Overview
Entrapment neuropathies of the upper extremity are common problems. A wide range of physicians, from primary care providers to specialists such as orthopedic surgeons, plastic surgeons, or neurosurgeons, are sought to care for these problems.
What has traditionally been attributed to features of normal aging (eg, weakness, loss of function or sensation) has been subsequently recognized in younger patients whose vocations require repetitive motion to complete work-related tasks. Repetitive motion, force, posture, and vibratory influences on the peripheral nerves of the upper extremity are poorly understood but are blamed as contributing factors to the development of neuropathic symptoms. [1]
Currently, patterns of symptomatology, objective measures of nerve function (eg, electromyelogram [EMG] evaluation, nerve conduction studies), and the anatomy associated with nerve compression have been well outlined. [2] Despite attempts at conservative medical and functional management, surgical decompression has become the choice for definitive treatment. [3]
Anatomy
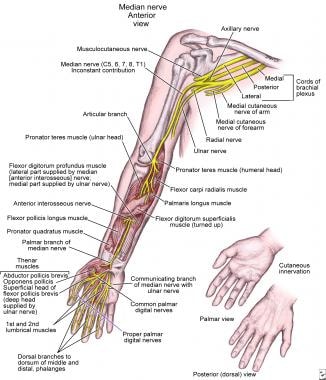
See the image below.
The median nerve
The main nerve entrapments in the upper extremity involve the median nerve, ulnar nerve, or radial nerve. The median nerve forms the junction of the lateral medial cords. It travels lateral to the brachial artery to approximately the mid humerus or junction of the proximal two thirds to distal one third of the humerus. At this level, the median nerve crosses over the brachial artery to lie in a more medial anatomic position.
The nerve is superficial to the brachialis muscle and usually lies in a groove with the brachial artery, between the brachialis and biceps muscle. It travels across the antecubital fossa, underneath the bicipital aponeurosis, and between the biceps tendon and the pronator teres. At this level, the median nerve is on the distal aspect of the brachialis muscle. The nerve then travels underneath the 2 heads of the flexor digitorum sublimis (FDS) muscle to lie between this muscle and the flexor digitorum profundus (FDP) muscle. The median nerve emerges between these 2 muscles in the distal forearm to then travel ulnar to the flexor carpi radialis and radial to the sublimis tendons, usually directly underneath the palmaris longus tendon, and enters the carpal tunnel in a more superficial plane to the flexor tendons.
The motor branch emerges at variable sites but most frequently at the distal aspect of the carpal ligament to service the thenar musculature. Just beyond the end of the carpal ligament, the median nerve trifurcates to become the common digital sensory nerves to the fingers. The palmar cutaneous branch of the median nerve is a sensory branch that comes from the main body of the nerve approximately 6 inches above the rest of the nerves and services an elliptical area at the base of the thenar eminence. This superficial nerve does not lie within the carpal tunnel.
Just distal to the antecubital fossa, the median nerve branches into the anterior interosseous nerve, which travels on the interosseous membrane and innervates the flexor pollicis longus (FPL), the FDP to the radial 2 digits, and the pronator quadratus at its termination. The nerve innervates the pronator teres, flexor capri radialis, the FDS, and the 2 radial FDP tendons. It also supplies the FPL and the pronator quadratus.
Within the hand, the motor branch of the median nerve supplies the opponens pollicis, the flexor pollicis brevis, and the abductor pollicis brevis musculature. It also supplies the 2 radial lumbrical muscles in the hand. The median nerve supplies sensation to the 3.5 digits on the radial aspect.
The ulnar nerve
The ulnar nerve arises from the medial cord of the brachial plexus. The ulnar nerve travels posterior to the brachial artery and remains within the flexor compartment of the upper extremity until it reaches the medial epicondyle. The nerve travels behind the medial epicondyle back into the flexor compartment underneath the flexor musculature. Above the elbow, the ulnar nerve lies on the long head and then the medial head of the triceps muscle, directly posterior to the medial intermuscular septum between the brachialis and the triceps muscles.
