Practice Essentials
Mandible fractures are a frequent injury because of the mandible's prominence and relative lack of support. As with any facial fracture, consideration must be given for the need of emergency treatment to secure the airway or to obtain hemostasis if necessary before initiating definitive treatment of the fracture.
Workup in mandibular fractures
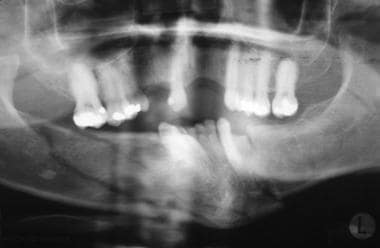
The following types of radiographs are helpful in the diagnosis of mandibular fractures:
-
Panoramic radiograph
-
Lateral oblique radiographs
-
Posteroanterior (PA) mandibular view
-
Reverse Towne view
-
Mandibular occlusal view
-
Periapical radiographs
Initial screening of patients is most effective with a panoramic radiograph, since it shows the entire mandible, including the condyles.
Management of mandibular fractures
The use of preoperative and perioperative antibiotics in the treatment of mandibular fractures, especially in the dentate portion, is well established to reduce the risk of infection. [1, 2]
Means of closed reduction in dentate patients include the following:
-
Erich arch bars
-
Bridle wire
-
Ivy loops
Means of open reduction in mandibular fractures include the following:
-
Wire osteosynthesis
-
Plate fixation
-
Compression screws
History of the Procedure
The first description of mandibular fracture was as early as 1650 BC, when an Egyptian papyrus described the examination, diagnosis, and treatment of mandible fractures. Many patients received either improper treatment or no treatment and, subsequently, died. Hippocrates was the first to describe reapproximation and immobilization through the use of circumdental wires and external bandaging. The importance of establishing proper occlusion first was described in a textbook written in Salerno, Italy, in 1180. Maxillomandibular fixation was first mentioned in 1492, in an edition of the book Cirugia printed in Lyons. Chopart and Desault used dental prosthetic devices to immobilize fracture segments. [3]
Most fracture treatment, however, involved some form of external bandage or wrap, occasionally used in conjunction with a bridle wire, until the 19th century, when Gilmer reformed the treatment of fractures by fixated full arch bars on the mandible and the maxilla. [4] In 1888, Schede was the first to use a solid steel plate held by 4 screws for fixation. [5]
The technique of rigid internal fixation was developed and popularized by Arbeitsgemeinschaft fur Osteosynthesefragen/Association for the Study of Internal Fixation (AO/ASIF) in Europe in the 1970s. The basic principles of the AO, outlined by Spiessl, call for primary bone healing under conditions of absolute stability. [6] Rigid internal fixation must neutralize all forces (tension, compression, torsion, shearing) developed during functional loading of the mandible to allow for immediate function. This is accomplished by interfragmentary compression plates. Use an inferior border plate to counter compression forces and a superior border plate or arch bars to counter traction or tension forces at the superior border. [7]
AO reconstruction plates also impacted the management of comminuted and infected mandibular fractures; Ellis reported a 7.5% infection rate in treatment of mandibular angle fractures with an AO reconstruction plate without intermaxillary fixation (IMF). [8]
During the same time that Spiessl was expounding the AO doctrine, Champy et al in France were developing the concept of adaptive osteosynthesis. Champy advocated transoral placement of small, thin, malleable, stainless steel miniplates with monocortical screws along an ideal osteosynthesis line of the mandible. Champy believed that compression plates were unnecessary because of masticatory forces that produce a natural strain of compression along the inferior border. [9]
These 2 changes of AO rigid internal fixation and the Champy method of monocortical miniplates revolutionized the treatment approach to mandibular fractures. Many fractures previously treated with closed reduction or open reduction with wire osteosynthesis are now commonly treated with open reduction with plate and screw fixation. An example of this evolution is the treatment of comminuted mandibular fractures. These were thought to be treated best by closed reduction to minimize stripping of the periosteum of small bone fragments. Although this treatment modality is still used, rigid fixation now enables the clinician to avoid closed reduction with the use of reconstruction plates and good soft tissue coverage. [10]
Epidemiology
Frequency
Numerous investigators have reported studies on populations on all continents; fractures of the mandible have been reported to account for 36-70% of all maxillofacial fractures. [11, 12, 8, 13] All reports apparently show a higher frequency in males aged 21-30 y. [14] Other contributing factors, such as socioeconomic status, environment, alcohol use, and mechanisms, show greater variability. [15, 16]
Etiology
Major etiologic factors vary based on geographic location. Investigators in countries such as Jordan, [17] Singapore, [18] Nigeria, [19] ] ,[ [20] New Zealand, [21] Denmark, [22] Greece, [23] Japan, [24] and Brazil [25] reported motor vehicle accidents to be the most common cause; in reports from other countries such as Greenland, [26] Finland, [27] Scotland, [28] Sweden, [29] Bulgaria, [30] and Canada [13] found assaults to be the most common etiology.
