Background
Technology has created a trend for less invasive procedures in all surgical specialties. The endoscope, with its accompanying instrumentation, has been the key development supporting this trend. It has helped surgeons in nearly every surgical specialty, including plastic surgery, develop less invasive techniques. With new technology comes patient demand and expectation for less invasive procedures, or at least for procedures perceived as such. The endoscope now is used in a variety of reconstructive and cosmetic plastic surgical applications, with the endoscopic brow lift the first procedure to gain widespread acceptance. [1, 2]
History of the Procedure
Over the last four decades, more surgical specialties have incorporated fiberoptic and endoscopic technology. Endoscopes have been widely used by gynecologists since the 1970s for diagnostic and therapeutic procedures. By the end of that decade, the same technology was gaining acceptance in the orthopedic specialties for diagnostic procedures. As instrumentation improved, less invasive therapeutic procedures became widely accepted..
Endoscopic procedures were introduced into general surgery in 1986, and laparoscopic (endoscopic) cholecystectomies became standard by 1990, with increasingly complex surgeries gradually transitioning to less invasive approaches. In the early 1990s, the first endoscopic brow lift procedures were described. [3] Shortly thereafter the endoscope was incorporated into plastic surgery of the mid and lower face, breast, abdomen, hand (in carpal tunnel surgery), and trunk. [4, 5]
The advent of the endoscopic approach to the face and, in particular, the brow was brought about in large part by the ability to create a sufficient optical cavity. Specialized dissection instruments and understanding of principles of brow suspension were also significant contributing factors.
Problem
A treating plastic surgeon should examine the face as a whole to better determine which procedures will help achieve the goal of a balanced natural appearance. [6] When evaluating the face for rejuvenation or other cosmetic improvement, surgeons classically divided the face into 3 sections: face and/or neck, brow, and eyes. As techniques and technology advanced, analysis of the face became more sophisticated, changing relationships between these classifications. The face and neck now are analyzed as mid face, lower face, and neck. For information and CME activities on aesthetic procedures of the face, visit Medscape’s Aesthetic Medicine Resource Center.
Evaluation of the eyelids now includes examination of the midface. Brow examination must include evaluation of lids and the general orbital area. Specifically, patients with upper lid ptosis or even blepharochalasia must be evaluated regarding dynamic rhytides of the forehead. Patients with lid ptosis often overanimate brow elevation to help open their eyes. It is critical to carefully evaluate brow and lid ptosis, because often these patients require surgical correction of the eyelids in conjunction with the brow lift. The location of the hairline or width of the brow must be noted also. [7] Very high foreheads or very deep rhytides may require some degree of skin excision in addition to endoscopy to allow relaxation of the forehead.
Although most facial soft tissue structures tend to descend under constant forces of gravity and time (eg, cheeks, neck), the brow is often an exception. Some individuals naturally have a low-set brow. Others may show significant signs of facial aging but have little or no brow ptosis. Just because a brow can be elevated does not mean it should be elevated.
The endoscopic brow lift can be performed for the following reasons:
-
Elevate the eyebrows - Brows may be congenitally low or low from changes associated with aging; elevating the brow may remove excess skin and/or fullness from the upper eyelid
-
Improve symmetry of the eyebrows
-
Change the shape of the eyebrows
-
Decrease the transverse static wrinkles of the brow
-
Decrease function of muscles in the brow and glabellar region that cause dynamic wrinkling
Pathophysiology
Poor brow position can be an inherited condition or an acquired condition associated with aging. As with other soft tissue structures of the face, the brow may become ptotic with increasing age; however, note that in the youthful face the brow is often quite low yet still attractive. As the face ages, fat is lost from the orbital rim between the brow and eyelid, creating an aged or ptotic appearance.
Repetitive or hyperactive use of corrugator muscles can depress the medial head of the eyebrow over time. [8, 9] Similarly, overuse of frontalis muscles, especially on one side, can create noticeable asymmetry in eyebrow height. In addition, patients who have significant upper lid ptosis may attempt to compensate by overusing the frontalis muscle to lift the brows and, subsequently, the lids out of the field of vision.