The fascial bands over the median nerve constitute the Struthers arcade. The nerve passes within the cubital tunnel posterior to the medial epicondyle. It is directly underneath a tight fascial roof known as the Osborne band, which is contiguous with the leading fascial heads of the flexor carpi ulnaris (FCU) muscle. Just above the elbow branches, the nerve branches to the superficial head of the FCU. The nerve lies directly over the top of the FDS muscle and beside the FDP muscle at the elbow.
As the ulnar nerve travels down the forearm, it is wedged between the FDS and the FDP muscle bellies to exit in the distal forearm just ulnar to the ulnar artery and the FDP tendons. The FCU tendon protects the nerve on its ulnar aspect. The ulnar nerve travels within the Guyon canal at the wrist to supply the hypothenar muscles, including the opponens digiti quinti and the abductor digiti quinti. It also supplies the 2 ulnar lumbrical muscles and the interossei to the hand and the deep branch to the flexor pollicis brevis muscle. The ulnar nerve supplies sensation to the 1.5 digits of the ulnar aspect. The dorsal cutaneous branch of the ulnar nerve supplies sensation to the dorsal ulnar half of the hand and fingers. This nerve arises from the main ulnar nerve approximately 6 cm proximal to the wrist.
The radial nerve
The radial nerve emerges from the posterior aspect of the humerus in the spiral groove between the brachialis and brachioradialis muscles above the elbow. It leaves the extensor compartment to travel in front of the elbow underneath the brachioradialis muscle, sending branches of innervation to it just above the elbow. The radial nerve divides at the level of the radial capitellar joint into the deep motor branch of the radial nerve (ultimately becoming the posterior interosseous nerve) and the superficial radial nerve. At this point, it branches to the extensor carpi radialis brevis.
The superficial radial nerve continues to travel underneath the brachioradialis muscle to ultimately emerge between that muscle and the extensor carpi radialis longus tendon. The superficial radial nerve supplies sensation to the radial half of the dorsum of the hand. The deep motor branch of the radial nerve travels within the fat pad and runs below the supinator muscle to emerge the supinator and become the posterior interosseous nerve in the distal dorsal aspect of the forearm. The posterior interosseous nerve travels at the level of the interosseous membrane to ultimately provide sensation to the posterior aspect of the wrist. This nerve innervates the extensor indicis proprius, extensor digiti quinti, extensor carpi ulnaris, abductor pollicis longus, extensor pollicis brevis, and extensor digitorum communis muscles.
Pathophysiology
The phrase compressive neuropathy implies that the peripheral nerves are being impinged upon by adjacent anatomic structures. The resultant injury is assumed to be related to reduced epineural blood flow. The relative ischemia decreases axonal transport and, in turn, the nerve's ability to conduct impulses. Long-standing disease can produce irreversible damage, in the form of scarring or fibrosis, and loss of motor endplates, causing muscle atrophy. The double-crush theory predicts that a compressive lesion at one point along a peripheral nerve lowers the threshold for occurrence of compression at another site secondary to internal derangement of nerve cell metabolism. Examples of some pathogenic factors inciting neural compression are as follows:
-
Vascular - Diabetes, microcirculatory disease
-
Inflammatory - Synovitis, rheumatoid arthritis
-
Trauma - Supracondylar humerus fracture, lunate dislocation
-
Anatomical - Anomalous muscles, vascular plexus, fascial bands
-
Metabolic - Pregnancy, hypothyroidism
-
Iatrogenic - Injections, hematomas
-
Neoplastic - Ganglion, lipoma, sarcoma
Diagnosis
Many of the findings of peripheral nerve irritation or entrapment are identified during the physical examination and are discussed here in relation to each of the individual syndromes. Reproducing symptoms via provocative maneuvers or diagnosing deficits in strength or sensation can be accomplished in the office or with the aid of hand therapists.
