Background
The leg is a complex district with functions of weight-bearing support, stability, and motility. The osseus structure of the lower leg is composed of the tibia and the fibula. The tibia is most responsible for lower leg functions, while the fibula is a fairly expendable bone.
Occasionally, traumas, neoplasms, or acquired or congenital malformations affect the tibia, inhibiting leg functions and consequently necessitating bone reconstruction or substitution. [1] Small bone defects of the tibia are treated with external fixation and cancellous bone grafting, with satisfactory results.
The management of extensive and complex defects is more challenging and often results in leg amputation or shortening. Leg amputation is a severe mutilation that alters the patient's work and social life by limiting ambulation and self-sufficiency. Limb shortening is also responsible for an asymmetric gait and posture deformities.
The advent of microsurgery and its application to bone transfers has radically changed the treatment of complex tibial injuries, allowing plastic surgeons to reconstruct wide bone gaps with optimal functional, morphological, and cosmetic outcome—in most instances, avoiding the need for limb amputation or shortening. Free vascularized fibular transfer has become the standard practice to bridge long (>6 cm) bone defects of the extremities.
History of the Procedure
In the 1970s, microsurgical techniques were mainly used in emergency settings to reestablish vascular perfusion of amputated limbs and salvage them. Complex tibial fractures or extensive bone defects were usually treated by orthopedic surgeons with autologous nonvascularized cancellous bone grafting stabilized with external fixation. Complex open fractures of the tibia were associated with an increased incidence of delayed union (20-40%), nonunion (7-45%), and osteomyelitis (2.7-27%). [2] These contributed to a high incidence rate of delayed amputation, ranging from 20-75%.
Later, cortical bone grafting with rigid internal fixation was introduced. The early results of the use of the fibula graft protibia appeared satisfactory. In 1980, Enneking et al reported a 95% success rate in the postneoplastic reconstruction of tibial gaps greater than 7.5 cm with large, nonvascularized fibular autografts. This procedure demonstrated several complications, such as stress fractures (32%), bone nonunions (27% at 6 mo), and tibial curvatures. To reduce the complication rate, which increased in infected and poorly vascularized wounds, the use of free bone transfer microsurgically revascularized to the recipient area was proposed.
In 1973, Ueba and O'Brien evaluated the fibula as a donor site for the free microvascular bone flap. The first report of a successful free bone transplant was in 1974 by Ostrup and Fredrickson, who successfully transplanted free rib grafts vascularized on intercostal arteries in dogs. [3]
In 1975, Taylor et al performed the first 2 free microvascular fibula transfers on human patients to reconstruct tibial bone gaps. [4] Microvascular bone flaps were shown to heal more rapidly, with fewer complications and earlier functional recovery than conventional nonvascularized grafts. Gradually, microvascular bone flaps have gained popularity, becoming the treatment of choice for bone defects larger than 6 cm or located in poorly vascularized and contaminated wound beds.
Other donor areas have been used, such as ribs, the iliac crest, the radius, the metatarsus, and the scapula. Each of these has demonstrated some pitfalls and limits because of the reduced amount and poor quality of the bone available to be harvested, the possibility of raised muscle or skin in the flap, and the morbidity of the donor area.
Chen and Yan [5] and Harrison reported on the successful free osteocutaneous fibula flap, and, in 1982, Bovet et al [6] reported the use of an osteomuscular flap by including one half of the soleus muscle together with the fibula bone stock. In 1983, Ueba and O'Brien transplanted a bone stock as long as 30 cm, eventually associated to muscle and skin, using a free osteomyocutaneous fibula flap, with negligible donor area morbidity. Actually, the free fibula flap and the rigid fixation system are the universally recognized methods of treatment of complex tibial defects.
Problem
The tibia is a long bone, the anterior third of which is placed subcutaneously in the leg throughout most of its length. It is covered only by a thin layer of skin and subcutaneous tissue, with no surrounding muscle cuff. This anatomic location may be explained by the need to protect the blood vessels and nerves of the leg, which are located deep laterally, medially, and posteriorly. This position makes the tibia easily vulnerable to traumas, often resulting in exposed fractures.