Results in the United States have been divided. In 1982, Olson and associates demonstrated that vehicular accidents caused 48% of fractures. [31] In 1985, Fridrich and associates demonstrated that altercations accounted for 47% of fractures and automobile accidents for 27%. [32] Also in 1985, Ellis et al reported that 43% were caused by vehicular accidents, 34% were caused by assaults, 7% were work-related, 7% occurred as the result of a fall, 4% occurred in sporting accidents, and the remainder had miscellaneous causes. [8]
A retrospective cohort study by Afrooz et al using hospitalized patients enrolled in the National Trauma Data Bank between 2001 and 2005 found that males made up 80% of mandibular fracture patients, with the most frequent mechanisms of injury in males being assault (49.1%), motor vehicle accidents (25.4%), and falls (12.8%). Among females, the most common injury mechanism was motor vehicle accidents (53.7%), with falls (23.7%) and assault (14.5%) being the next most frequent. [33]
Vaillant and Benoist described 14 cases of gunshot injuries to the mandible; 2 children had injuries that resulted from accidents, and the adults' fractures were caused by suicide or assault. [34]
Location of mandibular fractures
Fridrich and associates showed that most fractures occur in the body (29%), condyle (26%), and angle (25%) of the mandible. The symphyses account for 17% of mandibular fractures, whereas fractures of the ramus (4%) and coronoid process (1%) have lower occurrence rates. In automobile accidents, the condylar region was the most common fractured site. In motorcycle accidents, the symphysis was fractured most often. When assault was the cause, the angle demonstrated the highest incidence of fracture. [32]
A literature review by Giovacchini et al indicated that the presence of a mandibular third molar doubles the risk of mandibular angle fracture. The third molar’s position, as categorized using the Pell and Gregory impaction classification, also apparently can increase the risk of angle fracture, particularly when the impaction is class C, class II, or class III. [35] A study by El-Anwar et al also found an association between impacted mandibular third molars and increased risk of mandibular angle fracture. [36]
Associated injuries with mandibular fractures
Fridrich and associates reported that in patients with mandible fractures, 43% of the patients had an associated injury. Of these patients, head injuries occurred in 39% of patients, head and neck lacerations in 30%, midface fractures in 28%, ocular injuries in 16%, nasal fractures in 12%, and cervical spine fractures in 11%. Other injuries present in this group were extremity trauma in 51%, thoracic trauma in 29%, and abdominal trauma in 14%. Of the 1067 patients studied, 12 (2.6%) died of their associated injuries before the mandible fracture could be treated. [32]
Number of fractures per mandible
In patients with mandible fractures, 53% of patients had unilateral fractures, 37% of the patients had 2 fractures, and 9% had 3 or more fractures. [31]
Pathophysiology
Classification of mandibular fractures
See the list below:
-
Simple or closed - Fracture that does not produce a wound open to the external environment, whether it be through the skin, mucosa, or periodontal membrane
-
Compound or open - Fracture in which an external wound, involving skin, mucosa, or periodontal membrane, communicates with the break in the bone
-
Comminuted - Fracture in which the bone is splintered or crushed
-
Greenstick - Fracture in which one cortex of the bone is broken and the other cortex is bent
-
Pathologic - Fracture occurring from mild injury because of preexisting bone disease
