Practice Essentials
Extensor tendon lacerations of the hand and fingers are quite common constellations of injuries. Most of these acute injuries to the hand present in the emergency department and are frequently treated there. [1] This fact gives a false sense of security, and the complexities of certain extensor tendon injuries are often incorrectly assessed. An extensor tendon laceration should receive the same diligence as a flexor tendon laceration. More often than not, such injuries should be treated in the operative suite. The soft tissue elements of the dorsal hand and digits are thin in comparison to the flexor side; therefore, dorsal hand and finger injuries are frequently associated with extensor tendon damage. Extensor tendon injuries are also commonly associated with deep structure damage, such as bone, joint, and ligamentous support; up to two thirds of all extensor tendon lacerations have concomitant injuries. [2, 3, 4, 5]
Extensor tendon injuries can be grouped into 2 large categories: 1) acute simple laceration and 2) complex extensor tendon laceration with associated features. Although the diagnosis and treatment of simple lacerations are usually straightforward, certain aspects critical to ensure the optimum outcome are discussed further below. A complex laceration includes associated injuries of surrounding structures or dysfunction that arises from the disruption of the tendon or surrounding structures (eg, mallet finger, boutonniere deformity, sagittal band disorder). [6] This article reviews the current understanding of diagnosis and treatment of the complete range of extensor tendon laceration issues.
A study by Mehrzad et al found that in the United States, complete extensor tendon lacerations of the hand in patients who undergo surgical repair cost an estimated $307 million annually, with the figure possibly reaching $531 million, depending on how worker absenteeism affects core production-based industries. The investigators stated that upward of 91% of the total cost of these injuries is derived from indirect costs (including lost income, missed workdays, and disability payments). [7]
Workup in extensor tendon lacerations
Bedside ultrasonography is more sensitive and specific than physical examination for detecting tendon lacerations. Moreover, bedside ultrasonography in the emergency department takes less time to perform than traditional wound exploration techniques or magnetic resonance imaging (MRI). [8]
A three-view x-ray of the hand, wrist, or forearm must be performed on all but the most benign extensor tendon laceration injuries to rule out foreign bodies or bony injury. Also, in all blunt trauma cases, radiographs are used to evaluate for possible fractures or dislocations.
Management of extensor tendon lacerations
Injuries at the distal interphalangeal joint are treated as follows:
-
Open injury - Lavage and debridement of the joint, tendon repair, skin closure, and K-wire fixation are the principles of management
-
Closed injury - This type of injury should be treated closed, with the single exception of those with an associated fracture involving a large intra-articular fragment (>30% of the articular surface)
-
Established mallet finger deformity - Surgical correction by excision of the redundant scar and prolonged splintage is best for patients with established deformity
-
Associated swan neck deformity - This is best corrected by addressing the distal interphalangeal deformity; alternately, a sliding tenotomy of the central tendon can be performed, taking great care not to produce a boutonnière deformity
For injuries at the middle phalangeal level, repair and immobilize open injuries as for a mallet finger deformity, with the exception that 4 weeks of immobilization is sufficient.
Proximal interphalangeal (PIP) joint–level injuries are treated as follows:
-
Open injury - Treat any laceration over the PIP joint as a central slip rupture until proven otherwise
-
Closed injury - Treat all closed injuries apart from those involving a large intra-articular bony fragment by splintage
-
Established boutonnière deformity - In patients whose boutonnière deformity is fixed rather than mobile, treatment may require surgical release of the contracted volar structures and passive stretching, or it may require merely the latter
-
Swan neck deformity - The Littler oblique retinacular ligament technique for swan neck deformity relocates the one lateral band volarly and inserts it into the volar aspect of the middle phalanx
In a proximal phalanx–level injury, treatment of an open wound involves direct repair and K-wire immobilization.
At the metacarpophalangeal (MP) joint level, the most common injury is the fight bite due to human tooth injury. In these contaminated injuries, primary repair is contraindicated. Once the acute infection has been treated, the swelling has lessened, and the passive range of motion has been restored, repair can be undertaken. Splint the MP joints in a full extension splint for 3 weeks. Of importance, the PIP and distal interphalangeal (DIP) joints should remain free. Use a dynamic extension splint following removal of the full extension splint until no extensor lag remains.
In metacarpal-level injuries, repair all divided structures. A horizontal mattress suture is often better for these flat structures.
