Background
This review covers primary fractures and dislocations involving the wrist region. The wrist is composed of the anatomic region between the forearm and the hand. Its ability to place the hand in 3-dimensional space is essential for normal daily function of the upper extremity. Over the last few decades, significant advances have occurred in the understanding of wrist anatomy, pathophysiology, and carpal kinematics. Even so, some wrist injuries remain a diagnostic enigma, while others remain frustrating to treat either conservatively or with operative intervention.
Epidemiology
Frequency
In the Western world, the most common orthopedic fractures are distal radius fractures. Peak incidence is found in young men and postmenopausal women. [1]
Approximately 14% of all hand fractures are carpal fractures. Scaphoid fractures are by far the most common of the carpal fractures, estimated at 70-79%. Fractures of the triquetrum make up an estimated 14% of all carpal fractures, trapezial fractures make up 2.3%, and hamate fractures make up 1.5%. Lunate, pisiform, and capitate fractures combine for 3% of all carpal fractures. Trapezoid fractures are rare, encompassing 0.2% of all carpal fractures.
Injuries occur more commonly in young, active, and energetic males and are also common in osteoporotic elderly persons. The demographics may vary by season, as fractures in children seem to be more common in the warmer months while those in adults increase in the colder months. The overall incidence of these fractures appears to be increasing over time.
One retrospective study on carpal fractures in Singapore found that the prevalence of carpal fractures in this population was consistent with findings of studies in other countries. Isolated scaphoid and other carpal fractures were more common in men compared with women (male-to-female ratio of 13:1), and the mean age of those experiencing these fractures was 26 years. Military conscription was identified as an at-risk activity predisposing to carpal fracture. [2]
Etiology
Most wrist fractures and dislocations are a result of axial loading on the outstretched palm and extended wrist, usually from a fall on outstretched hand (FOOSH), motor vehicle accident, or sports contact injury. Most result in fractures of distal radius, scaphoid, and other carpal bones. Higher-impact injuries from falls or severe motor vehicle accidents can lead to more complex fracture/dislocation patterns of the wrist (ie, perilunate fracture/dislocation).
Pathophysiology
Scaphoid Fractures
Fractures of the scaphoid represent the most common carpal fracture, accounting for 60-70% of all carpal fractures. Fracture of the scaphoid has been explained as a failure of bone caused by a compressive tension load, by torsion, or by rotation forces. This is usually seen in a FOOSH type injury and is typically characterized by dorsiflexion and ulnar deviation. However, with dorsiflexion (95-100°) and radial deviation (10°), the scaphoid becomes trapped between the volar edge of the radius proximally and the trapezium and trapezoid distally at the level of the radioscaphocapitate ligament, thereby fracturing the scaphoid through impaction.
The most common site of fracture within the scaphoid is the anatomic waist (70-80%). These fractures may be stable or unstable, depending on the orientation of the fracture line (see below). Of scaphoid fractures, 15-20% occur at the proximal pole, while 10-15% occur through the distal pole of the scaphoid.
Several classification systems have been proposed for scaphoid fractures.
Russe described scaphoid fractures on the basis of orientation, including horizontal oblique, vertical oblique, and transverse fractures. The vertical oblique fracture is considered to be the least stable and most likely to require surgical intervention.
One of the other commonly employed classification systems was described by Herbert. In this system, the author combines fracture anatomy, stability, and chronicity of scaphoid fractures in an alphanumeric system (below).
-
Type A fractures are stable acute fractures, including fracture of the tubercle (A1) and incomplete fractures of the scaphoid waist (A2).
-
Type B fractures are unstable and include distal oblique fractures (B1), complete fracture of the waist (B2), proximal pole fractures (B3), and transscaphoid perilunate fracture dislocation of the carpus (B4).
-
Type C fractures are characterized by delayed union.
-
Type D fractures are characterized by established nonunion and either fibrous union (D1) or pseudarthrosis (D2).
The diagnosis of fracture displacement or instability includes the following:
-
Translation or gap at the fracture site ≥1 mm on any x-ray view
-
Greater than 15° dorsal angulation of the lunate with respect to the radius
-
Carpal height ratio of the affected side less than the opposite side by at least 0.03
-
Scaphoid length >1 mm shorter than the contralateral side
Understanding that the carpal configuration is in carpal rows is useful (see Relevant Anatomy). The carpus can be thought of as a 3-bar linkage system, with the radius, proximal row (ie, lunate, triquetrum), and distal row (ie, hamate, capitate, trapezoid, trapezium) aligned in a linear fashion (see image below).
 Diagrammatic representation of the common transscaphoid perilunate fracture dislocation of the wrist.
Diagrammatic representation of the common transscaphoid perilunate fracture dislocation of the wrist.
The scaphoid acts like a bridge between the proximal and distal rows and provides carpal stability. Under compressive forces, the scaphoid flexes. The counterbalance to this is the natural extension of the triquetrum. Both bones try to influence the lunate through their respective ligamentous attachments, but in opposite directions (see image below).
Once scaphoid integrity is lost, an imbalance occurs and the lunate extends and assumes a dorsal tilt (see DISI below). Through the scapholunate ligament complex, the proximal pole of the fractured scaphoid also assumes an extended (dorsal) position. However, the distal fragment of the scaphoid is still loaded by the overlying trapezium and trapezoid, which causes the fragment to flex in a volar direction, thereby leading to the so-called humpback deformity.
With the loss of colinearity, the entire carpus becomes unstable and subject to collapse. The lunate and proximal row lie dorsal, thus the term dorsal intercalated segment instability (DISI). These forces result in a large gap at the fracture site and an increased incidence of delayed union, malunion, and nonunion.
The blood supply of the scaphoid is largely interosseous and oriented in a distal to proximal direction. Therefore, with fractures of the scaphoid waist and, especially, the proximal pole, this tenuous blood supply can become interrupted, thereby predisposing the proximal pole to avascular necrosis (AVN) with an incidence approaching 100%. Fractures of the middle third are similarly associated with a 30% incidence of avascular necrosis, while less than 15% of distal pole fractures lead to avascular necrosis.