 Clinical Case 2. Preoperative picture. Medial view of the left leg with exposed fracture of the inferior third of the tibia (Gustilo stage 3c) and loss of skin cover.
Clinical Case 2. Preoperative picture. Medial view of the left leg with exposed fracture of the inferior third of the tibia (Gustilo stage 3c) and loss of skin cover.
 Clinical Case 2. Preoperative picture. Lateral view of the left leg with exposed fracture of the inferior third of the tibia (Gustilo stage 3c).
Clinical Case 2. Preoperative picture. Lateral view of the left leg with exposed fracture of the inferior third of the tibia (Gustilo stage 3c).
Because of the exposure of devascularized bone in a contaminated bed, the spontaneous healing of these wounds is usually aggravated by delayed union, nonunion, infection, and osteomyelitis. Replacing necrotic or denuded bone with a skeletal substitute capable of healing in such an unfavorable environment is a problem with a difficult solution, even when adequate soft tissue cover is available.
The reconstruction of partially comminuted fractures or small bone gaps usually benefits from cancellous or devascularized cortical bone grafting and external fixation.
On the contrary, the reconstruction of segmental, comminuted tibial fractures or extensive bone defects requires vascularized bone grafts to overcome infection and restore bone continuity and blood supply. The Ilizarov technique is a procedure used for the reconstruction of such defects, but the bulky apparatus, long lengthening and union times, and pin tract infection limit the present method. [7]
Occasionally, malignant neoplasms such as osteosarcomas, chondrosarcomas, Ewing sarcomas, and metastatic tumors may involve the tibia and require resection of the bone and surrounding tissues. [8] In these patients, local curettage is not recommended because of the high incidence of local recurrences and distant metastasis and because of the poor rate of disease-free survival. Wide en bloc excision is indicated, and long bone reconstruction is useful to avoid amputation.
Acquired and congenital pathologies, such as osteomyelitis or pseudoarthrosis, also may affect the tibia, requiring resection and long bone substitution. In these patients, the more favorable local vascular and soft tissue conditions make reconstruction easier; nevertheless, bone grafts still yield high complication rates when gaps greater than 6 cm must be restored.
Generally, the goal in the reconstruction of tibial defects is to restore the anatomy of the altered segment, gaining a satisfactory functional recovery. Finding a bone substitute of adequate length and width, customized to the defect, covered by vascularized muscle or skin, and stabilized in the most anatomic position compatible with maximal functional return is often a great demand. Currently, microvascular free bone grafts are the best answer.
Etiology
Large defects of the tibia are more often caused by low- to high-speed injuries resulting in exposed comminuted fractures than by the resection of bone tumors, osteomyelitis, or pseudoarthrosis.
Tibial fractures are the most common long bone fractures of the body skeleton. The most frequent causes are motorcycle accidents (28% of patients), vehicle accidents (24%), domestic accidents (13%), pedestrian accidents (12%), crushing lesions (8%), firearm accidents (2%), and miscellaneous causes such as work- and sports-related accidents (13%). For more information on traumatic injury, visit Medscape’s Trauma Resource Center.
Malignant tumors arising from the skeleton frequently involve the long bones such as the tibia. Among these tumors, the most frequent are osteogenic sarcomas, chondrosarcomas, fibrosarcomas, malignant histiocytomas, adamantinomas, lymphomas, angiosarcomas, liposarcomas, Ewing sarcomas, and tumors from metastatic diseases.
Etiologic factors involved in the pathogenesis of bone tumors are generally the same as those recognized for the development of cancer, such as genetic predisposition, exposure to carcinogens, and irradiation.
Chronic osteomyelitis of the tibia may be the consequence of an infection caused by trauma, surgery, or a contiguous infection (exogenous form), or it may be caused by an unknown bacteremia (hematogenous form; see the image below).
 Clinical Case 4. Osteomyelitis of the middle third of the tibial shaft. Shown is a long-standing osteocutaneous fistula secreting pus.