In division at the wrist joint, the extensor retinaculum is repaired by Z lengthening.
In thumb injuries, repair to the extensor pollicis longus involves supinating and adducting the first ray and transfixing the involved joint with a K wire.
History Of The Procedure
The history of tendon reconstruction can be traced back to the times of Hippocrates and Galen. Interestingly, Galen (131-201 AD), in his Ars Parva, stated that tendons were composed of both ligaments and nerves. He warned, therefore, that placing sutures in tendons would lead to pain, twitching, and eventual convulsions. This erroneous concept was not refuted until 1682, when Meekren observed that tendons are insensitive and described the successful repair of incompletely severed tendons. Modern tendon repair surgery was promoted by Kirchmayr, who, in 1917, published a method of "locking" suture in tendon repair, variants of which are still in use today. [9]
Anatomical and functional understanding of the extensor system was advanced significantly by Albinus, who first illustrated the basic structure in extensor tendon anatomy in 1734. Further progress of extensor tendon dynamics and balance forces concepts were made by Fowler in 1942. Landsmeer also contributed to the understanding of the extensor system's dynamic interplay with the oblique retinacular ligament in 1949. [2] See Relevant Anatomy for a detailed discussion of anatomy.
Presentation
Extensor tendon laceration can result from various injuries. The most common mechanisms are sharp object direct laceration, crush injury, avulsions, burns, animal or human bites, and deep abrasions. A study by Naito et al found that 88% of patients with a distal radius fracture with a dorsal roof fragment had an extensor pollicis longus (EPL) tendon injury, with 36% of the study’s patients having a laceration. [10]
Extensor lacerations are accompanied by various degrees of skin injury, ranging from minimal (as in puncture wounds) to large avulsions, which can cause significant loss of domain of both elements.
Because of the superficial location of the extensor tendons in the wrist and hand, the laceration often easily directly observed on physical examination with manipulation of the overlying skin. The underlying joint is passively flexed and extended for full visualization of the injury area.
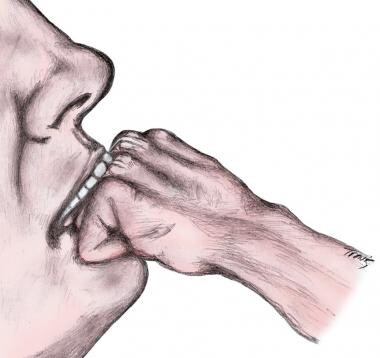
The most common condition wherein the tendon laceration is present outside the area of the skin laceration is the fight bite. In this situation, the metacarpophalangeal joint is flexed and makes contact with an opponent's teeth (see image below). The resultant extensor tendon laceration is located proximal to skin laceration when the hand is in resting position with the MP joints extended, which is the normal position of the hand, especially when being medically examined. In the acute setting, most extensor tendon lacerations exhibit some loss of extensor function, whether it is a decrease in active extension range of motion, decrease in extension strength, or complete loss of extension of affected joints.
In the most straightforward case, the patient presents with one or more digits that stay more flexed than the others when the patient attempts to extend all fingers. This indicates a complete laceration of the extensor tendon on the affected digits. However, if all the extensors in the hand are completely lacerated, then the fingers stay flexed at rest or at attempt to straighten. Also, the position of the fingers does not change regardless of the position of the wrist; this indicates loss of the normal tenodesis effect.
In less straightforward cases, a tendon laceration can be present on examination, but the degree of laceration or surrounding anatomy can hide an extension deficit. Up to 80% of the extensor tendon may be lacerated without loss of function, but the chance of delayed rupture is increased when the laceration includes more than 40% of the tendon. Therefore, the dorsal hand and wrist wound must be explored well when any suspicion of tendon injury exists.
At the wrist, 3 dedicated wrist extensors (extensor carpi radialis longus [ECRL], extensor carpi radialis brevis [ECRB], extensor carpi ulnaris [ECU]) and the finger extensors aid in wrist extension. Therefore, a single wrist extensor laceration can be missed on an initial function examination; thus, careful direct examination must be performed. Finger extension tendon laceration also can be masked. The index and small fingers have 2 extensor tendons apiece, and masking could be present if only one is lacerated. Also, extensor tendon laceration of the dorsal palm occurring proximal to juncturae tendinae may also mask extensor dysfunction. Juncturae tendinae are intertendinous fascia connections that attach diagonally between the tendons of the extensor digitorum communis (EDC).