Lunate Fractures
Lunate fractures account for approximately 1% of all carpal fractures (excluding Kienböck disease). Lunate fractures may also occur with axial loading to the dorsiflexed wrist. However, lunate fractures are correlated more with ulnar deviation of the wrist during impact.
Lunate fractures can be difficult to diagnose; therefore, they may be difficult to treat.
Lunate fractures are thought to invariably precede Kienböck disease, which occurs when the lunate undergoes avascular necrosis. This eventually leads to collapse of the carpus in a predictable, progressive pattern and, ultimately, pancarpal arthritis.
Five types of lunate fractures have been described, based on location and vascular supply.
Palmar pole (most common) fractures (affect the palmar nutrient artery)
Osteochondral (chip) fractures of the proximal articular surface (do not affect vascularity)
Dorsal pole fractures (may affect the dorsal nutrient artery)
Sagittal-oblique through the body
Coronal split of the body
Type 1 fractures result from hyperextension and compression from the capitate and radius; the radiolunate and lunotriquetral ligaments pull in radial and ulnar directions, respectively. The distal palmar pole is avulsed by the lunotriquetral ligament.
Type 2 fractures may be a result of Kienböck disease but may also result from shearing related to lunate dislocation or subluxation.
Type 3 fractures result from shear force as the capitate dislocates dorsally in perilunate dislocation or from avulsion of the scapholunate ligament in acute rotatory subluxation of the scaphoid.
Type 4 fractures result from shear forces induced from a radial carpal fracture dislocation.
Type 5 fractures result from hyperextension as the short radiolunate ligament avulses the palmar pole while the capitate forces the lunate into extension. This also happens in palmar perilunate dislocation as a shear force.
Kienbock Disease
In 1910, Kienböck described lunate collapse as the result of progressive vascular compromise resulting from repetitive wrist sprains and contusions. They are now understood to be characteristic lesions from failure of the lunate fractures to unite (often the dorsal pole).
The incidence and progression of Kienböck disease relies on a combination of "at-risk" factors. These include ulnar (minus) variance, lunate geometry, lunate vascular pattern, triangular fibrocartilage complex compliance, intraosseous pressure gradients, vocational loading, and underlying congenital and developmental disorders.
All factors are pathophysiologically important, each to varying degrees. However, describing and understanding the concept of ulnar variance is the most relevant clinically.
Ulnar variance refers to the distance between the articular surfaces of the radius and ulna (with a standard anteroposterior radiograph, the shoulder is abducted to 90º and the palm of the hand is on the radiograph plate). Ulnar-minus infers that the ulna is relatively short with respect to the radius and the articulating surface, and vice versa. Inequality in the length of the forearm bones leads to differential stress-loading of the lunate, which is one of the factors leading to the disease process.
During impact on a dorsiflexed and ulnarly deviated wrist, a short ulna contributes to the stress forces across the lunate and contributes to fracture, thus explaining the correlation with ulnar-minus variance and the incidence of Kienböck disease.
This concept forms the basis of various surgical procedures designed to unload the lunate by transferring the load to more lateral carpal columns in the treatment of Kienböck disease.
Kienböck disease is best divided into 4 stages based on radiological progression of the disease.
-
Stage I: Radiographic findings are normal, but the bone scan findings are positive for disease. MRI shows a decreased signal on T1- and T2-weighted images.
-
Stage II: Sclerotic changes and fractures are visible on radiographs; however, carpal integrity is intact.
-
Stage III (A and B): This stage occurs when the lunate collapses and the capitate migrates proximally. In stage IIIA, no fixed carpal derangement is noted. In stage IIIB, decreased carpal height, ulnar migration of the triquetrum, scapholunate dissociation, and flexion of the scaphoid are noted.
-
Stage IV: This stage is associated with additional carpal degeneration and generalized arthritis.
A study by Rhee et al indicated that the severity of Kienböck disease is influenced by lunate morphology, with lunates bearing a medial hamate facet (type II lunates) offering more protection against the disease than lunates without this feature (type I lunates). The study involved 106 wrists, including 75 with type I lunates and 31 with type II lunates. The investigators found that Kienböck disease tended to be significantly more advanced at presentation in the type I lunate wrists than in those with type II lunates. In addition, type I lunates had a higher rate of coronal fractures than type II lunates (77% vs 58%), and type II lunates seemed to be more resistant to scaphoid flexion deformities. [3]
Triquetrum
Triquetral fractures are the second most common carpal fracture. These fractures are usually not seen in isolation, and the most common presentation is with other carpal injuries that are boney, ligamentous, or both (ie, perilunate fracture dislocation). The vascular supply of the triquetrum contains rich vascular networks and numerous intraosseous anastomoses, making nonunions exceptionally rare. Triquetral fractures may be divided into 3 types based on radiographs.
Dorsal cortical fractures (most common)
Body fractures
Volar avulsion fractures
The mechanism of chip fractures has been debated. Some think the mechanism is due to avulsion of the conjoined insertion of the dorsal intercarpal or dorsal radiocarpal ligaments with hyperextension and radial deviation, while others think it is due to direct impact from the ulnar styloid or hamate with wrist hyperextension.
Trapezium
The trapezium fracture is the third most common carpal fracture. Five types of trapezial fractures exist and are based on radiographic findings.
Vertical transarticular (most common) - Most likely due to axial force along the thumb metacarpal bone
Horizontal - Due to direct shearing forces
Dorsal radial tuberosity - Due to vertical shearing forces
Anteromedial ridge - Due to anteroposterior crush injury
Comminuted
Trapezoid
The trapezoid fracture is rare. Standard radiographs often fail to demonstrate trapezoid fractures. A computed tomography (CT) or magnetic resonance imaging (MRI) scan may be needed to diagnose a fracture of the trapezoid. Two types of trapezoid fractures exist.