Two-point discrimination testing, Semmes-Weinstein monofilament testing, and grip strength measurements are simple and inexpensive means of evaluation. Findings from imaging studies (eg, plain radiographs, MRIs) are occasionally helpful for excluding cervical ribs, lung tumors, or extremity masses, which may be contributing to neural compression.
Electrodiagnostic studies (eg, EMG, nerve conduction studies) remain the criterion standard for objective evaluations of neuropathic conditions. These studies are not without flaws; they are highly operator-dependent and the results do not always correlate with the severity of symptoms or patient outcomes. Despite these drawbacks, they may help confirm equivocal physical examination findings or help isolate the specific site of compression preoperatively. EMGs also may be used to verify progression or resolution in neurophysiology following surgical release.
Common Compressive Neuropathies
Median nerve
See the list below:
-
Pronator syndrome
-
Anterior interosseous syndrome
Ulnar nerve
See the list below:
Radial nerve
See the list below:
-
Posterior interosseous syndrome [7]
-
Superficial radial nerve syndrome
Median Nerve Entrapment Syndromes
Pronator syndrome
Sites of compression
These include the lacertus fibrosus (bicipital aponeurosis, superficial forearm fascia), the Struthers ligament (thickened or aberrant origin of pronator teres from distal humerus), the pronator teres (musculofascial band or compression between 2 muscular heads), and the FDS proximal arch or the flexor digitorum superficialis.
Signs and symptoms
These include pain in the volar forearm that is exacerbated with activity and relieved by rest; decreased sensation in the thumb, index finger, long finger, and radial side of the ring finger; weakness of thenar muscles; and a positive Tinel or Phalen sign in the proximal forearm.
Treatment
Nonsurgical or conservative treatment includes rest and anti-inflammatory medications. Surgical treatment includes exploration of the median nerve in the proximal forearm, an incision distal and more or less proximal to the antecubital fossa in a zigzag fashion across the joint, and the release of all sites of possible compression.
Anterior interosseous syndrome
Nerve anatomy
The anatomy includes the branch of the median nerve arising approximately 6 cm below the elbow and supplying motor function from the FPL, pronator quadratus, and FDP to the index finger.
Etiology
Causative factors include tendinous bands, a deep head of the pronator teres, accessory muscles (including the Gantzer muscle, which is the accessory head of the FPL), aberrant radial artery branches, and fractures.
Symptoms
These include vague pain in the proximal forearm and weakness of the FPL and FDP to the index finger. Affected persons cannot form a circle by pinching their thumb and index finger (ie, hyperextension of index distal interphalangeal joint and thumb interphalangeal joint). Sensory involvement is not described.
Treatment
Nonsurgical treatment includes rest, anti-inflammatory medications, and splints. Surgical treatment includes exploration of the median nerve through an approach similar to that for pronator syndrome, release of the lacertus fibrosus and division superficially more or less to the deep heads of the pronator teres, and ligation of crossing vessels.
Carpal tunnel syndrome
Anatomy
The carpal tunnel is formed by carpal bones (floor), the transverse carpal ligament (roof), the scaphoid and trapezium (radial aspect), and the pisiform and hook of the hamate (ulnar aspect). The tunnel contains 4 FDS muscles, 4 FDP muscles, the FPL, and the median nerve.
Etiology
Causative factors may include accessory muscles (manus)/lumbricals, tenosynovitis, rheumatoid arthritis, type 1 diabetes mellitus, pregnancy, a ganglion, foreign or loose bodies, repetitive motion, carpal fractures or dislocations, or a persistent median artery.
Symptoms
These include decreased sensation, paresthesias, and tingling in the distribution of the median nerve; worsened symptoms with repetitive use; night awakening with tingling or numbness; radiation of pain up the forearm; a positive Tinel or Phalen sign or compression at the wrist; and possible thenar muscle wasting with advanced cases.