Clinical Case 4. Osteomyelitis of the middle third of the tibial shaft. Shown is a long-standing osteocutaneous fistula secreting pus.
Chronic exogenous osteomyelitis is frequently the result of mistreatment of severe open fractures, leading to nonunion, deep acute infection, and bone incarceration.
Congenital pseudoarthrosis of the tibia is a specific type of nonunion that is present or incipient at birth. It is a rare malformation involving only 1 in 250,000 live births. Etiologic causes are unknown, but this disorder is frequently associated (50-90%) with neurofibromatosis.
Acquired forms of pseudoarthrosis may occur as a result of delayed union of severe fractures, leading to excessive callus formation, reduced stability, and tibial bowing.
Presentation
The classification of tibial fractures considers the mechanism of the trauma, the location, the extent and type of fracture, involvement of soft tissues, and neurovascular impairment. The type of tibial fracture is related to the mechanism involved in its pathogenesis, ie, contusive, clean-cut, tear, degloving, crushing, avulsion, and burst (high speed). Usually, crushing, avulsions, or high-speed bursting injuries lead to more complex defects.
The anatomic classification divides tibial fractures into fractures of the knee, the tibial plate, the tibial shaft, and the ankle. Most of these are of strict pertinence to the orthopedic surgeon, while large, comminuted open fractures of the tibial shaft, commonly associated with wide soft tissue loss, require the expertise of plastic microsurgeons.
The extensive Orthopaedic Trauma Association classification of long bone fractures divides them according to the line of fracture as follows: linear (transverse, oblique, spiral), comminuted (< 50%, >50%, butterfly < 50%, butterfly >50%), segmental (2 level, 3 level, longitudinal split, comminuted), and bone loss (< 50%, >50%, complete).
The clinical classification considers the involvement of soft tissues in open fractures. In 1984, Gustilo and colleagues described 5 different grades in the Association of Osteosynthesis classification, as follows [9] :
-
Grade 1 - Skin lesion smaller than 1 cm; clean; simple bone fracture with minimal comminution
-
Grade 2 - Skin lesion larger than 1 cm; no extensive soft tissue damage; minimal crushing; moderate comminution and contamination
-
Grade 3 - Extensive skin damage with muscle and neurovascular involvement; high-speed injuries; comminution of the fracture; instability
Grade 3a - Extensive laceration of soft tissues with bone fragments covered; usually high-speed traumas with severe comminution or segmental fractures
Grade 3b - Extensive lesion of soft tissues with periosteal stripping, contamination, and severe comminution due to high-speed traumas; usually, exposed bone must be replaced with a local or free flap as a cover
Grade 3c - Exposed fracture with arterial damage that requires repair (see the images below)
 Clinical Case 1. Preoperative radiograph of the traumatized leg. A multiple segmental and exposed spiral fracture of the tibia is identified (Gustilo stage 3c).
Clinical Case 1. Preoperative radiograph of the traumatized leg. A multiple segmental and exposed spiral fracture of the tibia is identified (Gustilo stage 3c).
The association of soft tissue injury with tibial fracture is of great importance in determining the ideal treatment.
Bone fragments or segments that are preserved but devascularized and not covered by healthy soft tissue usually heal into nonunion or pseudoarthrosis or undergo necrosis and require removal and secondary free bone reconstruction.
In 1985, Byrd et al formulated a new and simplified classification of fractures, based on the mechanism of the trauma and bone and soft tissue lesion. [10] They recognized the importance of both the direct and indirect traumatic forces responsible for the bony lesions. Their classification is as follows:
-
Type I - Low-energy fractures; oblique or spiral fracture with clean-cut laceration smaller than 1 cm
-
Type II - Medium-energy trauma; displaced or comminuted fracture with laceration larger than 2 cm and myocutaneous contusion
-
Type III - High-energy trauma; severely displaced or comminuted fracture; segmental fracture or bone defect with laceration larger than 2 cm and loss of skin and muscle substance
-
Type IV - High-energy bursting trauma; crushing or avulsion with arterial damage requiring microvascular repair
Usually, malignant neoplasms involving the tibia, such as osteosarcomas, may be discovered incidentally during a routine roentgenogram of the skeleton or may manifest as a mass evoking pain by irritating surrounding tissues or causing a spontaneous fracture.