Dorsal rim
Body
These fractures are rare and are usually associated with fracture dislocation that involves dislocation of the index metacarpal or the trapezoid itself. The force is usually axial along the index metacarpal bone.
Capitate
Capitate fractures are thought to occur with a frequency of less than 1%. The proximal pole is entirely intra-articular and without soft tissue attachment. These fractures are usually identified on CT or MRI, using a high degree of suspicion. Capitate fractures can be categorized into 4 types.
Transverse (axial body; most common)
Transverse (axial proximal pole)
Coronal oblique
Parasagittal
Types 1 and 2 occur with extreme dorsiflexion. The transverse fracture of the neck of the capitate in conjunction with a fracture of the waist of the scaphoid has been referred to as the scaphocapitate syndrome. Malrotation of the proximal capitate (rotating with the proximal scaphoid fracture fragment) fracture usually occurs, and many believe that this represents a variant of the perilunate pattern of injury. The other types of capitate fractures occur as a result of hyperextension, axially loading injuries, or both.
Hamate
Hamate fractures are most common in stick- or bracket-handling sports (eg, golf, baseball, tennis). The vascular supply is most tenuous at the waist of the hamate hook. Two types of hamate fractures exist.
Hook fractures
See the list below:
-
Avulsion (tip)
-
Waist
-
Base
Body fractures
See the list below:
-
Proximal pole
-
Medial tuberosity
-
Sagittal oblique
-
Dorsal coronal fractures
Hook fractures have several causes. Fractures can result from a direct blow or from repetitive contusions with a handle (golf, baseball) or racket (tennis, squash). Indirect avulsions through forceful pull of the flexor carpi ulnaris (FCU) and avulsion through the pisiform hamate ligament can cause hook fractures, as can a crush injury. Because of the tenuous vascular supply, nonunions of the hook of the hamate are common.
Body fractures can result from severe wrist fracture-dislocation, a direct blow to the ulnar aspect of the hand, anteroposterior crush injury, or transcarpal-carpal metacarpal dislocations, resulting in dorsal coronal fractures with posterior subluxation of the fourth and fifth metacarpal bones.
Pisiform
Often regarded as a proximal carpal bone, it is truly a sesamoid bone within the FCU tendon substance. Pisiform fractures fall into 4 broad categories.
Transverse (most common)
Parasagittal
Comminuted
Pisotriquetral impaction
The most common mechanism is a fall or impaction directly on the pisiform (or hypothenar eminence) with the wrist extended. Active firing of the FCU simultaneously with the direct impaction may result in transverse avulsion fractures; also ADM co-contraction may cause ulnar border avulsion fractures.
Perilunate Dislocation and Fracture Dislocation
Seven percent of carpal injuries fall into this category. Cooney et al classified carpal dislocations to 5 categories. [4]
Dorsal perilunate dislocation (lesser arc injuries)
Transcarpal fracture dislocation (greater arc injuries)
Radiocarpal dislocation
Longitudinal (axial dislocation)
Isolated carpal dislocation
These transcarpal injuries result from more extreme hyperextension injuries of the wrist such as violent motor vehicle accidents or high-impact falls. The position of the wrist and magnitude and direction of the fall or impact determine the fracture/dislocation pattern.
Fracture dislocations, or greater arc injuries, are twice as common as pure ligamentous dislocations (lesser arc).
The pathophysiology focuses on zones of vulnerability where most carpal fractures and dislocations occur. The potential lines for cleavage around the lunate can be divided into a lesser arc and a greater arc (see image below). The lesser arc is the ligamentous zone surrounding the lunate bone, and injury to this zone results in perilunate dislocation. The greater arc consists of the bony structures surrounding the lunate, including the scaphoid, trapezium, capitate, hamate, and triquetrum. Combined fracture and ligament disruption to this zone results in a typical perilunate fracture-dislocation pattern.
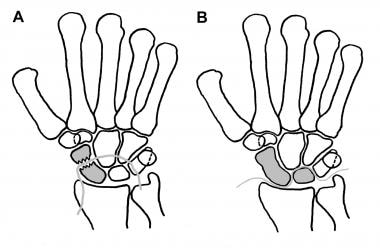 A is the greater-arc or transscaphoid perilunate dislocation pattern. B is the lesser-arc or perilunate dislocation pattern.
A is the greater-arc or transscaphoid perilunate dislocation pattern. B is the lesser-arc or perilunate dislocation pattern.
Perilunate dislocations
Lesser-arc injury is best understood within the context of progressive perilunate instability. This concept describes a predictable sequence of ligamentous injury leading to perilunate and lunate dislocation as described by Mayfield et al. [5]
-
Stage I includes scaphoid dissociation from tearing of the scapholunate interosseous and volar displacement of the radioscaphoid joint.
-
Stage II includes dorsal dislocation of the capitate with dissociation at the lunocapitate joint.
-
Stage III (perilunate dislocation) includes lunotriquetral ligament disruption. The lunate remains aligned with the radius, while the rest of the carpus is displaced, usually dorsally.
-
Stage IV (volar lunate dislocation) is complete ligament disruption. The capitate remains aligned with the radius, while the lunate is squeezed out in a volar direction.
Perilunate (stage III) and lunate dislocations (stage IV) display different dislocation patterns and alignments, yet they are understood to be manifestations of the same progressive disease.
Perilunate fracture dislocations
Greater-arc injuries are characterized by complete loss of contact between the lunate and head of the capitate and one or more fractures of bones surrounding the lunate.
Several potential patterns for disruption are possible. In all cases, disruption occurs through the greater arc, while the dorsal intercarpal ligaments remain intact; thus, the distal carpal row is displaced dorsally and proximally over the proximal row.
The maximum point of force may be initiated at the radial styloid and extend through the scapholunate interosseous ligament through to the lunotriquetral joint. Alternatively, the point of maximum force may begin at the scaphoid waist and tear through ligaments until the capitate, hamate, triquetrum, and distal scaphoid are carried away from the lunate and proximal scaphoid.