 Extensor system of the hand. Note the juncturae tendinae that interconnect the extensor digitorum communis (EDC) tendons.
Extensor system of the hand. Note the juncturae tendinae that interconnect the extensor digitorum communis (EDC) tendons.
The purpose of the juncturae is to coordinate the extensor motion of the digits. The interconnection of the juncturae allows continue extension of the affected digit if an extensor tendon laceration occurs proximal to the junctura. Understanding this anatomical subtlety avoids missing the diagnosis of an extensor tendon laceration.
Debris is often present in these wounds, and particles need to be completely cleared for adequate healing, for prevention of infection, and to attain an unobstructed view of injured area. For open dirty wounds of the hand and wrist, after the full sensory examination is complete, local blockage of the extensor area should be performed. This allows adequate cleansing of the wounds without pain or muscle dysfunction, since the extensor muscle bellies and innervations lie much more proximal. After a thorough wound debridement, the direct extensor tendon examination and muscle function testing should be performed.
Indications
As with most normal structures, significant disruption should be repaired when possible. Most lacerations of the extensor system should be repaired. However, certain lesser degree lacerations can do well without repair. A laceration of the extensor over the proximal phalanx involving 40% of tendon, in which the patient can extend the finger against resistance, do well with or without repair. [11] Small partial extensor lacerations can sometimes demonstrate triggering but do not exhibit the delayed rupture exhibited by lacerations of >40% of the extensor tendon. The general principles and timing of management for extensor tendon injuries are similar to those for flexor tendon injuries. In combined repairs, flexor tendon rehabilitation must take priority.
Associated fractures are common with extensor injuries in the digits. In closed injury over the dorsum of the proximal interphalangeal (PIP) joint, suspect extensor tendon injury. Because of the superficial nature of the extensor tendons and the lack of significant delicate and critical adjacent structures (as opposed to the presence of the neurovascular bundle in a flexor tendon injury) these repairs can be performed immediately in the emergency department, urgent care, or office setting, given the proper lighting and instruments. [1, 12] (For a detailed description of extensor tendon repair in an emergency department or office setting, see Medscape Reference article Extensor Tendon Repair.) If the repair is likely to be complicated by injury to additional structures, an operating room is the best setting for the repair. [12]
When deciding when and where to perform an extensor repair, one of the first questions to address is infection risk due to contamination of the wound. An extensor tendon laceration wound that is not infected or severely contaminated can be repaired immediately. Extensor tendon laceration wounds with significant debris contamination or high risk of future infection (eg, fight bites) must be taken to the operating room for a thorough debridement and washout before repair. The nature of this type of contamination requires optimal lighting, instruments, and surgical support uniquely found in the operating suite. At the completion of the debridement, the clinical decision must be made whether to directly repair the extensor tendon or delay the repair for a course of antibiotics and observation to avoid wound infection.
A study by Al-Qattan indicated that partial extensor tendon lacerations greater than half the width of the tendon can be conservatively treated by immediate nonresistive active mobilization (4 wks), followed by resistive exercises, without the employment of splints or sutures. Specifically, this applied to lacerations in zones II, IV, and VI-VIII of the fingers and II, IV, and V of the thumb. The study included 39 patients, all of whom achieved full range of motion without extension lags by 8- to 9-month follow-up. [13]
Relevant Anatomy
As with all disorders of the hand, diagnosis and correct therapy application hinges on a thorough understanding of the relevant anatomy. [14, 15] The upper extremity contains 12 extensor tendons. These tendons comprise an extensor system that dorsally maneuvers the wrist, thumb, and all fingers. Extensor tendons also participate in the radial and ulnar deviation of the wrist and contribute to the supination and pronation of the wrist and thumb. The primary origin site is the lateral epicondyle of the humerus and proximal forearm.
As the extensor tendons travel from proximal to distal, they form an arrangement that can be described as a deep group and a superficial group. The superficial group consists of extensor carpi radialis longus (ECRL) and extensor carpi radialis brevis (ECRB), the extensor digitorum communis (EDC), the extensor digiti minimi (EDM [otherwise known as extensor digiti quinti]), and the extensor carpi ulnaris (ECU). The deep group comprises the abductor pollicis longus (APL), the extensor pollicis longus (EPL), the extensor pollicis brevis (EPB), and the extensor indicis proprius (EIP). Also coursing along with the tendons in the deep compartment is the deep branch of the radial nerve, which is otherwise referred to as the posterior interosseous nerve (PIN). It provides innervation to all the aforementioned extensor tendons. See the table below for a complete extensor tendon list.