Studies
EMG or a nerve conduction velocity study can be used in difficult cases or with polyneuropathy. [8] Occasionally, radiographs help rule out occult fractures, a foreign body, or tumors. Laboratory studies may include an erythrocyte sedimentation rate, blood glucose value, thyroid evaluation, and rheumatoid factor.
A study by Han et al indicated that the risk for the future development of idiopathic carpal tunnel syndrome is increased when, on radiography, the lunate shows excessive dorsiflexion or demonstrates volar displacement compared with the radial shaft. [9]
Treatment
Nonsurgical measures include wrist splinting in a neutral position to minimize intratunnel pressures at night due to posture; anti-inflammatory medications; steroid injections for transient relief; and an alteration of work station arrangement or the amount of repetitious motion, with breaks or a total change in work activities. [10, 11, 12] Surgical therapy is indicated in refractory cases or those not responsive to nonsurgical measures. [10] All surgical techniques focus on release of the volar transverse carpal ligament. [10] Different incisions are used for an open approach or, more recently, endoscopic release; both (ie, endoscopic and open) have advantages and disadvantages. The main goal is complete release of the ligament without injury to the palmar cutaneous, thenar, and main branch of the median nerve.
Clinical practice guidelines on the diagnosis and treatment of carpal tunnel syndrome were released in 2016 by the American Academy of Orthopaedic Surgeons. [13]
Risks
These may include bleeding, infection, and a tender scar; injury to nerves, palmar arch vessels, or tendons; failure to completely release the ligament; and recurrence.
Recovery
Some advocate short-term (3-5 d) wrist immobilization. Others advocate immediate movement to prevent scar formation. Sutures are removed in 2 weeks. [10]
Ulnar Nerve Entrapment Syndromes
Cubital tunnel syndrome
Anatomy
The ulnar nerve runs adjacent to the medial head of the triceps into the groove behind the medial epicondyle of the humerus. It passes beneath the fascia joining the 2 heads of the FCU and lies on the superficial surface of the FDP.
A retrospective study by Wilson et al indicated that the presence of an anconeus epitrochlearis muscle may discourage the development of cubital tunnel syndrome, finding that 5.4% of patients in the study with cubital tunnel syndrome had the muscle, while 15.5% of asymptomatic controls had the anconeus epitrochlearis. The investigators suggested that the muscle protects against the syndrome by reducing the rigidity of the cubital tunnel entrance. [14]
Sites of compression
These include the Struthers arcade, the anconeus epitrochlearis, the intermuscular septum, the Osborne band, and the aponeurosis of the FCU.
Signs and symptoms
These include pain in the forearm, which radiates in the distribution of the ulnar nerve; numbness; tingling in the 1.5 fingers of the ulnar aspect; wasting or weakness of intrinsic hand muscles; a positive compression test result at the elbow; recurrent subluxation of the nerve over the epicondyle; and the reproduction of symptoms with elbow flexion, with or without wrist extension. One study of patients with cubital tunnel syndrome sought to determine the association between the elbow flexion test and the degree of extraneural pressure in the cubital tunnel. Results of the study suggest that the reproduction of cubital tunnel syndrome symptoms via the elbow flexion test could not be explained simply by dynamic pressure in the cubital tunnel. [15]
Treatment
Nonsurgical measures include nighttime pillow splints to keep the elbow extended. [16] Rest and anti-inflammatory medications are also useful. Surgical methods focus on releasing the nerve along its course at sites of compression, preventing subluxation over the medial epicondyle, and preventing traction or tension on the nerve with elbow motion. Most commonly, decompression, medial epicondylectomy, anterior transposition (subcutaneous vs submuscular), or a combination of these is used. [5, 17]
A retrospective study by Gaspar et al indicated that in patients with cubital tunnel syndrome who undergo medial epicondylectomy, risk factors for revision surgery include younger age, less severe disease, preoperative use of opioids, and the submission of associated claims for workers’ compensation. [18]
Advantages and disadvantages of surgical options
Simple decompression may fail to prevent subluxation or traction on the nerve. Epicondylectomy is painful and may make trauma to the nerve more common. Unless subluxation is the cause of symptoms, relief may be incomplete. Transposition of the nerve allows for more slack in the nerve course, but this can cause a kink at the Struthers arcade if improperly released. Subcutaneous placement often results in painful paresthesias with simple local trauma. With more extensive dissection, more vascular supply is interrupted and may cause further injury to the nerve. Placing the nerve in a well-vascularized bed (submuscular transposition) may aid in recovery from or may help prevent recurrent symptoms. Submuscular transposition requires longer immobilization postoperatively to allow flexors to heal, thereby increasing risks of stiffness and reflex sympathetic dystrophy. All surgical approaches can injure the medial brachial and antebrachial cutaneous nerves, causing painful scars and neuromatous pain.