-
Multiple - Variety in which two or more lines of fracture on the same bone are not communicating with one another
-
Impacted - Fracture in which one fragment is driven firmly into the other
-
Atrophic - Fracture resulting from severe atrophy of the bone, as in edentulous mandibles
-
Indirect - Fracture at a point distant from the site of injury
-
Complicated or complex - Fracture in which considerable injury to the adjacent soft tissues or adjacent parts occurs; may be simple or compound
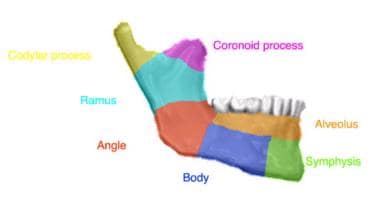
Classification by anatomic region
See the list below:
-
Symphysis - Fracture in the region of the central incisors that runs from the alveolar process through the inferior border of the mandible
-
Parasymphyseal - Fractures occurring within the boundaries of vertical lines distal to the canine teeth
-
Body - From the distal symphysis to a line coinciding with the alveolar border of the masseter muscle (usually including the third molar)
-
Ramus - Bounded by the superior aspect of the angle to two lines forming an apex at the sigmoid notch
-
Condylar process - Area of the condylar process superior to the ramus region
-
Coronoid process - Includes the coronoid process of the mandible superior to the ramus region
-
Alveolar process - Region that normally contains teeth
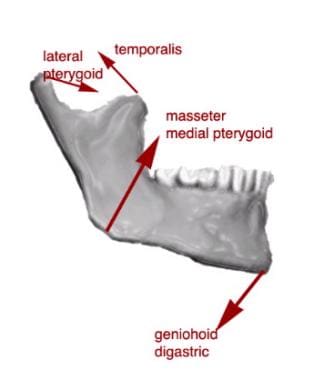
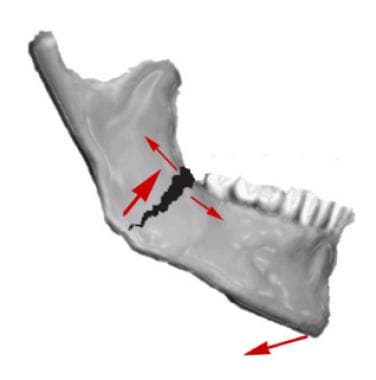
The effect of muscle action on the fracture fragments is important in classification of mandibular angle and body fractures. Angle fractures may be classified as (1) vertically favorable or unfavorable and (2) horizontally favorable or unfavorable. The muscles attached to the ramus (masseter, temporal, medial pterygoid) pull the proximal segment upward and medially and the symphysis of the mandible is displaced inferiorly and posteriorly by the pull of the digastric, geniohyoid, and genioglossus muscles.
When the fractures are vertically and horizontally unfavorable, the fragments tend to be displaced.
Conversely, these same muscles tend to stabilize the bony fragments in horizontally and vertically favorable fractures.
Condylar fractures are classified as extracapsular, subcondylar, or intracapsular. The lateral pterygoid tends to cause anterior and medial displacement of the condylar head. Five types of condylar fractures are described in order of increasing severity:
-
Type I is a fracture of the neck of the condyle with relatively slight displacement of the head. The angle between the head and the axis of the ramus varies from 10-45°.
-
Type II fractures produce an angle from 45-90°, resulting in tearing of the medial portion of the joint capsule.
-
Type III fractures are those in which the fragments are not in contact, and the head is displaced medially and forward. The fragments are confined within the area of the glenoid fossa. The capsule is torn, and the head is outside the capsule.
-
Type IV fractures of the condylar head articulate on or in a forward position with regard to the articular eminence.
-
Type V fractures consist of vertical or oblique fractures through the head of the condyle.
Presentation
History
See the list below:
-
A complete medical and psychiatric history is important for diagnosis and future treatment of mandible fractures.
-
Thoroughly explore possible bleeding disorders, endocrine disorders, [37] or bony and collagenous disorders prior to surgery.
-
History of previous mandibular trauma can help prevent misdiagnoses.
-
Any pretraumatic temporomandibular joint dysfunction needs to be documented in detail prior to treatment.
-
The source, size, and direction of traumatic force are helpful in diagnosis.
