Background
Lipoplasty of the lower extremities has become increasingly popular. Although it was once considered a procedure that was fraught with complications and unsatisfactory results, improvements in technique are addressing these concerns. Emphasis on an aesthetic lower extremity has now replaced previous experiences with liposuction, in which legs became thinner but remained tubular and lacked curves. Liposuction can now reduce the bulky look of the calves and result in slimmer, tapering lower legs.
According to the Aesthetic Society, liposuction was the top aesthetic surgical procedure in the United States in 2022, with over 405,000 procedures estimated to have been performed. The second most popular operation was breast augmentation, at over 255,000 estimated procedures. [1]
History of the Procedure
As early as 1964, Schrudde treated the ankle using small incisions strategically placed about the ankle and contoured the area using sharp curettage. Illouz popularized liposuction as opposed to curettage in 1977. He recommended suctioning the deep layer of fat in areas with a defined superficial and deep layer. These areas were typically the outer and inner thighs. In 1982, Teimourian and Fisher reported a case using both sharp curette and suction for the ankle.
Mladick began to suction the upper calf in selected patients in 1983. Further advances in 1985 and 1987 were the introduction of cross-tunneling and the accelerator-tip cannula, respectively. He then reported his first case of circumferential liposuction of the lower legs in 1990. [2]
In 1994, Gasperoni and Salgarello, using small cannulae and incisions, popularized superficial liposuction 1-2 mm below the skin. [3] Over the last several years, Rohrich et al discussed using internal ultrasound-assisted liposuction for the upper one half of the lower leg. [4] Hoppmann et al have recommended liporemodeling as an alternative to silicone implants in reshaping the calf. [5]
Indications
Liposuction of the lower extremity from thigh to ankle is an important adjunct to many plastic surgeons' practice. [6] Having succeeded in reducing particular bulges in the thigh, lower extremity liposuction has now advanced to providing a curvy lower extremity with techniques of circumferential [7] and superficial liposuction.
Patients who are considering this procedure must be examined to see if liposuction of the calves and ankles can adequately address their concerns. Larger lower extremities can be secondary to hypertrophy of muscle tissue, in which case liposuction would be of little benefit.
In selecting a patient for liposuction of the calves and ankles, legs are classified as circumferential or localized heavy legs. In the circumferential type, specific fat distributions are not well-defined and the leg, as a whole, is considered fat. Areas in exception to this are between the perimalleolar regions and over the Achilles tendon distally, rarely having significant fat deposits. In the localized type, the lower calves and ankles tend to have definite bulges over the lower lateral fibular, medial tibial, and ankle regions. Excess fat over the transition between the gastrocnemius muscles and the inferior leg can lead to a tubular-appearing leg.
The pinch test can be used to assess fat deposits. This is performed with patients standing on a stool flat-footed and then standing on their toes. The pinch test can also be carried out with the leg rested horizontally on a chair and the knee bent 90° while the patient stands on the other leg. The minimum pinch test result should be 2 cm in the calves and 1 cm in the ankles.
The ideal patient is in good health, is aged 20-30 years, and has good skin tone. If the patient is older than 50 years and has good skin tone, he or she is a suitable candidate.
Relevant Anatomy
While the motor nerves and most vessels lie deep to the investing fascia, certain structures within the fatty tissue must be taken into consideration when carrying out liposuction of the calves and ankles.
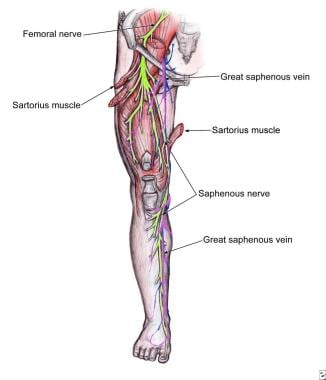
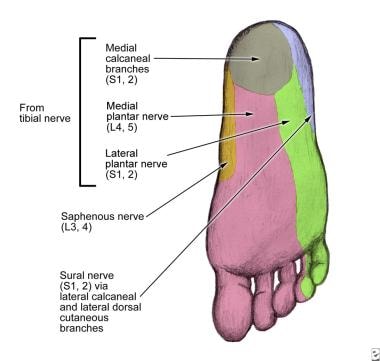
Posterior to the femoral and tibial condyles, the greater saphenous vein descends from behind the knee along the medial leg and then anteriorly to the medial malleolus (see first image below). In the foot, it courses dorsomedially and merges with the medial marginal vein in the sole of the foot through small tributaries (see second image below). The marginal vein courses along the dorsolateral aspect of the foot behind the lateral malleolus and becomes the small saphenous vein as it courses superiorly.