Alternatively, if the force is directed through the scaphoid, this may then be propagated interosseously, fracturing the capitate and tearing through to the triquetrum. In all cases, the triquetrum can fracture directly or tear at the lunotriquetral ligament.
Simply, the carpal fractures can be classified into 3 stages.
-
Stage I is transscaphoid dislocation.
-
Stage II includes transcapitate dislocation in addition to stage I features (transscaphoid, transcapitate perilunate).
-
Stage III consists of transscaphoid, transcapitate, and transtriquetral (body or avulsion) with or without hamate disruption.
Axial Dislocation and Fracture Dislocation
This describes global disruption of the carpus into longitudinal patterns parallel to the long axis of the limb. Injuries occur in industrial accidents in which machinery applies high-energy force combined with dorsal and palmar compression to the hand.
The incidence of axial carpal disruption has been estimated at 1.4-2.08% of patients with carpal fracture dislocations or subluxations. Variables include magnitude, velocity, duration, and angle point of application of force. Parallel compression results in dislocation, whereas pressure under more oblique angles also results in fractures. In addition to universal tearing of the flexor retinaculum, important intercarpal ligament tears (eg, palmar hamate-capitate, palmar capitate-trapezium) disrupt the normal springlike integrity of the carpal arch. The wrist can split into 2 or more columns, usually with the metacarpals displacing along with the corresponding carpal bones.
Garcia-Elias et al described 2 major groups of injuries in this category. [6]
Axial ulnar
See the list below:
-
Transhamate, peripisiform
-
Perihamate, peripisiform
-
Perihamate, trans-triquetrum
Axial radial
See the list below:
-
Peritrapezoid, peritrapezium
-
Peritrapezium
-
Trans-trapezium
Most fractures are of the axial-ulnar type, in which injury is often at or around the hamate and capitate (see figure A in the image below). An ulnar column is created that is displaced proximal and ulnar. Axial-radial dislocation occurs when the ulnar carpus remains aligned but the radial carpus is displaced (see figure B in the image below). Usually, the trapezium is dislocated along with the first metacarpal, or a combined trapezoid-trapezial dislocation can occur with the first, second, and third metacarpals. In the axial radial dislocation, combined axial-radial-ulnar dislocation has also been reported.
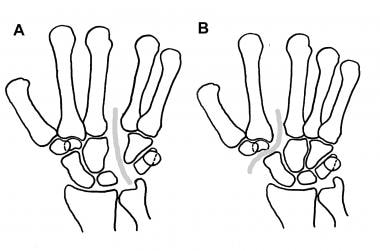 A is ulnar axial dislocation (fracture pattern also possible). B is radial axial dislocation (fracture pattern also possible).
A is ulnar axial dislocation (fracture pattern also possible). B is radial axial dislocation (fracture pattern also possible).
Isolated Carpal Dislocations
Isolated carpal dislocations are extremely rare and a challenge to treat.
Lunate dislocations are the most common type and occur in the context of progressive stage IV perilunate instability.
Dislocation is almost always in a palmar direction. The rare dorsal dislocation occurs during wrist flexion injury.
Scaphoid dislocation occurs with forceful dorsiflexion while an object is grasped and the wrist is ulnarly deviated. The 2 clinical types that have been reported are isolated anterolateral dislocation of the proximal pole of the scaphoid and scaphoid dislocation associated with an axial derangement of the capitohamate joint.
Triquetral dislocations occur in a palmar and dorsal direction. Palmar dislocation can contribute to carpal tunnel pressures and lead to median nerve compression.
Pisiform dislocation occurs with injury directly to the ulnar carpus or hyperextension traction of the flexor carpi ulnaris that tears the pisohamate or pisometacarpal ligaments.
Trapezoidal dislocations may occur from a dorsal blow to the second metacarpal during wrist flexion. Because of the pyramidal shape of the trapezoid and the weak dorsal ligaments, the trapezoid is usually dislocated in a dorsal direction.
Trapezium dislocations occur in dorsal and palmar directions. They occur with crush injuries either alone or with radial-axial dislocations.
The hamate may be dislocated in both dorsal and palmar directions. Direct, indirect, or a severe crush-type trauma usually manifests as axial dislocation.
Presentation
Most patients with wrist injuries present with a history of a fall on an outstretched palm and extended wrist.
Scaphoid fractures
This usually manifests as pain and swelling of the radial wrist after a traumatic event, usually a fall on the outstretched hand or a motor vehicle accident. The classic presentation is swelling in the anatomic snuffbox, although this is not specific to scaphoid fractures alone.
Physical examination may reveal a limited range of motion. Palpation in the anatomic snuffbox (interval between the extensor pollicis longus ulnar/dorsal and the abductor pollicis longus and extensor pollicis brevis radial/volar) often elicits pain. Tenderness is usually found upon radial deviation and flexion of the wrist, and pain is usually found with the Watson maneuver. Another useful sign may be pain with scaphoid compression via axial load to the first metacarpal. Patients not uncommonly present with diminished grip strength when compared to the contralateral wrist. Patients may present with pain and tenderness months after a traumatic event; in this situation, the pain is often a vague and aching pain, usually on the radial side of the wrist.
Lunate fractures
Uncomplicated lunate fractures usually manifest as simple wrist sprains or can remain painless. Upon palpation, dorsal tenderness may be observed between the Lister tubercle and the third metacarpal base.
Most fractures are difficult to diagnose, and patients may not present until avascular necrosis has already occurred. The patient presents with chronic wrist pain and tenderness localized dorsally over the lunate. Diffuse swelling and grip weakness may be observed. Disease progression involves stiffness, clicking, crepitation, and grinding, with increasing pain as time passes after the inciting traumatic event.
Triquetral fractures
Triquetral fractures are most commonly associated with other carpal injuries and can be seen with both perilunate and axial ulnar injury. Isolated fractures are seen less frequently. They can result from a fall with the wrist in extension and ulnar deviation. Direct impaction by the ulnar styloid and a direct blow to the dorsum of the wrist are common mechanisms of injury. Patients typically present with ulnar-sided wrist pain and decreased range of motion and grip strength secondary to pain. The lunotriquetral shear test may elicit pain, though this is not necessarily specific for a triquetral fracture alone, as a tear in the lunotriquetral ligament may also elicit pain.