Fractures sustained by a fist tend to have single, simple, or nondisplaced fractures whereas patients involved in motor vehicle accidents sustain compound comminuted fractures.
Localized trauma (eg, pipe, stick, hammer) tends to cause a single comminuted fracture since the force is concentrated in a small area.
Trauma distributed to a larger surface area may cause several fractures (eg, symphysis, condyle) secondary to distribution of the force throughout the mandible.
Direction of the force can help in making the diagnosis of concomitant fractures. Trauma directed to the chin often results in a symphyseal fracture with concomitant unilateral or bilateral condylar fractures.
Clinical examination
See the list below:
-
Advanced trauma life support protocol
Note facial lacerations, swellings, and hematomas. A common site for a laceration is under the chin, and this should alert the clinician to the possibility of an associated subcondylar or symphysis fracture.
From behind the supine or seated patient, bimanually palpate the inferior border of the mandible from the symphysis to the angle on each side. Note areas of swelling, step deformity, or tenderness.
Note areas of paresthesia, dysesthesia, or anesthesia along the distribution of the inferior alveolar nerve. Numbness in this region is almost pathognomonic of a fracture distal to the mandibular foramen.
Standing in front of the patient, palpate the movement of the condyle through the external auditory meatus. Pain elicited through palpation of the preauricular region should alert the clinician to a possible condylar fracture.
Observe any deviation on opening of the mouth. Classically, deviation on opening is toward the side of the mandibular condyle fracture. Note any limited opening and trismus that may be a result of reflex muscle spasm, temporomandibular effusion, or mechanical obstruction to the coronoid process resulting from depression of the zygomatic bone or arch.
Changes in occlusion are highly suggestive of a mandibular fracture. A change in occlusion may be due to a displaced fracture, fractured teeth and alveolus, or injury to the temporomandibular joint.
Look for intraoral mucosal or gingival tears. Floor of the mouth ecchymosis may indicate a mandibular body or symphyseal fracture.
If a fracture site along the mandible is suggested, grasp the mandible on each side of the suspected site and gently manipulate it to assess mobility.
Indications
The indications for closed versus open reduction have changed dramatically over the last century. The ability to treat fractures with open reduction and rigid internal fixation (ORIF) has dramatically revolutionized the approach to mandibular fractures. [38, 39]
Traditionally, closed reduction (CR) and ORIF with wire osteosynthesis have required an average of 6 weeks of immobilization by maxillomandibular fixation (MMF) for satisfactory healing. Difficulties associated with this extended period of immobilization include airway problems, poor nutrition, weight loss, poor hygiene, phonation difficulties, insomnia, social inconvenience, patient discomfort, work loss, and difficulty recovering normal range of jaw function. In contrast, rigid and semirigid fixation of mandible fractures allow early mobilization and restoration of jaw function, airway control, improved nutritional status, improved speech, better oral hygiene, patient comfort, and an earlier return to the workplace. [40, 41, 14]
Schmidt et al [42] and Shetty et al [43] performed financial analysis comparing patients treated with closed reduction and MMF with those treated with ORIF, and found, at least within the patient population at risk for mandible fractures, that the closed treatment was more cost-effective.
Indications for closed reduction
See the list below:
-
Nondisplaced favorable fractures: Open reduction carries an increased risk of morbidity, thus use the simplest method to reduce and fixate the fracture.
-
Grossly comminuted fractures: Generally, these are best treated by closed reduction to minimize stripping of the periosteum of small bone fragments.
-
Fractures in children involving the developing dentition: Such fractures are difficult to manage by open reduction because of the possibility of damage to the tooth buds or partially erupted teeth. [44] A special concern in children is trauma to the mandibular condyle. [45] The condyle is the growth center of the mandible, and trauma to this area can retard growth and cause facial asymmetry. Early mobilization (7-10 d of intermaxillary fixation) of the condyle is important. [46] If open reduction is necessary because of severe displacement of the fracture, the use of resorbable fixation or wires along the most inferior border of the mandible may be indicated.
-
Coronoid fractures: These fractures usually require no treatment unless impingement on the zygomatic arch is present.