Presentation
Good candidates for endoscopic brow lift present in several ways. The patient may note that the brow is ptotic or low. These patients commonly report that their eyes have a tired or heavy appearance. Often they note that they "have always had this" or that it "runs in the family." Frequently, the patient has practiced achieving the desired look by pulling the lateral brow up with his or her hands while looking in the mirror.
Patients often present with excess upper eyelid skin. Carefully evaluate the brow in any patient evaluated for cosmetic eyelid surgery, because the brow may be involved in 50% of patients.
Patients frequently present with a chief complaint of deep glabellar rhytides caused by excessive corrugator activity. They often are frustrated that they look angry, upset, or tired when they do not feel this way. They have a frequent subconscious tendency to frown. Additionally, patients may be concerned with horizontal forehead creases caused by excessive frontalis activity.
Patients may also present for endoscopic brow lift after being treated with neuromodulators for some period of time. These are individuals seeking a permanent solution to avoid repeated injections to maintain their brow appearance.
Indications
In the normal brow (see the image below), the medial eyebrow extends to the medial canthus of the eye, and the lateral eyebrow extends to the intersection of an imaginary line drawn from the nasal ala through the lateral canthus of the eye. [10] Head of the medial eyebrow can begin below or at the medial orbital rim. Tail of the lateral brow is positioned above the bony orbital rim, often dropping to the same horizontal level as the medial head of the eyebrow. Tail of the brow normally may be found above the horizontal line of the medial brow. Apex of the brow arch lies immediately above the lateral edge of the iris. In fashion models, the apex tends to be at the point dividing the medial and lateral third of the brow, or sometimes even more laterally, creating a stylized or more exotic appearance. In the average patient the apex of the brow often is located more centrally, but this still can produce an attractive brow.
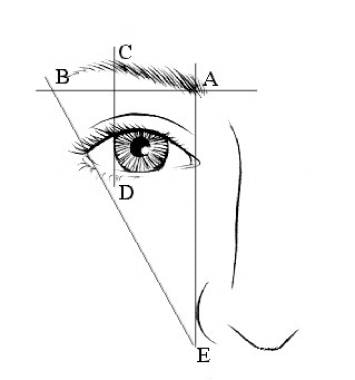 An aesthetic brow. A-B Lateral brow is at or above medial brow. C-D Brow peak is at lateral limbus of the iris or at junction of medial and lateral thirds of brow. A-E Head of medial brow begins at vertical line extending from nasal ala. B-E Lateral brow may extend to a line drawn from ala through lateral canthus of eye (Gunter JP, Antrobus SD: Plast Reconstr Surg 1997; 99(7): 1808).
An aesthetic brow. A-B Lateral brow is at or above medial brow. C-D Brow peak is at lateral limbus of the iris or at junction of medial and lateral thirds of brow. A-E Head of medial brow begins at vertical line extending from nasal ala. B-E Lateral brow may extend to a line drawn from ala through lateral canthus of eye (Gunter JP, Antrobus SD: Plast Reconstr Surg 1997; 99(7): 1808).
Recent analysis has provided objective evidence that the ideal youthful brow peak has migrated laterally over recent decades to lie at the lateral canthus. [11] In addition, there has been a nonstatistically significant trend toward lower and flatter brows.
In evaluating the orbit, note several essential things, including depth of the orbit or eye socket and shape of the overall orbit. In a patient with deep-set eyes, an overly elevated brow appears more abnormal, whereas a patient with a shallower orbit can tolerate over-elevation of the brow and still appear within normal limits.
As the face ages, the orbital shape changes from an oval or egg shape to a circular shape, caused most often by ptosis of the mid face. In patients with significant nasojugal crease from midface ptosis, avoid elevating the brow as an isolated procedure, since this accentuates the circular shape of the orbit and increases the aged appearance. Consider performing a facelift or mid facelift in conjunction with brow lift. A mid facelift also can be performed in conjunction with a lower eyelid procedure.