Occasionally, they may be discovered because of the presence of regional nodal metastasis of a silent primary bony lesion. Diagnosis is made using images from standard roentgenograms, nuclear magnetic resonance (NMR) and CT imaging scans, arteriograms, guided biopsies, and the report from the pathologist.
Radiologically, these malignant neoplasms may manifest variably as lytic or sclerotic lesions. The classification is according to the extent of the bony lesion, invasion of soft tissues, presence of regional or distant spread, and histologic grade.
In 1989, Enneking staged tumors in relation to anatomic site as follows [11] :
-
Tumors
T1 - Intracapsular
T2 - Extracapsular intracompartmental
T3 - Extracompartmental
-
Grading
G0 - Benign
G1 - Low-grade malignant
G2 - High-grade malignant
-
Presence of metastases
M0 - Absent
M1 - Present
Enneking classified them in 3 main stages (I, II, III) and 2 substages (A, B) and differentiated treatment in relation to the stage. Staging grade site metastasis is as follows:
-
IA, G1, T1, M0
-
IB, G1, T2, M0
-
IIA, G2, T1, M0
-
IIB, G2, T2, M0
-
IIIA, G1-2, T1, M1
-
IIIB, G1-2, T2, M1
The hallmark of chronic osteomyelitis is infected dead bone within a compromised soft tissue envelope. Usually, osteomyelitis of the tibia manifests clinically as a torpid skin ulcer or cutaneous fistula secreting pus and overlying a chronic fracture site. One or more foci in the bone may contain purulent material, granulation tissue, or a sequestrum, and they may be surrounded by sclerotic, avascular bone and covered by scarred muscle and subcutaneous tissue.
Systemic symptoms usually subside. Bone necrosis, sclerosis, and lysis may be evident on radiographs. The diagnosis is supported by findings of radiolabeled monoclonal antibodies against leukocyte antigen scanning.
According to Cierny and Mader, clinical classification depends on physiologic and anatomic criteria. [12] The physiologic criteria are as follows:
-
Class A - Normal response host
-
Class B - Compromised wound healing
-
Class C - Potentially worsening
Anatomic criteria are as follows:
-
Type I - Medullary
-
Type II - Superficial
-
Type III - Localized full-thickness
-
Type IV - Diffuse
Congenital pseudoarthrosis usually manifests in adolescence as an incorrect development of one of the main bone articulations.
Boyd classified congenital pseudoarthrosis into 6 types, as follows [13] :
-
Type I - Anterior bowing and defect present at birth
-
Type II - Hourglass constriction at birth
-
Type III - Congenital cyst
-
Type IV - Sclerotic segment with medullary obliteration
-
Type V - Dysplastic fibula
-
Type VI - Intraosseous neurofibroma or schwannoma
Acquired pseudoarthrosis manifests clinically as a chronically unstable bone union at the fracture site. Angulation or displacement of the bone segments may be evident. A hypertrophic callus may be present on the radiograph, together with a still-evident line of fracture (see the images below).
 Clinical Case 1. Radiologic evidence of the pseudoarthrosis. Laterolateral radiograph of tibial pseudoarthrosis that shows bone nonunion and anterior bowing.
Clinical Case 1. Radiologic evidence of the pseudoarthrosis. Laterolateral radiograph of tibial pseudoarthrosis that shows bone nonunion and anterior bowing.
Indications
Traumatic fractures, tumors, osteomyelitis, or pseudoarthrosis may require compromised bone resection and subsequent reconstruction. Conventional treatments (ie, bone grafting, Ilizarov technique) are best indicated for limited (< 6 cm) defects because of the long time needed for newly formed bone to consolidate.