Trapezium fractures
These fractures are usually associated with other carpal bone fractures, as well as fractures of the first metacarpal and the radius. Dislocation in isolation is very rare.
Symptoms may include the presence of localized tenderness and swelling following the injury. Fractures of the wrist are tender immediately distal to the tuberosity of the scaphoid. The tenderness of the body fracture of the trapezium is more easily elicited anterior or dorsal to the tendon of the abductor pollicis longus, about 1cm distal to the tip of the radial styloid. Range of motion in the wrist may be pain free, but pinch strength specifically is weak and painful. Fractures of the trapezial ridge may be associated with symptoms of carpal tunnel syndrome secondary to median nerve compression.
Trapezoid fractures
This type of fracture is rare, as the trapezoid is well-protected by strong ligament attachment with the trapezium, capitate, and index metacarpal and also by the bony geometry of the carpometacarpal articulation.
Trapezoid fractures are usually associated with trapezoid and index metacarpal dislocations, as in axial pattern fracture dislocation. Palmar dislocation is also possible.
Capitate fractures
Isolated capitate fractures are often undisplaced, but most of the fractures can be found in combination with other major carpal bones, especially the scaphoid (scaphocapitate syndrome). Diagnosis depends on a degree of suspicion, which should be present when evaluating a scaphoid fracture.
Hamate fractures
Fracture of the body or the hook of the hamate can present similarly.
Usually, the patient experiences pain on the ulnar half of the wrist and localized swelling and tenderness over the dorsal ulnar projection of the body of the hamate. These injuries should be suspected for ulnar wrist pain in golf, tennis, baseball, and squash players. Patients may also complain of symptoms of ulnar nerve compression (Guyon canal), including weakness and decreased subjective sensation to the ulnar-innervated digits.
Pisiform fractures
This type of fracture is very uncommon. About half of pisiform fractures occur in association with other upper extremity injuries that can delay the diagnosis of pisiform fractures. They are most commonly caused by a direct blow to the hypothenar eminence.
Perilunate dislocation
Patients have generally diffuse tenderness with significant loss of motion and pain. Initial mild swelling increases significantly over time. The patient can have good active wrist extension, but flexion is usually limited. Crepitation also can be present.
Palpation reveals disruption of the normal bony contour. In a person with a dorsal perilunate injury, the capitate can be identified as dorsal swelling. Volar perilunate dislocation can manifest with median neuropathy.
Perilunate fracture dislocation
Compared to other injuries, patients present with more severe pain that is incapacitating. The wrist is swollen, and patients cannot flex their fingers. The pathognomonic feature is dorsal and palmar pain upon palpation, not isolated to a single area. Again, median nerve compression is common and, therefore, requires a careful neurologic examination.
Axial dislocation and fracture dislocation
The manifestations of injuries can range from open laceration and denudement to closed injury. Patients have extreme pain, swelling, and tenderness in the wrist. Combined injury and dislocation of the metacarpals and phalanges is common. Serious neurovascular compromise and a variety of ligamentous and tendon disruptions may be evident upon careful examination.
Isolated carpal fractures
Isolated carpal fractures also manifest as wrist pain and tenderness. Bruising may be evident over the trapezium, scaphoid, and hamate hook in the palm.
Tenderness to palpation and swelling over the ulnar wrist suggest triquetral or pisiform fracture, which is more volar with pisiform fractures and dorsal with triquetral fractures. Also, pain with forceful wrist flexion suggests triquetral fracture.
Dull aching over the hypothenar eminence and ulnar nerve palsy suggest hamate fracture (see image below). The hamulus is usually tender. Progressive grip weakness, pain with flexion, and lateral movement of the little finger also can be present, especially with nonunion at the injury site.
Isolated carpal dislocations
Isolated dislocations manifest similar to the other injuries, and symptoms are localized to the area of dislocation. Palpation may reveal a bony mass.
Indications
Scaphoid fractures
Type A and other stable, nondisplaced fractures can be treated using closed methods. Short arm casting is usually sufficient, with 95% union in 11 weeks. All higher-grade and other unstable fractures are treated with open reduction and internal fixation (ORIF).
Generally, operative indications include a radiolunate angle greater than 15°, a scapholunate angle greater than 60°, or a greater than 1-mm displacement of the scaphoid. All proximal pole fractures should be treated by ORIF due to the predictably high rates of nonunion. Avascular necrosis of the proximal scaphoid should be treated with ORIF, usually with a vascularized bone graft (see image below).
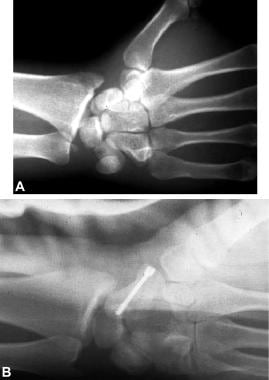 A is a lateral radiograph typical of transscaphoid perilunate fracture dislocation of the wrist. B is a postoperative lateral radiograph of the injury following Herbert screw fixation.
A is a lateral radiograph typical of transscaphoid perilunate fracture dislocation of the wrist. B is a postoperative lateral radiograph of the injury following Herbert screw fixation.
Lunate - Acute lunate fracture
Early diagnosis of lunate fractures is an uncommon occurrence. If discovered, immobilization is usually sufficient for healing. Displaced fractures (>1 mm) and transverse fractures require ORIF to optimize bony union.
Kienbock disease
With stage I, immobilization in a short cast for up to 3 months may be sufficient. This may provide an opportunity for the lunate to revascularize. If no improvement is observed in 3 months, radial shortening for ulnar-minus variance is recommended. This operation significantly reduces the axial load on the lunate (redistributing it to the radioscaphoid and ulnocarpal joints) and allows for spontaneous or indirect revascularization. Otherwise, neutral or the ulnar-plus variety should be directly revascularized with a vascular bone graft, usually the 4,5 extensor compartment artery (ECA). This corticocancellous graft taken from the distal radius at the base of the fourth compartment perfuses based on the retrograde flow from the intercarpal arch.