In a study of 375 patients with primary clinical cubital tunnel syndrome who were treated with one of four types of surgery, at mean 92-month follow-up, each surgical technique cured or reduced symptoms in more than 90% of patients who underwent the procedure. Patients in the study were treated with either open or endoscopic in situ decompression or subcutaneous or submuscular anterior transposition. The only long-term complication in the study was a case of scar pain. Of six recurrences of cubital tunnel syndrome that developed by the end of follow-up, one occurred in a patient who had undergone open in situ decompression and five developed in patients who had undergone submuscular anterior transposition. [19]
A study by Nicholson et al of 26 overhead athletes with cubital tunnel syndrome found that at an average 2.7 months following ulnar nerve transposition surgery, 24 patients (92%) had resumed their sporting activity, with 16 of them (62%) having returned to the previous level of play. [20]
A literature review by Buchanan et al indicated that in patients with cubital tunnel syndrome, overall clinical improvement associated with endoscopic tunnel release is comparable to that obtained through open release, as measured using the Bishop and visual analogue scale scores. Rates of new-onset scar tenderness/elbow pain were lower for endoscopic release, although the incidence of postoperative hematomas was higher. The reoperation rate for endoscopic surgery was 4.9%, compared with 4.1% for open release. The investigators cautioned, however, that future research employing a larger patient population and longer follow-up will be needed to draw stronger conclusions regarding endoscopic cubital tunnel release. [21]
Ulnar tunnel syndrome (Guyon canal)
Anatomy
This is the triangular canal at the base of the ulnar side of the palm. It is bordered laterally by the hook of the hamate and the transverse carpal ligament. The medial wall is formed by the pisiform and the attachments of the pisohamate ligament. Both the ulnar nerve and artery traverse the canal to enter the hand. The dorsal cutaneous branch of the ulnar nerve branches before the nerve enters the Guyon canal.
Etiology
Causative factors include repeated blunt trauma from power tools and gripping or hammering with the palm of the hand. Fractures of the hook of the hamate can impinge on the nerve. Other etiologies include tumors such as ganglia or lipomas, anomalous muscle bellies, or hypertrophy of the palmaris brevis. Thrombosis or aneurysm of the artery may compress the nerve.
Symptoms
These may include numbness and tingling, paresthesias and pain in an ulnar distribution of the palm and the 1.5 digits of the ulnar aspect, cold intolerance in the ring and small fingers, normal sensation in the dorsal sensory cutaneous branch of the ulnar nerve, and a positive Tinel or Phalen sign.
Treatment
Nonsurgical treatment includes rest and avoidance of provocative activities. Immobilization with a splint and corticosteroid injections are also effective. Surgical treatment includes surgical decompression of the Guyon canal through the carpal tunnel or through a zigzag wrist crease–traversing incision. Complete exploration should be performed to help exclude a mass or aneurysm that requires repair.