-
Treatment of condylar fractures: This is one of the more controversial topics in maxillofacial trauma. [47] Indications for open reduction are discussed below. If condylar fractures do not fall within this criteria, they can be treated with closed reduction for a period of 2-3 weeks to allow for initial fibrous union of the fracture segments. If the condylar fracture is in association with another fracture of the mandible, treat the noncondylar fracture with ORIF, and treat the condylar fracture with closed reduction.
Indications for open reduction
See the list below:
-
Displaced unfavorable fractures through the angle of the mandible: Often, the proximal segment is displaced superiorly and medially and requires an open technique for proper reduction. [48]
-
Severely atrophic edentulous mandibles: These have little cancellous bone remaining and minimal osteogenic potential, and fracture healing may be delayed. Ellis and Price advocate an aggressive protocol of ORIF with rigid fixation and acute bone grafts. [49] They demonstrated no complications with this approach, despite the advanced age and medical comorbidities of this patient population. [49]
-
Complex facial fractures: Such fractures can be reconstructed best after open reduction and fixation of the mandibular segments to provide a stable base for restoration.
-
Condylar fractures: Although strong evidence supporting open reduction of condylar fractures is lacking, a specific group of individuals benefit from surgical intervention. The classic article by Zide and Kent lists absolute and relative indications for open reduction of the fractured mandibular condyle. [50] Palmieri et al [51] and De Riu et al [52] demonstrated better long-term range of motion and occlusion in patients with condylar factures treated with ORIF versus closed reduction and MMF.
Absolute indications
Displacement of the condyle into the middle cranial fossa
Inability to obtain adequate occlusion by closed techniques [53]
Lateral extracapsular dislocation of the condyle
Relative indications
Bilateral condylar fractures in an edentulous patient when splints are unavailable or impossible because of severe ridge atrophy
Unilateral or bilateral condylar fractures when splinting is not recommended because of concomitant medical conditions or when physiotherapy is not possible
Bilateral fractures associated with comminuted midfacial fractures
-
Mandibular nonunions require open access for debridement and subsequent reduction. [54]
-
Malunions after improper reduction often require osteotomies through open surgical approaches to correct mandibular discrepancies. [55]
Timing of open reduction
Traditional teaching has been that mandible fractures should be reduced within 24 hours of injury. [9] Recent studies have shown no increase in complications with a delay of repair beyond 24 hours. [56, 57, 58, 59, 60, 61] Biller et al showed no increase in infections in repairs delayed over 72 hours, but there was an increased incidence of technical complications. [59] Barker et al showed no correlation of complications and delay of repair of over 2 weeks. [61]
Relevant Anatomy
The mandible is a U-shaped bone; the middle portion is termed the symphysis. The horizontal body of the mandible bears the tooth-bearing alveolar process. Distally, the horizontal body of the mandible joins the vertical ramus at the angle. The ramus has both the coronoid and condylar processes. The coronoid is the site of insertion for the temporalis muscle, while the condylar process articulates with the mandibular fossae of the temporal bone.
Contraindications
Contraindications to closed reduction include the following (these patients benefit from open reduction and rigid internal fixation [ORIF]):
-
Patients with poorly controlled seizure history
-
Patients with compromised pulmonary function (ie, moderate-to-severe asthma, chronic obstructive pulmonary disease)
-
Patients with psychiatric or neurologic problems
-
Patients with eating or GI disorders
-
The anatomic regions of the mandible.
-
The muscular forces acting upon the mandible.
-
A "favorable" body fracture with muscular force not tending to distract the fracture.
-
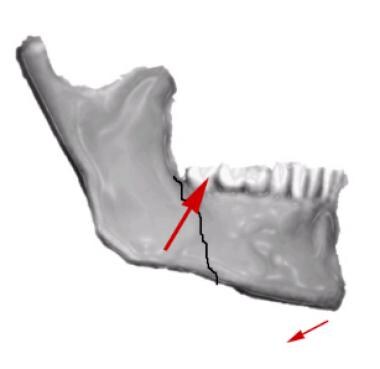
An "unfavorable" angle fracture with distracting muscular forces.
-
Right mandibular condylar fracture.
-
Retromandibular approach to right mandibular condylar fracture.
-
Intraoperative view. Fixation of right mandibular condyle fracture.