For stage II and IIIA, treatment is similar to stage I disease. In addition to revascularization, stage II/IIIA ulnar-plus/neutral fractures may benefit from capitate shortening or radial wedge osteotomy.
For stage IIIB, scaphocapitate fusion or other limited fusions (ie, triscaphe or STT fusion) may maintain some degree of functional wrist mobility. Necrotic or fragmented lunate should be excised.
For stage IV, salvage procedures are necessary, either proximal row carpectomy or total wrist fusion. Patients whose goal is simply pain relief and return to heavy manual labor may benefit most from a total wrist fusion.
Perilunate dislocation
Dorsal perilunate and palmar lunate dislocations are different manifestations of the same injury, and treatment remains essentially the same.
Closed reduction and casting is rarely satisfactory and is not currently recommended as definitive treatment. Initial closed reduction has the benefit of immediate restoration of anatomy and alleviating pressures on the median nerve in the carpal tunnel. In this case, postreduction radiographs are essential and only perfect alignment is acceptable. A scapholunate angle greater than 60° or a scapholunate gap greater than 4 mm indicates significant residual scaphoid subluxation. Any malalignment or instability compromises the outcome and mandates ORIF. However, most surgeons now prefer initial operative management and direct ligament repair as the standard of care.
Perilunate fracture dislocation
Perilunate fracture dislocation is an indication for operative intervention. Closed reduction and percutaneous fixation is still performed, but this is generally considered to have a poor outcome and is currently not recommended. Direct primary repair of the extrinsic and intrinsic ligaments of the wrist needs to be performed. The potential for median nerve compromise also warrants operative intervention.
Isolated carpal fractures (not including the scaphoid)
Triquetral fractures usually heal well with simple cast or splint immobilization for 3-6 weeks. Nonunion is extremely rare.
Pisiform fractures also heal well with splinting for similar periods. Complications are rare.
Regarding the hamate, any intra-articular fracture with displacement at the capitohamate, triquetrohamate, or hamatometacarpal joints greater than 1 mm requires ORIF. This may be performed through a dorsal approach and the hamate secured with either screw fixation (headless compression) or with percutaneous K-wires. Stable nondisplaced fractures typically heal with cast immobilization.
Fractures at the base of the hamate hook usually heal well if diagnosed and treated within 2 weeks of the injury. These are usually best treated with cast immobilization. The more distal fracture (more volar in location) tends not to heal as well. Any fracture of the base that is older than 14-21 days, failed conservative treatment, or is a more distal acute fractures of the hook should be treated by direct hamate hook excision. This has been shown to provide adequate pain relief and adequate predictable functional outcomes (see image below).
For the trapezium and trapezoid, fractures greater than 1 mm displacement at the carpometacarpal or scaphotrapeziotrapezoidal joint require ORIF. Otherwise, thumb spica cast/splinting is adequate.
With capitate fractures, undisplaced injury to the body may be treated with cast immobilization. Intra-articular fractures of the proximal pole require ORIF for optimal outcome.
Isolated carpal dislocations
For scaphoid dislocation, closed reduction or open reduction with associated ligament repair has been advocated. The latter method is preferred because direct ligament attachment and, therefore, subsequent anatomic healing may be achieved. Kirschner wire (K-wire) fixation is usually needed in either case.
Triquetral dislocations do well with closed reduction or open reduction. Any displacement larger than 1 mm requires ORIF. Consideration of an open procedure should be given to volar avulsion fractures, as rupture of the lunotriquetral ligament may be an associated finding.
Pisiform dislocations require only simple excision.
For trapezoidal and trapezium dislocations, closed reduction with percutaneous pin placement can be attempted; however, more accurate reduction may be achieved with an open reduction and direct fixation or percutaneous K-wire fixation.
Hamate fracture/dislocations have been successfully treated with closed and open reduction techniques with mixed success. Simple excision has also been described; however, this may leave the patient with residual pain. A limited intracarpal arthrodesis would likely lead to a more predictable functional outcome.
Axial dislocation and fracture dislocation
Treatment of axial dislocations requires immediate recognition and reduction to ensure proper healing.
Examination for soft tissue and neurovascular injury is critical. After adequate anesthesia, intravenous antibiotics, and debridement of frankly necrotic tissue, closed reduction can be attempted and pin fixation performed. Failure to reduce, poor reduction alignment, or tendinous/neurovascular injury require operative reduction and fixation.
Relevant Anatomy
Bone anatomy
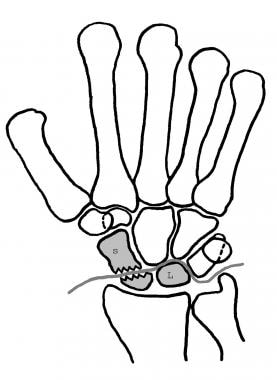
The wrist is composed of 8 bones, including the scaphoid, lunate, triquetrum, pisiform, hamate, capitate, trapezoid, and trapezium (see image below).
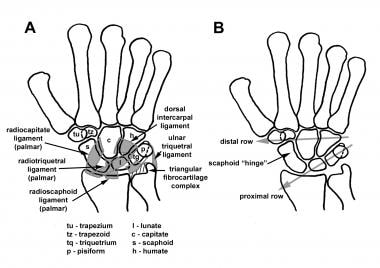 A is the anatomy of the carpus and palmar ligaments. B is illustrating the proximal and distal rows, with the scaphoid hinge binding the movement between rows.
A is the anatomy of the carpus and palmar ligaments. B is illustrating the proximal and distal rows, with the scaphoid hinge binding the movement between rows.
