of undermining necessary to achieve the result. Of course, it makes more sense to describe the operation using terms to define both the incision used and the level of undermining employed (eg, pretrichial subgaleal brow lift).
Pretrichial denotes an incision in front of the hairline. On a practical note, it is advisable to make the bevelled incision about 2 mm behind the hairline to induce hair growth through the scar and improve cosmesis. See the image below.
 Diagram showing preoperative marking: The scalpel incision follows 2 mm behind the hairline in the frontal region and extends into the hair in the temporal region. The lateral extension joins the upper extent of the facelift incision, if a facelift is performed at the same time. The incision is beveled posteroanteriorly.
Diagram showing preoperative marking: The scalpel incision follows 2 mm behind the hairline in the frontal region and extends into the hair in the temporal region. The lateral extension joins the upper extent of the facelift incision, if a facelift is performed at the same time. The incision is beveled posteroanteriorly.
According to statistics from the American Society of Plastic Surgeons, its members performed 13,318 brow lifts in 2022, a 17% reduction from the 16,046 such procedures performed in 2019, prior to the coronavirus disease 2019 (COVID-19) pandemic. Of the 2022 figure, 93% of the surgeries were performed in females. [3]
For expert viewpoints on skin procedures, see Medscape’s Aesthetic Medicine Resource Center.
Problem
Aesthetically, the face is divisible into 3 equal parts, of which the forehead (from the top of the eyebrow to the anterior hairline) occupies the upper third. In males, this area averages 7 cm; in females, it averages 5 cm. In Caucasians, in the ideal situation, the medial extent of the eyebrow lies over a line extrapolated upward from the nasal ala to the medial canthus. The lateral extent of the eyebrow lies over a similar line extrapolated upward from the nasal ala to the lateral canthus. The male eyebrow is less arched than the female eyebrow. Maximum arching of the eyebrow occurs in a vertical line with the lateral limbus. The male eyebrow lies at the level of the supraorbital rim; the female eyebrow lies above the rim. The top of the eyebrow lies approximately 2.5 cm from the mid pupil. [4] A lesser distance denotes eyebrow ptosis. With aging, these parameters may shift.
Pathophysiology
Loss of forehead skin elasticity from genetics, solar damage, and gravity causes eyebrow drooping, with resultant upper eyelid ptosis and visual embarrassment. This causes hypertonicity of the forehead elevator muscles. Aging causes depletion of the subcutaneous fat with resorption of the subjacent skull bone. This leads to forehead wrinkling, the direction of which depends upon the vector of action of the underlying muscle.
Presentation
Clinical presentation
The patient may state that others describe him or her as having a tired, surprised, worried, or annoyed look. Younger patients may state that they are misconstrued as aged.
Clinical examination
The position of the hairline, eyebrow, and upper eyelids is carefully noted. The role of brow ptosis in causing pseudoblepharoptosis or in adding to blepharochalasis is examined. The examination is performed by manually locating the eyebrow to the ideal position and observing the effect on the upper eyelid. The presence of lagophthalmos is a contraindication to surgery. The sites of forehead wrinkles are recorded along with eyebrow asymmetry, which should be brought to the patient's attention. The patient is counseled on realistic results. If the patient questions the postoperative results, preoperative photodocumentation, apart from self-education, can help the physician demonstrate the results to the patient.
Indications
The pretrichial incision is indicated in individuals with a forehead section that is aesthetically larger than acceptable. Allowances must be made for impending or foreseeable receding male hairlines, which often require another approach.
Relevant Anatomy
Forehead region
The layers in the forehead and scalp region include the skin, subcutaneous fat layer, superficial musculoaponeurotic system (SMAS) equivalent termed the galea (which incorporates the paired frontalis muscles and continues laterally to become the temporoparietal fascia), a loose areolar layer, and the periosteum.
The frontalis muscle inserts at the medial supraorbital rim into the upper part of the orbicularis oculi muscle and overlying skin. The paired corrugator muscles, arising from the periosteum at the superomedial aspect of the orbital rim, lie deeper and insert with the frontalis and orbicularis oculi into the skin laterally. The supratrochlear nerves may penetrate the corrugator muscle to emerge on the deep surface of the frontalis muscle. Damage to the nerve may occur at this point during corrugator resection. The procerus muscle lies medial and ventral to the corrugator muscles, arising from the nasal bones and upper lateral cartilages and inserting into the skin between the eyebrows. The supraorbital nerve and vessels usually emerge from the supraorbital notch or canal and continue cephalad in the galea. Occasionally this neurovascular bundle may exit from a foramen cephalad to the orbital rim, demanding caution with blind subperiosteal dissection within 2 cm of the supraorbital rim.
Temporal region
The layers of the temporal region include the skin, subcutaneous fat, temporoparietal fascia (the equivalent of the SMAS layer), temporal fascia, and the temporalis muscle. See the image below.
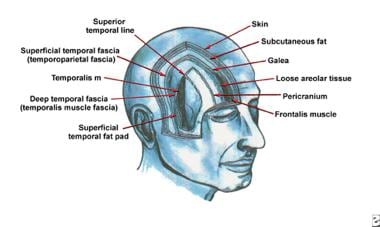 The fascial planes of the forehead and temple. The temporal branch of the facial nerve runs within the superficial temporal fascia (ie, temporoparietal fascia).
The fascial planes of the forehead and temple. The temporal branch of the facial nerve runs within the superficial temporal fascia (ie, temporoparietal fascia).
The temporal fascia overlying the muscle splits into 2 layers that enclose the superficial fat pad before reuniting approximately 1 cm above the superior margin of the zygomatic arch and fusing with the parotidomasseteric fascia below. The deep fat pad is an extension of the masticatory fat pad of Bichat and lies deep to the deeper layer of temporal fascia. The frontal division of the temporal branches of the facial nerve lies in the temporoparietal fascia and is at risk during lateral undermining.
For more information about the relevant anatomy, see Forehead Anatomy.
Contraindications
Contraindications to surgery include general systemic instability and bleeding dyscrasias. The patient must discontinue use of aspirin and similar medications at least 2 weeks prior to surgery and for 2 weeks postoperatively. An absolute contraindication is the presence of lagophthalmos. Psychosocial deficiency is carefully assessed. Unrealistic expectations must be dealt with preoperatively.
-
Schematic sagittal section through forehead in the frontal region.
-
Schematic dissection in the loose areolar tissue (subgaleal) plane in the frontal region. View from cephalic aspect.
-
The supratrochlear nerve branches penetrating through the corrugator muscle are shown. The orbicularis oculi muscle has been reflected downward, and the periosteum has been incised superiorly.
-
The superficial temporal artery and its subdivisions above the level of the zygoma lie in the superficial musculoaponeurotic system layer.
-
Schematic representation of the frontal division of the temporal branches of the facial nerve around the zygoma region. The deep layer of the temporal fascia separates the superficial fat pad from the deep fat pad.
-
Diagram showing preoperative marking: The scalpel incision follows 2 mm behind the hairline in the frontal region and extends into the hair in the temporal region. The lateral extension joins the upper extent of the facelift incision, if a facelift is performed at the same time. The incision is beveled posteroanteriorly.
-
Preoperative view of forehead of an ideal patient.
-
Postoperative view of same patient following pretrichial brow lift.
-
The fascial planes of the forehead and temple. The temporal branch of the facial nerve runs within the superficial temporal fascia (ie, temporoparietal fascia).