Table. Extensor Tendons of the Hand (Open Table in a new window)
Abbreviation |
Full Name |
Insertion |
Function |
Origin |
Ext. Compartment |
APL |
Abductor pollicis longus |
Base on thumb metacarpal |
Abduction of thumb |
Proximal radius and ulna, interosseous ligament |
I |
EPB |
Extensor pollicis brevis |
Base of thumb proximal phalanx |
Extension of thumb proximal phalanx |
Proximal radius and interosseous ligament |
I |
ECRL ECRB |
Extensor carpi radialis longus/brevis |
Base of metacarpal II Base of metacarpal III |
Extends and abducts hand |
Lateral epicondyle |
II |
EPL |
Extensor pollicis longus |
Distal phalanx of thumb |
Extends thumb IP joint |
Proximal ulna |
III |
EDC (4 tendons: II - V) |
Extensor digitorum communis |
Proximal and mid. phalanges of digits II-V |
Extends digits II - V |
Lateral epicondyle |
IV |
EIP |
Extensor indicis proprius |
Extensor hood of digit II |
Extends digit II |
Proximal ulna and interosseous membrane |
IV |
EDM (EDC) |
Extensor digitorum minimi (quinti) |
Proximal phalanx, digit V |
Extends digit V |
Lateral epicondyle |
V |
ECU |
Extensor carpi ulnaris |
Base of metacarpal V |
Extends and abducts hand |
Lateral epicondyle and proximal ulna |
VI |
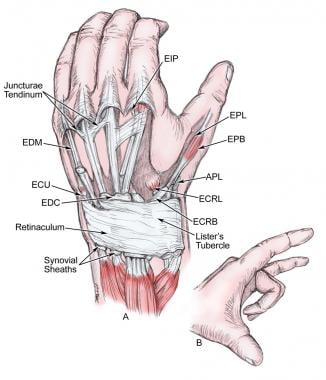
As the extensor tendons cross the wrist, they course under the extensor retinaculum. The extensor retinaculum prevents the tendons from dorsal displacement caused by natural tendency to develop a straight line from tendon origin to insertion, known as bowstringing, and is divided into the tendons in 6 extensor compartments by vertical septae. See the image below.
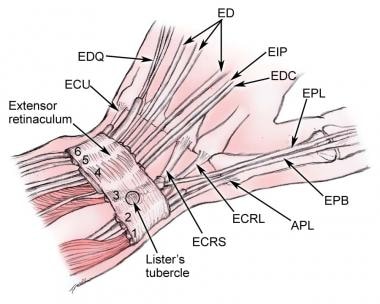 The extensor tendons of the wrist and hand are divided into 6 compartments at the dorsal wrist, each containing specific tendons.
The extensor tendons of the wrist and hand are divided into 6 compartments at the dorsal wrist, each containing specific tendons.
The first extensor compartment contains the EPB and the APL. The second compartment contains the radial wrist extensors, the ECRL and ECRB. The third compartment is occupied by the EPL. The EPL is notable for the diagonal course that it takes after it deviates around the dorsal radius bony protrusion called the Lister tubercle. The EIP and the 4 EDC tendons make up the fourth compartment. The fifth compartment holds the EDM tendon, and the sixth compartment holds the ECU.
The tendons travel distally past the extensor retinaculum to their insertion sites. The ERCL inserts on the dorsal base of the index metacarpal. The ECRB inserts on the dorsal base of the long finger metacarpal, as it is the most central extensor tendon. This fact is important to note when tendons are selected for tendon transfer. The ERCB should not be used for a transfer donor tendon, if possible, because the resultant wrist extension will deviate to the radial or ulnar side because of the laterality of the remaining tendons.
All the extensor tendons to the hand are extrinsic, that is, no tendons that extend the digits originate in the hand. As the digital extensors travel over the hand, dorsum extensor juncturae tendinae are formed to cause interconnections between tendons. These interconnections are important to understand when evaluating extensor injuries. Juncturae tendinae can cause a misdiagnosis of an extensor tendon laceration because they can aid continual extension of a digit whose tendon was cut proximal to the juncturae. See the image below.