Check for asymmetry, which often goes unnoticed by the patient. Noticeable asymmetry of eyebrows is present in approximately one third of patients. Often the distance from orbit to brow is the same bilaterally even though the brows appear uneven. In this situation, the entire orbit on one side of the face is usually lower. Decide which approach provides a more symmetric look—raising the brow the same degree bilaterally, which maintains the asymmetry of the brow, or raising the eyebrows asymmetrically, which equalizes the eyebrows but may introduce a new asymmetry in distances between brows and eyes. Computer imaging helps determine the more suitable approach.
Although any brow can be elevated, evaluate the amount of redundant skin in the lateral canthal region. [12] Significant overhanging skin near the "crow's feet" is difficult, if not impossible, to remove with eyelid surgery alone. Elevating the lateral brow may be necessary. This is one helpful indication in addressing the need for brow elevation, especially in the patient presenting with heavy upper eyelids.
Relevant Anatomy
Scalp
Scalp layers include skin, subcutaneous tissue and fat, the galeal aponeurosis, and periosteum. As the scalp joins the forehead, an additional layer of muscle (frontalis muscle) is found between the subcutaneous and galeal layers. The superficial fascia is a fibrofatty layer that connects skin to the underlying aponeurosis of the occipitofrontalis muscle and provides a passageway for nerves and blood vessels. See Scalp Anatomy for more information.
Vascular anatomy
Supraorbital vessels exiting supraorbital foramina above each orbit supply the forehead. These vessels coalesce with superficial temporal arteries and occipital vessels in the posterior scalp to provide a redundant blood supply to the scalp. The entire scalp can survive on one major arterial vessel. Additional blood to the central forehead is supplied by supratrochlear vessels exiting the orbits superomedially and extending in a cephalad direction. In the temporal region, the sentinal vein should be avoided. [13]
Neurologic anatomy
Sensory nerves to the forehead (supraorbital and supratrochlear nerves) exit the orbits in neurovascular bundles with supraorbital arteries and supratrochlear arteries. These nerves may be large singular nerves or smaller bundles. Usually a dominant single nerve is present. Supraorbital nerves exit approximately 2.7 cm from the mid line. Nerves easily are seen and preserved. [14]
Motor nerves
The facial nerve's temporal branch (VII) provides innervation to the frontalis muscle. Its course follows a line drawn from the tragus through a point 1-1.5 cm lateral to the eyebrow's lateral tail. The nerve is found in a fatty layer between the temporoparietal fascia and superficial layer of the deep temporal fascia (see the first image below). During dissection, one can identify the general location of this motor nerve by locating a predictable vein (see the second image below), referred to as the "sentinel vein." Injury to this nerve can cause temporary or permanent frontalis muscle paralysis. See Facial Nerve Anatomy for more information.
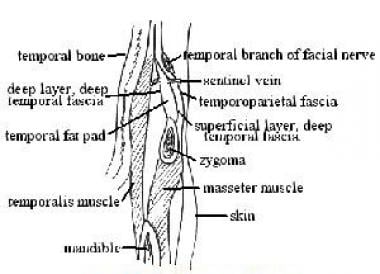 Cross section illustrating anatomy of temporal region and close relationship between sentinel vein and temporal branch of the facial nerve (VII).
Cross section illustrating anatomy of temporal region and close relationship between sentinel vein and temporal branch of the facial nerve (VII).
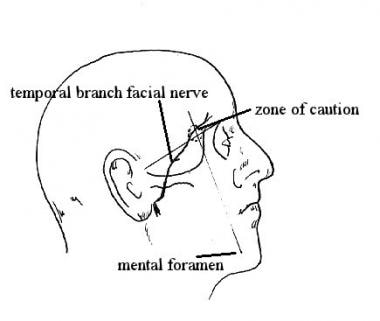 Diagram showing surface anatomy relationship between sentinel vein and temporal branch of facial nerve. Caution zone 10 mm in diameter is drawn at intersection of 2 lines: one extending from the mental foramen to lateral edge of the orbit, and another from the superior edge of the orbit to the junction of the ear helix and zygomatic arch. Perform dissection in this area under endoscopic vision (Trinei, 1998).