The largest bone of the proximal row is the scaphoid, which serves as a stabilizing link between the proximal and distal carpal rows. Its name is derived from the Greek word skaphos, which means boat, because of the resemblance in shape. Almost the entire surface of the scaphoid articulates with surrounding bones and is, therefore, covered almost entirely with cartilage. The distal convex surface articulates with the trapezoid and trapezium.
The medial surface has 2 facets. The larger, more distal medial facet is concave and articulates with the capitate. The more proximal medial facet is also concave and articulates with the lateral lunate surface. The lateral scaphoid surface is large, convex, and articulates the radius at the scaphoid fossa. The scaphoid tubercle is the only nonarticulating surface and is found distally on the palmar aspect of the scaphoid. This prominence serves as a pivot point for the flexor carpi radialis tendon and as an attachment point for the radioscaphocapitate and the scaphotrapeziotrapezoid ligaments.
The lunate sits like a cup, holding the capitate (and a small component of the radial and proximal hamate) in its distal biconcave surface. The proximal surface is convex and articulates primarily with the radius and with the triangular fibrocartilage complex (TFCC) more medially. The lateral (radial) surface of the lunate articulates with the scaphoid, while the medial (ulnar) surface articulates with the triquetrum. The hornlike palmar and dorsal nonarticulating surfaces serve as ligamentous attachment points and function to stabilize the head of the capitate in place. Viegas classified lunates into 2 types based on their distal articulation. Type 1 lunates articulate with the capitate distally, while type 2 lunates articulate with the capitate and with the hamate by way of a small distal ulnar/medial facet. This may have some clinical significance in terms of midcarpal stability patterns.
The triquetrum also has 4 articulating surfaces. The distal surface has a radial convex and an ulnar concave formation, which both articulate with the hamate. The lateral (radial) surface articulates with the lunate and proximally serves as the insertion site for the lunotriquetral interosseous ligament and the vascular penetration into the triquetrum. The small convex proximal surface articulates with the TFCC. The palmar aspect of the triquetrum contains an oval-shaped surface that articulates with the pisiform through cartilaginous structures. The dorsal triquetrum has a transverse ridge and is the attachment point to the highly relevant dorsal radiotriquetral, dorsal lunotriquetral, and dorsal intercarpal ligaments.
The pisiform is a sesamoid type bone that solely articulates with the triquetrum on its small, flat, oval, dorsal articular surface. The remaining surface is round and rough and is the site of attachment for the flexor carpi ulnaris tendon. Ligamentous connections at this site attach the pisiform to the hook of hamate and the base of the fourth and fifth metacarpals.
The trapezium has 4 articulating surfaces. The distal saddle-shaped surface articulates with the first metacarpal, while the more ulnar (medial) distal surface articulates with the base of the second metacarpal. Medially, the trapezium articulates with the trapezoid and, proximally, with the distal scaphoid.
The trapezoid is trapezoidal. Distally, the wedge-shaped facet articulates with the second metacarpal. In some cases, an additional facet may articulate with the third metacarpal. The radial surface articulates with the trapezium, the ulnar surface articulates with the capitate, and the proximal concave surface articulates with the distal scaphoid. The palmar and dorsal aspects receive ligamentous attachments.
The capitate is the largest and most prominent bone in the wrist. The proximal head articulates with the scaphoid radially, the hamate ulnarly, and the lunate proximally. The distal body articulates with the trapezoid laterally through cartilage and articulates medially with the hamate through an interosseous ligament. The distal capitate articulates with the styloid process of the third metacarpal, the entire base of the third metacarpal, and, often, the proximal medial facet of the fourth metacarpal.
The hamate articulates distally with the fourth and fifth metacarpal bases. The oblique medial surface articulates with the triquetrum, while the lateral surface articulates with the capitate. The palmar nonarticulating projection is known as the hamulus and is the site of attachment of the flexor retinaculum, pisohamatum ligament, and the muscular origin of opponens digiti minimi.
Ligament anatomy
Several ligamentous complexes exist in the wrist. They can be classified as follows:
Extrinsic carpal ligaments are divided into superficial extrinsic radial carpal ligaments, deep extrinsic radial carpal ligaments, and deep extrinsic ulnar carpal ligaments.
Superficial extrinsic radial carpal ligaments are as follows:
-
Radioscaphoid (palmar)
-
Radiocapitate (palmar)
-
Long radiolunate (palmar)
-
Radiotriquetral (dorsal)
Deep extrinsic radial carpal ligaments are as follows:
-
Short radiolunate
-
Radioscapholunate
Deep extrinsic ulnar carpal ligaments are as follows:
-
Ulnotriquetral
-
Ulnolunate
-
Ulnocapitate
Intrinsic carpal ligaments include the following:
-
Scapholunate interosseous ligament
-
Lunotriquetral interosseous ligament
-
Distal carpal row interosseous ligament
-
Dorsal intercarpal ligaments
-
Palmar intercarpal ligaments
The palmar ulnocarpal ligaments comprise the other group of capsular ligaments that cross the carpus in a palmar direction. This includes the ulnolunate, ulnotriquetral, and ulnocapitate ligaments. Collectively, they originate from the palmar radioulnar ligament, which contributes to the formation of the triangular fibrocartilage complex (TFCC).
Dorsally, the capsule of the wrist is primarily composed of the dorsal intercarpal and dorsal radiocarpal ligaments. The dorsal radiocarpal ligament connects the radius, lunate, and triquetrum. The dorsal intercarpal ligament connects the triquetrum to the scaphoid and trapezoid. These structures can be dissected together to provide a radial flap when access to the dorsal carpus is required. This technique, commonly referred to as a capsular-sparing capsulotomy, allows excellent exposure and may result in reduced postoperative scarring and stiffness. [7]
The palmar midcarpal ligaments are the main stabilizing ligaments of the carpus and appear as a continuous flat sheet of ligament, which converges at the capitate. Its most important components include the scaphotrapezium, trapezoid, scaphocapitate, triquetrocapitate, triquetrohamate, and pisohamate ligaments.