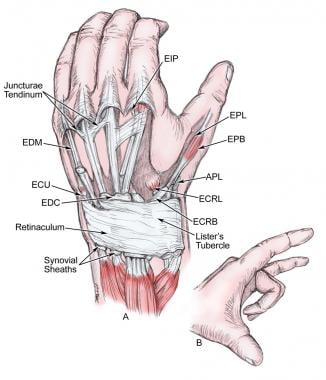 Extensor system of the hand. Note the juncturae tendinae that interconnect the extensor digitorum communis (EDC) tendons.
Extensor system of the hand. Note the juncturae tendinae that interconnect the extensor digitorum communis (EDC) tendons.
Several unique aspects of the extensor tendon system are important to note. Unlike the flexor tendons, extensor tendons do not have flexor sheaths except for at the wrist, as tendons pass below the extensor retinaculum. The EDM tendon is usually split into 2 separate slips as it crosses over the wrist and travels to the metacarpophalangeal (MP) joint. The fifth dorsal compartment, in which the EDM travels, is located just dorsal to the distal radioulnar joint. [16] The EDC tendon to the small finger is estimated to be absent in 54% of the population. [17]
Extensor apparatus of the fingers
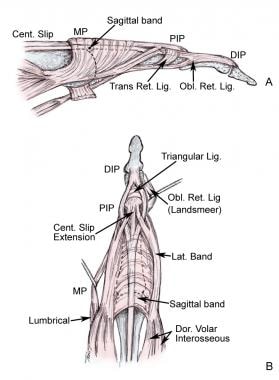
The extensor apparatus of the fingers is called an apparatus or system because of the complex interplay between the multiple extensor tendons, the intrinsic muscle system, and the many interconnecting ligaments between the tendons and the volar plates. The extensor apparatus of the digits begins just proximal to the MP joints. See the image below.
As the extensor tendons travel over the MP, a dorsal sling of transverse fibers is present. The sling attaches to the extensor tendon dorsally and passes palmarward on each side of the MP joint to attach to the volar plate and the transverse metacarpal ligament. This dorsal sling is called the sagittal band. These transverse fibers are layered in a crisscross pattern that changes its arrangement as the finger flexes and extends. [16]
MP joint extension is accomplished by the contraction of the finger extensor tendons and its attachment to the proximal phalanx via sagittal band fibers. The sagittal band acts both as a static tether to prevent radial or ulnar displacement of the extensor tendon and as a dynamic tether that allows proximal and distal gliding of the extensors tendons during flexion and extension. Complete laceration of the sagittal bands on either side can cause instability in the extensor tendon position as it travels across the MP joint. Laceration to the radial side of the sagittal band causes far more instability than injury ulnar side. [18] Complete laceration of one side of the sagittal band causes a subluxation of the extensor tendon to the opposite side of the laceration when the MP joint is flexed. When the MP joint is extended and tension is removed from the EDC, the tendon snaps back into the central position.
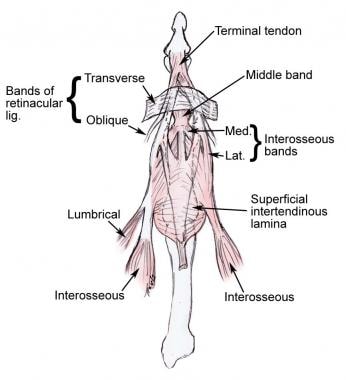
The extensor apparatus becomes a complex interplay of intrinsic muscle contribution as it travels from the MP joint distally. Three intrinsic sets of muscles (volar interossei, dorsal interossei, and lumbricals) contribute dynamic function to the extensor system through the lateral slips. See the image below.
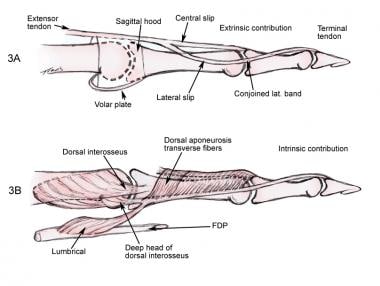 Both the intrinsic muscle and the extensor digitorum communis (EDC) tendon dynamically contribute to the extensor system of the digits.
Both the intrinsic muscle and the extensor digitorum communis (EDC) tendon dynamically contribute to the extensor system of the digits.