Microsurgical bone transfers are indicated when conventional treatments are not useful (ie, bone defect >6 cm, poorly vascularized or infected recipient beds) or have previously failed.
Primary indications for free bone transfer to tibial defects are as follows:
-
Severely comminuted fractures or wide bone loss greater than 6 cm (grade 3a-3c from Gustilo classification, type III from Byrd classification)
-
Wide (>6 cm) en bloc tibial resections for cancer
-
Wide bone resection (>6 cm) for congenital pseudoarthrosis of the tibia
Secondary indications for free bone transfer are as follows:
-
Wide bone resection of acquired pseudoarthrosis or chronic osteomyelitis following nonunions for failed conventional treatment of fractures
-
Short limb (>6 cm) following conventional treatment of fractures or reimplantation of avulsed limb, with or without distraction
-
Amputation stump lengthening
-
Wide soft tissue coverage of bone defects (< 6 cm) of the lower third of the leg (osteocutaneous-myo-osteocutaneous flap)
Relevant Anatomy
The framework of the lower leg is composed of 2 long bones, the fibula and tibia, which are arranged in parallel.
The fibula is thin and long. It can be divided into the body and the upper and lower extremities. The body can be considered a triangular prism. The upper extremity articulates with the articular face of the tibial epiphysis. The lower extremity joins the tibia in the tibiotarsal joint. The fibula provides insertion to many of the muscles of the leg.
The tibia is a long and thick bone. Anatomically, it can be divided into a body and 2 extremities. The body is a triangular prism, with 3 faces and 3 margins. The upper extremity is large and expands in 2 masses that form the tibial plate (which articulates with the femur). The lower extremity presents a basal articular surface and a medial thick protrusion, the medial malleolus, which, together, form the main part of tibiotarsal joint. Laterally, the lower tibial extremity articulates with the fibular lower epiphysis.
The tibia and fibula are also connected along their length by a fibrous membrane termed the interosseus membrane.
These 3 structures together divide the leg into 2 anatomic compartments, the anterior and posterior. The anterior compartment is further divided into anterior and anterolateral by a thick intermuscular fascia. [14]
The anterior compartment has 4 muscles termed the (1) extensor digitorum longus; (2) extensor hallucis longus; and (3) peroneus tertius, which originates from the fibula, and (4) the tibialis anterior, which originates from both bones. All together, these muscles bend and medially flex the feet. These muscles are vascularized by anterior tibial vessels and innervated by the deep peroneal nerve. Both vascular and nervous structures run deeply along the interosseous membrane.
The anterolateral compartment holds 2 muscles, the long and short (brevis) peroneus. Their action consists of extension, medial torsion, and abduction of the feet. They are vascularized by vessels from the peroneal artery and innervated by the superficial peroneal nerve (which runs deeply in the upper two upper thirds and then becomes superficial to the lower one third of the anterior skin of the leg).
The posterior compartment is divided into superficial and deep by a thin intermuscular fascia. Three muscles are located in the superficial compartment, termed the gastrocnemius, soleus, and plantaris. The gastrocnemius and plantaris originate from the femur, while the soleus originates from the fibula and tibia. The gastrocnemius and soleus join together in a thick tendon that inserts into the calcaneal bone (tendo calcanea). The plantaris is a thin muscle, the tendon of which medially follows the bigger triceps tendon to insert into the calcaneal bone. All of these muscles extend the feet (the gastrocnemius also bends the leg on the thigh) with a little medial torsion. They are vascularized by vessels from the popliteal artery and innervated by branches of the tibialis nerve from the popliteal fossa. The lateral portion of the soleus is also fed by branches from the peroneal artery.
The deep compartment contains 4 muscles termed the popliteus, flexor digitorum longus, flexor hallucis longus, and tibialis posterior. The popliteus helps bending of the knee and medially rotating the leg; the other muscles extend and medially rotate the feet and bend the toes.
The blood supply of the area is provided by 2 arteries, the tibial posterior and the peroneal. The first, which is a terminal branch of the popliteal artery, runs along the tibial posterior muscle, moving medially. It provides nutritional vessels for the muscles of the medial side of the compartment and an artery for the tibial bone.