-
Mandibular fracture. Postoperative pantomogram.
-
Mandibular fracture. Close-up view of postoperative pantomogram.
-
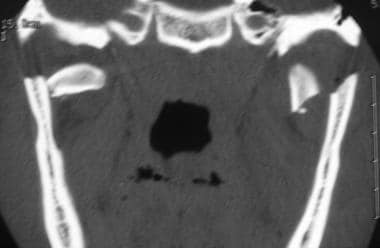
Mandibular fracture. Coronal CT scan demonstrating bilateral high condylar fractures.
-
Mandibular fracture. Postoperative coronal image demonstrating open reduction internal fixation of the left condylar fracture to restore posterior vertical height.
-
Mandibular fracture. Postoperative pantomogram.
-
Mandibular fracture. Intraoperative view. Reconstruction plate used to span continuity defect of right mandibular body.
-
Mandibular fracture. Autologous bone harvested from the patient's anterior iliac crest placed into defect.
-
Mandibular sagittal symphysis fracture and dentoalveolar fracture.
-
Mandibular fracture treated with lag screw fixation and debridement of dentoalveolar segment.
-
Mandibular fracture. Patient lost to follow-up at local county jail presents with infected nonunion of mandibular symphysis.
-
Mandibular fracture. Infection treated with incision and drainage and intravenous antibiotics. Hardware was removed and site debrided. Postoperative posteroanterior cephalometric view demonstrating reconstruction plate in place.
-
Mandibular fracture. Lateral view.
-
Right mandibular parasymphysis fracture.
-
Mandibular fracture treated with 4-hole positional plate and maxillomandibular fixation.
-
Comminuted mandibular fracture.
-
Axial CT scan demonstrating multiple fractures of the mandible.
-
Axial CT scan demonstrating severe displacement.
-
Mandibular fracture. Intraoperative view demonstrating fixation of mandibular segments.
-
Mandibular fracture. Left lateral view.
-
Mandibular fracture. Right lateral view.
-
Mandibular fracture. Axial CT scan demonstrating status post fixation.
-
Right mandibular ramus and left mandibular parasymphysis fractures.
-
Mandibular fracture. Pantomogram status post fixation.
-
Mandibular fracture. Postoperative posteroanterior cephalometric view.
-
Right sagittal mandibular body fracture and left parasymphysis fracture.
-
Mandibular fracture. The right side was treated with 3 positional screws to engage buccal and lingual cortices of sagittal fracture. The right side is rigidly fixated with a 6-hole plate.
-
Right mandibular body fracture. Left mandibular angle fracture going through tooth #17.
-
Right mandibular body and left mandibular angle fractures status post fixation. Tooth #17 was extracted.
-
Mandibular fracture. Interarch elastics may be used for maxillomandibular fixation. They also may be used loosely for guidance during postoperative care.
-
Left mandibular angle fracture involving tooth #17. Right mandibular body fracture.
-
Tooth #17 was extracted. A superior border plate was placed at the left mandibular angle. An inferior border plate was placed for the right mandibular body fracture.
-
Mandibular fracture. Patient presents with occlusal step off between right mandibular central and lateral incisors.
-
Mandibular fracture. View of occlusal step off.
-
Mandibular fracture. Bridle wire used to decrease mobility and provide patient comfort.
-
Mandibular fracture. Barton bandage used to decrease fracture mobility and provide patient comfort until definitive treatment.
-
Left mandibular body fracture.
-
Mandibular fracture. Open reduction rigid internal fixation of left mandibular body fracture.
-
Mandibular fracture. Postoperative radiograph demonstrating reduction and fixation.
-
Mandibular fracture. Patient with poorly controlled type 1 diabetes with left open, complete, moderately displaced mandibular angle fracture between teeth #17 and #18.
-
Mandibular fracture. Treated initially with a superior border plate and an inferior border plate as well as extraction of tooth #17.
-
Mandibular fracture. Patient returns with infected nonunion of left mandibular angle and loose hardware. The superior border plate was removed. Tooth #18 was extracted. The patient was treated with intravenous and oral antibiotics.
-
Mandibular fracture. Rigid fixation with an 8-hole plate. Two holes in the center are used to span the fracture site.