The tendons of the interossei muscles split in two; the superficial slip inserts on the proximal phalanx (causing MP flexion), and the deep tendon becomes part of the lateral slip. Interossei muscles contribute to the lateral slip on both sides of the finger while the lumbrical tendons only join the lateral slip on the radial side.
In discussion the extensor mechanism, some confusion often arises in the terminology of lateral slips and lateral bands. The lateral slip is the tendon by which the intrinsic muscle contributes (as just previously discussed) to the extensor mechanism. The lateral band is the extrinsic contribution (EDC tendon) to the extensor mechanism. The lateral slip and lateral band join together distal to the central slip insertion to make up a conjoined lateral band. The lateral slip gives tendon attachments to the central slip and terminal tendon to help extend the proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints. Likewise, the EDC tendon provides the major portion of the central slip. It splits into 2 tendinous branches on either side of the central slip, which join with the lateral slip to make the conjoined lateral band. Finally, both sides merge to form the terminal tendon, which inserts on the dorsal aspect of the distal phalanx and extends the DIP.
Between, around, and over this extensor system array are ligaments and fascial constructs (also called the reticular system), which aid the function and interplay of the extensor tendons. See the image below.
The principal components of the retinacular system are the transverse and oblique ligaments (eg, Landsmeer ligament). The transverse fibers originate from the flexor sheath and proximal phalanx on the volar aspect, pass through a window in the Cleland ligament, and insert into the lateral bands and triangular ligament dorsal to the axis of proximal interphalangeal joint rotation. The deeper and more tendinous oblique retinacular ligament arises from the volar proximal interphalangeal joint capsule and proximal two thirds of the middle phalanx and inserts distally into the conjoined tendon (conjoined lateral band).
Distal to the proximal interphalangeal joint, the lateral bands first are separated by a triangular ligament and then fuse to form a conjoined tendon, which inserts into the base of the distal phalanx. The extensor hood is free to slide proximally with MP extension and distally with MP flexion. With the hood in the distal position, the interossei contribute to MP flexion through their vertical fibers, with little effect on the interphalangeal joints. With the hood in the proximal position and the MP joints fixed in extension, the interossei, through the oblique fibers of the lateral bands, are able to extend the interphalangeal joints.
Conversely, the lumbrical muscles are effective IP extensors irrespective of the degree of MP flexion. Similar to the interossei, they provide flexion of the MP joint via their vertical fibers. The lateral bands normally lie dorsal to the axis of motion of the extended PIP joint and shift volarward with PIP flexion. The triangular ligament prevents the lateral bands from shifting volar to the axis of motion to become flexors of the PIP joint. The primary function of the EDC is MP function, but with full MP extension or MP extension blocked, the EDC can extend the IP joints. The EPL traverses the third dorsal compartment of the wrist. It adducts and supinates the first ray and extends the MP and IP joints.
The extensor pollicis brevis and abductor pollicis longus are important stabilizers of the first metacarpal base. The extensor pollicis brevis extends the carpometacarpal and MP joints, inserting into the base of the proximal phalanx. It occasionally inserts into the distal phalanx, as well. The anatomy of the thumb MP joint resembles the PIP joint anatomy of the digits. The adductor and abductor pollicis longus tendons contribute to a dorsal expansion, which has transverse fibers acting like the retinacular system to stabilize the tendons of extensor pollicis brevis and extensor pollicis longus. The intrinsics are able to extend (but not hyperextend) the IP joint through fibrous interconnections in the dorsal expansion.
-
Extensor system of the hand. Note the juncturae tendinae that interconnect the extensor digitorum communis (EDC) tendons.
-
The extensor tendons of the wrist and hand are divided into 6 compartments at the dorsal wrist, each containing specific tendons.
-
Depiction of sagittal bands, lateral bands, and the relationship of the ligamentous structures.
-
Both the intrinsic muscle and the extensor digitorum communis (EDC) tendon dynamically contribute to the extensor system of the digits.
-
Extensor retinacular system.
-
Regions of the dorsum of the hand have been divided up into extensor zones to further describe the location of an extensor tendon laceration. Defining a laceration per zone area enables better communication and relates to the complexity of the needed repair.
-
Primary closure of thumb extensor tendon laceration with the figure-of-8 technique.
-
Kirchmayr tendon laceration repair suture technique.
-
Four common core and epitenon tendon repair suture techniques.
-
Swan-neck deformity.
-
Boutonniere deformity.
-
Fight bite.