The peroneal artery originates from the posterior tibial artery approximately 3-4 cm from the division between the popliteal and anterior tibial arteries. This artery runs laterally and downward along the fibula. It provides arteries for the surrounding muscles, an artery for the fibula (approximately 17 cm from its origin), and many perforating arteries for the lateral skin of the leg. [15]
A single nerve, the tibial nerve, innervates the compartment. It runs deeply in the first half of the leg and then moves medially and superficially.
The sciatic popliteal nerve runs subcutaneously at the level of the head of the fibula, where it passes around its neck, to deeper into the muscles of the anterior compartment.
Contraindications
The following are contraindications to free bone transfer to tibial defects:
-
Crushing or avulsion injuries with jeopardized lower limb vascularization (high risk of failure of vascular anastomosis)
-
Crushing or avulsion injuries with severe motor and sensitive nerve damage (better functional recovery with below-the-knee amputation and prosthetic rehabilitation)
-
Severe, multiple lower limb joint compromise (better functional recovery with below-the-knee amputation and prosthesis rehabilitation)
-
Severe bilateral lower limb fractures (no safe donor area available)
-
Total amputations in which the segment may be reimplanted first and, if shortened, only then subsequently lengthened
-
Clinical Case 1. Preoperative radiograph of the traumatized leg. A multiple segmental and exposed spiral fracture of the tibia is identified (Gustilo stage 3c).
-
Clinical Case 1. Radiograph of the reduced fracture. Anteroposterior radiograph of the fractured leg after reduction and immobilization with an external fixation device. Pseudoarthrosis of the tibia.
-
Clinical Case 1. Early postoperative view of the emergency management of a middle-third tibial fracture. Reduction of the fracture and skin grafting to the defect.
-
Clinical Case 1. Radiologic evidence of the pseudoarthrosis. Laterolateral radiograph of tibial pseudoarthrosis that shows bone nonunion and anterior bowing.
-
Clinical Case 1. Preoperative picture. Lateral view of the left leg, which now has pseudoarthrosis with anterior bowing of the tibia at its middle third.
-
Clinical Case 1. Preoperative drawing. Schematic drawing of the preoperative defect and of the planned contralateral flap.
-
Clinical Case 1. Preoperative view of the donor leg with schematic drawing of the osteocutaneous peroneal flap.
-
Clinical Case 1. Postoperative drawing. Schematic drawing of the postoperative desired outcome at the recipient and donor areas.
-
Clinical Case 1. Intraoperative picture. The osteocutaneous peroneal flap synthesized to the recipient site, with its skin island.
-
Clinical Case 1. Early postoperative radiograph of the operated leg in anteroposterior view. The peroneal flap is easily identified after being infibulated into tibial stumps.
-
Clinical Case 1. Postoperative picture. Lateral view of the left leg 1 month after surgery.
-
Clinical Case 1. Postoperative radiograph (1 mo) of the leg. Anteroposterior radiograph of the tibia, which shows satisfactory bone alignment and healing 1 month after surgery.
-
Clinical Case 2. Preoperative picture. Medial view of the left leg with exposed fracture of the inferior third of the tibia (Gustilo stage 3c) and loss of skin cover.
-
Clinical Case 2. Preoperative picture. Lateral view of the left leg with exposed fracture of the inferior third of the tibia (Gustilo stage 3c).
-
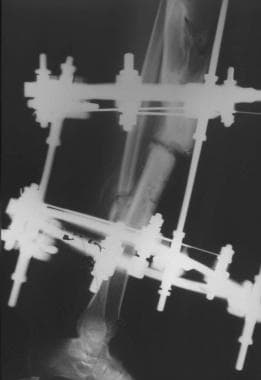
Clinical Case 2. Preoperative radiograph of the traumatized leg after early debridement and immobilization with external fixation. Shown is a double complete fracture of the tibia and fibula at their inferior third with loss of substance (Gustilo stage 3c).