Radial Nerve Entrapment Syndromes
Radial tunnel syndrome
Anatomy
Compression neuropathy of the radial nerve is considered somewhat more rare than the other compression neuropathies of the upper extremity. The radial tunnel proper is somewhat ill defined, but it is usually considered the area where the radial nerve exits between the brachioradialis and the brachialis muscles to where it drives below the proximal edge of the supinator muscle (Frohse arcade) and distal edge of the supinator.
Etiology
The deep branch of the radial nerve can be compressed by 5 structures within the radial tunnel. The most common site of compression is at the proximal fibrous edge of the supinator muscle, known as the arcade of Frohse. The most proximal structure that can compress the deep branch of the radial nerve is the fibrous fascia over the radiocapitellar joint. The next structures that can compress the deep branch of the radial nerve are the radial recurrent artery and the venae comitantes, known as the leash of Henry, although this is uncommon. Lastly, the deep branch of the radial nerve can also be compressed by the distal edge of the supinator muscle, which is known to be fibrous in 50-70% of patients.
Symptoms
These may include pain in the upper extensor forearm; dysesthesia in a superficial radial nerve distribution; and weakening of the extension of the fingers, thumb, or wrist.
Treatment
Surgical treatment includes release of the muscle and superficial slip of the supinator ligation and transection of the vascular leash or release of the fascial bands. The supinator muscle should also be released.
A study by Marchese et al suggested that radial tunnel syndrome can be successfully treated with corticosteroid injection. The report found that in patients with the syndrome who received a single corticosteroid injection in the proximal forearm at the posterior interosseous nerve, the mean quick Disabilities of the Arm, Shoulder and Hand (qDASH) score declined from a baseline 49.4 points to 35.8 points at 12 weeks, and 28.5 points at 52 weeks. In addition, the visual analogue scale score fell from 6.0 points at baseline to 3.4 points at 12 weeks, and 2.9 points at 52 weeks. However, of the 35 patients who completed 1-year of follow-up, eight (23%) did not achieve successful results with injection and were subsequently treated with surgical decompression of the posterior interosseous nerve. [22]
Posterior interosseous syndrome
Etiology
Causes may include entrapment of the nerve within supinator muscle, distal edge of the supinator muscle fracture or dislocation of the radial head, tumors (eg, ganglion, lipoma), and iatrogenic causes resulting from open reduction/internal fixation of proximal radius fractures.
Symptoms
Patients may report proximal forearm pain. No sensory deficit is described, but partial-to-complete motor paralysis of the extensors is reported. [7] Often, the brachioradialis and extensor carpi radialis brevis/extensor carpi radialis longus, which are innervated by more proximal branches, are spared. Therefore, any remaining wrist extension also displays radial deviation.
Treatment
Surgical exploration and decompression through an approach similar to that for radial tunnel syndrome is warranted.
Superficial radial nerve syndrome (Wartenberg syndrome)
Anatomy
The superficial radial nerve exits between the brachioradialis and the extensor carpi radialis longus tendons at the junction of the proximal two thirds to distal one third of the forearm. The superficial radial nerve then courses in a superficial subcutaneous plane to provide sensation to the dorsal aspect of the hand from the thumb to the junction of the ring and long fingers. Sensation to the digits is provided up to the area of approximately the dorsal proximal interphalangeal joint.
Sites of compression
Fascial bands in the subcutaneous plane at its exit site, the tendons of the brachioradialis, and the extensor carpi radialis longus tendons compress the nerve.
Symptoms
Patients report decreased sensation, paresthesia, and tingling in the distribution of the superficial radial nerve. A position Tinel and compression sign is present at the site of exit of the superficial radial nerve. The symptoms are often provoked by extreme pronation of the wrist.
Treatment
Nonsurgical treatment includes wrist splinting in a neutral position and anti-inflammatory medication, which may decrease symptoms in the early stages. Surgical treatment includes surgical resection of part of the brachioradialis tendon to allow for an easy glide motion of the superficial radial nerve at its exit point.
-
Anatomy of median nerve along its course in upper extremity.