Diagram showing surface anatomy relationship between sentinel vein and temporal branch of facial nerve. Caution zone 10 mm in diameter is drawn at intersection of 2 lines: one extending from the mental foramen to lateral edge of the orbit, and another from the superior edge of the orbit to the junction of the ear helix and zygomatic arch. Perform dissection in this area under endoscopic vision (Trinei, 1998).
Muscle anatomy
The frontalis muscle is a broad flat bilateral muscle of facial expression spanning the forehead that raises the eyebrows. Corrugator muscles are small fan-shaped muscles that lie nearly under the eyebrows. They also are muscles of facial expression that cause frowning in the glabellar region. The procerus muscle extends from the upper nose to the lower forehead, and its action wrinkles the upper nose.
For more information about the relevant anatomy, see Forehead Anatomy.
Contraindications
As with eyelid procedures, question patients regarding a history of dry eyes. Excessive brow elevation, especially in conjunction with upper eyelid surgery, can exacerbate a previous condition. Confirm adequate eye tearing or lubrication with a Schirmer test if necessary.
Patients with an excessively high hairline may not be good candidates for this procedure. Contrary to common belief, an endoscopic brow lift raises the hairline at least the distance the brow is elevated, if not more, depending on elasticity of skin and brow. Advise patients with high hairlines that the hairline may appear higher and offer them an anterior hairline approach, which can elevate the brow while shortening the forehead. Disadvantages of the anterior hairline approach are more visible scarring, temporary or permanent scalp paraesthesia, and longer operative time.
Evaluate all cosmetic surgery patients for psychological instability or unrealistic expectations.
-
An aesthetic brow. A-B Lateral brow is at or above medial brow. C-D Brow peak is at lateral limbus of the iris or at junction of medial and lateral thirds of brow. A-E Head of medial brow begins at vertical line extending from nasal ala. B-E Lateral brow may extend to a line drawn from ala through lateral canthus of eye (Gunter JP, Antrobus SD: Plast Reconstr Surg 1997; 99(7): 1808).
-
Cross section illustrating anatomy of temporal region and close relationship between sentinel vein and temporal branch of the facial nerve (VII).
-
Diagram showing surface anatomy relationship between sentinel vein and temporal branch of facial nerve. Caution zone 10 mm in diameter is drawn at intersection of 2 lines: one extending from the mental foramen to lateral edge of the orbit, and another from the superior edge of the orbit to the junction of the ear helix and zygomatic arch. Perform dissection in this area under endoscopic vision (Trinei, 1998).
-
Intraoperative photograph, endoscopic brow lift surgery. In balding patients or patients with high foreheads, obtain endoscopic access with small horizontal incisions directly on the forehead.
-
Endoscopic brow lift. Preoperative photograph of 63-year-old woman.
-
One year after endoscopic brow lift, no fixation performed.
-
Prior to endoscopic brow lift surgery, 65-year-old woman with severe corrugator rhytides and brow ptosis.
-
Postoperative view (2 y), endoscopic brow lift surgery. Patient has improved rhytides and improved brow position; however, note that brow shape has changed little despite medial release. Patient also had laser resurfacing of lower lids. No upper eyelid surgery was performed.
-
Selective elevation of lateral brow can be accomplished by leaving the periosteum intact centrally between the brows.
-
Elevating one brow more than the other requires an asymmetric dissection. As illustrated, dissection on patient's left brow stops at the transition zone, which allows a more permanent elevation of the right brow compared with the left.
-
Fifty-nine-year-old woman at rest, with active corrugator function and asymmetric brow (right lower than left) before endoscopic brow lift surgery.
-
Postoperative photo 2 years after endoscopic brow lift surgery with improvement in glabella and symmetry. Dissection on the right was complete, with dissection on the left not extending past the transition zone, creating an asymmetric lift.
-
Elevating entire brow symmetrically requires complete release of brow down to zygomatic arches, including transition zones at insertion of temporalis muscles.
-
Fifty-five-year-old woman before endoscopic brow lift surgery.
-
Five months after endoscopic brow lift surgery with temporary fixation (9 d), upper blepharoplasty, and facelift.