-
Clinical Case 2. Preoperative drawing. Schematic drawing of the preoperative bone defect and the planned contralateral flap.
-
Clinical Case 2. Early postoperative radiograph of the operated leg in anteroposterior view. The peroneal flap is easily identified after being infibulated into tibial stumps.
-
Clinical Case 2. Postoperative picture. Postoperative result in anteroposterior view.
-
Clinical Case 2. Late postoperative radiograph. Anteroposterior radiograph of the tibia 6 months after surgery, with a satisfactory bone alignment and union.
-
Clinical Case 2. Postoperative picture. Medial view of postoperative result.
-
Clinical Case 2. Preoperative picture. Frontal view of the right leg with a wide defect of the superior third of the tibia resulting from segmental exposed fracture (Gustilo stage 3c).
-
Clinical Case 3. Preoperative radiograph of the traumatized leg after early debridement and immobilization with external and internal synthesis. A displaced spiral fracture of the superior third of the tibia with loss of bone tissue is evident (Gustilo stage 3c).
-
Clinical Case 3. Preoperative drawing. Schematic drawing of the preoperative bone defect and the planned contralateral flap.
-
Clinical Case 3. Preoperative view of the left donor leg with schematic drawing of the osteocutaneous peroneal flap.
-
Clinical Case 3. Intraoperative picture of the flap. Intraoperative view of the harvested peroneal osteocutaneous flap.
-
Clinical Case 3. Postoperative drawing. Schematic drawing of the desired postoperative outcome at the recipient and donor areas.
-
Clinical Case 3. Postoperative radiograph of the operated leg in anteroposterior view. The peroneal flap is easily identified after being infibulated into tibial stumps.
-
Clinical Case 3. Anteroposterior radiograph of the tibia 6 months after surgery, with a satisfactory bone alignment and union.
-
Clinical Case 3. Postoperative result in anteroposterior view with the leg bearing full body weight.
-
Clinical Case 4. Osteomyelitis of the middle third of the tibial shaft. Shown is a long-standing osteocutaneous fistula secreting pus.
-
Clinical Case 4. Preoperative planning. Drawing of a right rectus abdominis muscle flap based on the inferior epigastric pedicle.
-
Clinical Case 4. Intraoperative picture. The right rectus abdominis flap isolated on its vascular pedicle.
-
Clinical Case 4. Postoperative result. Oblique view of the perfectly healed rectus abdominis muscle flap transferred in place and covered by a meshed split-thickness skin graft.
-
Fracture of the tibial plate and fibular head.
-
Early postoperative radiograph after fixation of the tibial fractures with a plate.
-
Infection and exposure of the plate through the surgical access site.
-
Posterior approach to the lateral head of the gastrocnemius.
-
The lateral head of the gastrocnemius is dissected and pedunculated proximally on the lateral sural artery. The soleus muscle is visible at the donor site.
-
The lateral head of the gastrocnemius is transferred anteriorly, by lateral rotation under the skin, to cover the plate and the fracture lines.
-
Meshed split-thickness skin graft is applied to the exposed row surface of the gastrocnemius.
-
Drawing of the reverse sural fasciocutaneous flap, vascularized from distal peroneal perforators.
-
Skin marking of a large reverse sural flap.
-
Incision is carried out through the skin down to the muscle fascia, to include the fascia of the leg into the flap.
-
Frontal view of large scarred area of the leg undergoing frequent breakdowns, with possible malignant transformation.
-
Medial view of the scarred area of the leg.
-
Lateral view of the scarred area of the leg. Perforators from the peroneal artery are identified along the lateral septum of the leg with the aid of a superficial Doppler probe.
-
Frontal view of postoperative results of the scarred area replaced by the reverse sural fasciocutaneous flap.
-
Postoperative medial view showing the proximal tip of the flap.
-
Postoperative lateral view showing the distal narrow pedicle of the flap.
-
Donor area of the reverse sural flap repaired with a meshed split-thickness skin graft.