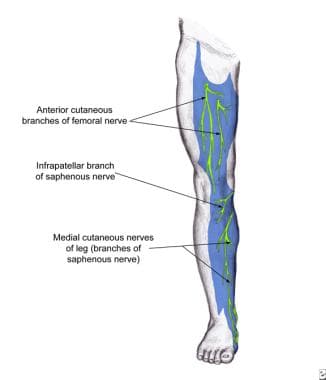
Accompanying the vessels, the saphenous nerve courses along with the greater saphenous vein, and the sural nerve courses with the small saphenous vein at the lower one third of the leg (see image below).
Importantly, stab incisions must not enter the saphenous veins or injure the nerves. Likewise, liposuction should never be performed at the popliteal fossa because of a high risk of injuring the neurovascular structures.
In the thigh, the greater saphenous vein is the only anatomic structure superficial to the fascia that may be injured. The vein is 1.5 in below the inguinal ligament, medial to the femoral artery, and ascends on the anterior and medial aspect of the thigh.
Surgical anatomy
When performing liposuction of the lower extremity, understanding the anatomy of the specific areas and the differences in fat layers is important.
Traditionally, both deep and superficial fat layers are found throughout many areas of the body. However, a deep layer is not present from the mid portion of the anterior and posterior thigh, in the calves, and in the ankles. When considering layers of fat, the subdermal layer is approximately 1-2 mm below the skin. The intermediate or superficial layer is 0.5-1 cm below the skin, and the deep layer is approximately 1-2 cm below the skin. Understanding these layers and the anatomy of the lower extremity helps determine whether superficial or deep liposuction can be performed and helps predict the expected results.
Chamosa has categorized the anatomy of the knee. [8] Area 1 is above the kneecap and is in the shape of a banana. It can appear as a flap of fat lapping down over one half of the kneecap. Area 2 is the medial knee, and area 3 is the lateral knee. Areas 4 and 5 are below the kneecap and represent 2 small areas of fat distribution. The lateral fat is usually greater than the internal or medial fat. Area 6 is the area from the inner lower kneecap to the upper calf. This gives the leg a tubular appearance.
Chamosa also describes the ankle and distal portion of the leg as a rhomboid prism. [9] He describes the major axis in the anterior-to-posterior direction, with 4 edges and 4 rectangular sides. The anterior edge is a prolongation of the anterior crest and tendon of the tibialis anterior muscle. The dorsal edge is the tendon calcaneus. The medial edge is the internal border of the tibia and medial malleolus. The lateral edge is the tendon of the peroneus longus and brevis muscles, which finish in the lateral malleolus.
The 4 sides of the rhomboid prism are seen in the frontal view as anteromedial and anterolateral and in the dorsal view as posteromedial and posterolateral. Adiposities of the ankle zone extend from the line between the lateral malleolus and medial malleolus. With exaggerated lipodystrophies, the malleoli prominences remain hidden.
In addition to excess fat over the malleoli, fat can overlie the inferior gastrocnemius muscles, leading to loss of definition.
Contraindications
Patients with a history of hypercoagulability, including deep venous thrombosis or thromboembolic events, should not undergo surgery. Active phlebitis is an absolute contraindication to this procedure. Checking for superficial vascular patterns and signs of a tendency toward venous insufficiency (ie, hemosiderin deposition, edema, varicose veins, spider veins) is important. Vein stripping for severe varicosities should precede liposuction by at least 3 months.
Evaluate the patient for lower extremity edema or venous disorders. Peripheral edema is generally not exacerbated by lipoplasty, but it may cause disappointing long-term results. In general, if venous competency is in question, refer the patient to a vascular surgeon for evaluation prior to liposuction.
-
Descent of the saphenous nerve down the anteromedial aspect of the leg.
-
Saphenous nerve dermatome of the anteromedial leg.
-
Saphenous nerve dermatome at the level of the foot.