The short ligaments between the bones are known as interosseous ligaments. The interosseous ligaments in the proximal row include the scapholunate, lunotriquetral, and pisotriquetral ligaments. The ligaments in the distal row include the trapeziotrapezoid interosseous ligament, trapeziocapitate interosseous ligament, and capitohamate interosseous ligament.
The palmar radioulnar ligament and dorsal radioulnar ligament (which sends fibers to the flexor carpi ulnaris subsheath) contribute to the formation of the triangular fibrocartilage complex. This articular disk is interposed between the ulnar head and carpal bones, and its thickness is inversely proportional to positive ulnar variance. See Kienböck disease in the Pathophysiology section.
Blood supply
The carpal wrist receives vascularization primarily from the dorsal and palmar carpal plexi (see image below). The radial artery, ulnar artery, and posterior branch of the anterior interosseous artery contribute branches that form the dorsal radiocarpal arch and the dorsal intercarpal arch. The dorsal radiocarpal arch is positioned over the radiocarpal joint and supplies the proximal carpal row, whereas the intercarpal is more distal and supplies the distal carpal arch.
In the palmar aspect, the radial, ulnar and the anterior branch of the anterior interosseous artery contribute to the formation of palmar radiocarpal and palmar intercarpal arches. In addition, the deep palmar arch supplies the distal carpal row through the recurrent ulnar and recurrent radial branches.
Vascularization at risk (tenuous carpal vascular supply)
The scaphoid is exclusively supplied by the radial artery, which sends a dorsal, proximal, and distal branch to the distal third of the scaphoid (see image below). The distal and proximal branches come off the superficial palmar branch of the radial artery (20-30% of scaphoid blood supply), and the distal branch comes off the dorsal radiocarpal branch of the radial artery (70-80% of scaphoid blood supply). These vessels flow retrograde through an interosseous artery to supply the proximal pole of the scaphoid. For this reason, fractures of the scaphoid waist lead to a severed blood supply and a high incidence of avascular necrosis of the proximal pole.
The lunate receives blood dorsally and volarly. Dorsally, the radial artery contributes small vessels with origination from the intercarpal arch. In the palmar direction, the lunate receives branches from (1) the anterior division of the anterior interosseous artery, (2) the palmar carpal branches of the radial and ulnar arteries, and (3) a recurrent branch from the deep palmar arch. In some instances, the lunate receives vascularization only from the dorsal components and thus is susceptible to avascular necrosis after lunate fracture. Gelberman et al found that 20-30% of lunates have a single nutrient vessel that enters the lunate either volarly or dorsally, while the remaining 70-80% have multiple nutrient arteries, shaped in the form of X or Y, that enter the lunate either volarly or dorsally. [8] See Kienböck disease in the Pathophysiology section.
The capitate receives blood from branches of the dorsal radiocarpal and intercarpal arches and dorsal branch of the anterior interosseous artery. On the palmar aspect, branches are from the palmar radiocarpal arch and deep palmar arch and a direct contribution from the recurrent ulnar artery. The blood vessels combine to form a plexus distally and supply the head of the capitate through retrograde interosseous vessels. Thus, the proximal capital may also be vulnerable to avascular necrosis.
Innervation
The wrist and carpal capsules are innervated by branches of the posterior and anterior interosseous nerves; superficial branch of the radial nerve; dorsal, lateral, and perforating branches of the ulnar nerve; palmar cutaneous of the median nerve; and the medial and lateral antebrachial cutaneous nerves of the forearm. These nerves play a significant role in the pathophysiology of chronic wrist pain and, therefore, also in the management of nerve-specific denervation techniques.
Contraindications
At this time, there are no known absolute contraindications to the initiation of treatment for most wrist fractures and dislocations.
-
A is the anatomy of the carpus and palmar ligaments. B is illustrating the proximal and distal rows, with the scaphoid hinge binding the movement between rows.
-
Diagrammatic representation of the common transscaphoid perilunate fracture dislocation of the wrist.
-
Lateral radiograph of the wrist illustrating volar dislocation of the lunate.
-
A is the greater-arc or transscaphoid perilunate dislocation pattern. B is the lesser-arc or perilunate dislocation pattern.
-
A is ulnar axial dislocation (fracture pattern also possible). B is radial axial dislocation (fracture pattern also possible).
-
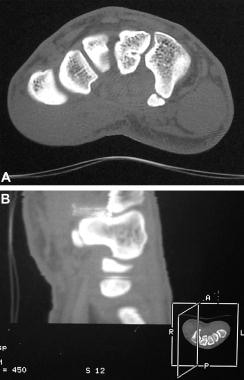
CT scan of the hamate demonstrating a nonunited fracture of the hamulus.
-
Diagrammatic representation of the intraosseous blood supply of the scaphoid.
-
Bone scan of the wrist illustrating increased uptake in the left wrist after Herbert screw fixation of a transscaphoid perilunate fracture dislocation of the wrist 3 months postoperatively.
-
A is a lateral radiograph typical of transscaphoid perilunate fracture dislocation of the wrist. B is a postoperative lateral radiograph of the injury following Herbert screw fixation.
Tables
What would you like to print?
- Overview
- Workup
- Treatment
- Medical Therapy
- Surgical Therapy
- Distal and Waist Fractures
- Proximal Pole Fractures
- Lunate Immobilization
- Operative Acute Lunate Fracture
- Kienbock Procedures
- Triscaphe (Scaphotrapeziotrapezoid Joint/STT) Arthrodesis
- Perilunate Dislocation (Lesser Arc) - Closed Reduction and Immobilization
- Perilunate Dislocation - Operative Procedure (ORIF)
- Perilunate Fracture Dislocation (Greater Arc)
- Perilunate Fracture Dislocation - Operative Procedure (ORIF)
- Isolated Carpal Fractures
- Management of Isolated Carpal Dislocations
- Axial Dislocation and Fracture Dislocation
- Complications
- Outcome and Prognosis
- Future and Controversies
- Show All
- Media Gallery
- References