Background
Orthognathic surgery involves the surgical manipulation of the elements of the facial skeleton to restore the proper anatomic and functional relationship in patients with dentofacial skeletal anomalies. [1, 2]
This article provides an overview of the principles used in orthognathic surgery, which can be used to manage a broad spectrum of maxillofacial abnormalities, including congenital, developmental, and acquired deformities.
History of the Procedure
While an exhaustive history is not possible, a brief chronologic history of orthognathic procedures follows.
Mandibular osteotomies
1846 - Hullihan - Anterior mandibular subapical osteotomy and setback
1906 - Blair - Mandibular body osteotomy
1907 - Blair - Horizontal osteotomy of the ramus, external approach
1925 - Limberg - Posterior oblique vertical ramal osteotomy, external approach
1927 - Wassmund - Inverted "L" ramal osteotomy, external approach
1939 - Kazanjian - Beveled horizontal osteotomy of the ramus, extraoral approach
1942 - Schuchardt - Step horizontal osteotomy of the ramus, intraoral approach
1954 - Caldwell and Letterman - Vertical ramal osteotomy, external approach
1955 - Obwegeser - Sagittal split ramal osteotomy
1968 - Caldwell et al - "C" ramal osteotomy
1970 - Hebert, Kent, and Hinds - Intraoral vertical ramal osteotomy
Maxillary osteotomies
1927 - Wassmund - Le Fort I osteotomy with the pterygomaxillary junction left intact; elastic forces used to bring the maxilla forward
1928 - Axhuasen - Segmental osteotomy through the mid palate
1942 - Schuchard - Staged Le Fort I osteotomy, followed by pterygomaxillary separation; external traction used to bring the maxilla forward
1949 - Moore and Ward - Horizontal transection of the pterygoid plate
1965 - Obwegeser - Fully mobilized the maxilla; in a single step brought it into the predicted position
Osseous genioplasty procedures
1942 - Hofer - Horizontal sliding osteotomy of a receding chin (extraoral)
1957 - Trauner and Obwegeser - Intraoral approach to osseous genioplasty [3]
Historically, the ability to reposition the mandible in a stable manner long preceded the ability to reposition the maxilla. As a consequence, many patients underwent only mandibular surgery to correct a primary maxillary deformity. The specialty of orthognathic surgery did not fully develop until Obwegeser demonstrated the possibility of repositioning the maxilla in a stable consistent manner in 1965 and reported simultaneous repositioning of the maxilla and mandible in 1970.
Problem
The word orthognathic comes from the Greek word orqos, meaning to straighten, and gnaqos, meaning jaw. Orthognathic surgery thus means to straighten a jaw. Defining a straight jaw versus one that is not requires determining the degree of deviation from a specified population norm. Nevertheless, restoring the orthognathic form of the face ultimately depends upon achieving the ideal facial esthetics of the individual patient, not simply restoring the average normative values of a population.
Remember that the face is more than the upper and lower jaw; when deformities extend to involve the cranio-orbital skeleton, evaluation and management expand the scope of maxillofacial surgery to craniofacial surgery. Thus, orthognathic or maxillofacial surgery is a subset of craniofacial surgery.
Correction of maxillofacial deformities requires careful analysis of the soft tissue with clinical examination and supporting photographs, skeletal evaluation with standardized radiographs, and dental evaluation with study dental casts. Formulation of a treatment plan thus requires close cooperation of the surgeon working with the dentist, the orthodontist, and at times the restorative prosthodontist. Unlike many surgical procedures, outcome depends not only on the surgical procedure but also on a multitude of factors that begin long before the actual surgery as well as on control of the variables long after surgery.
Epidemiology
Frequency
The exact incidence of dentofacial deformities requiring orthognathic surgery is difficult to estimate because it includes a broad population of patients with deformities of congenital, developmental, and traumatic origin. However, the number of individuals with developmental dentofacial deformities in the United States who may benefit from orthognathic surgery is estimated at 1.5–2 million; of these, approximately 1 million present with Class II deformities and 0.5 million with Class III deformities. In other regions of the world, the distribution among these classes seems to vary.
Etiology
Dentofacial skeletal anomalies generally occur as a result of a differential in growth of the upper facial skeleton to the lower facial skeleton, resulting in discrepancy of the normal relationship that exists between the upper and lower jaw. Underlying genetic predisposition and acquired causes can influence the normal growth of the facial skeleton. Congenital anomalies, from syndromic conditions such as Apert and Crouzon syndromes to facial clefts, affect normal growth and development.
Traumatic events in the mature skeleton can displace the normal elements and require repositioning osteotomies if improperly reduced initially. Traumatic events in the developing facial skeleton can disturb normal subsequent growth. Other etiologies that can result in significant dentofacial anomalies include neoplastic growth, surgical resection, and iatrogenic radiation. However, of all the etiologies, developmental anomalies representing the extremes of population norms are the most common conditions requiring orthognathic surgery.
Presentation
A wide range of clinical presentations is possible, some of which are outlined in the table below. Diagnosis is based on a comprehensive assessment that includes clinical examination, skeletal evaluation with standardized radiographs, and dental evaluation with study dental casts addressed as an integral part of the workup.
See the image below.
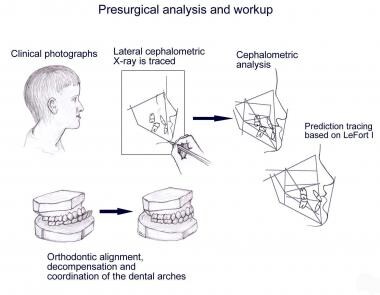 An overview of the clinical, radiographic, and dental evaluation used in planning orthognathic surgery.
An overview of the clinical, radiographic, and dental evaluation used in planning orthognathic surgery.
Clinical assessment should be directed specifically at evaluating the relative position and size of each of the facial skeletal elements, the degree of zygomatic projection, and the maxillary and mandibular positions in space relative to each other and to the cranial-orbital region. The nasolabial angle, upper lip length, lip competency, labial-mental sulcus, and cervicomental angle should be documented. Any facial asymmetry should be noted along with the relationship of the maxillary dental mid line to the mandibular dental mid line and the dental mid lines to the facial mid line. The intraoral examination should focus on the dental alignment within each arch and relationship of the dental arches to each other. The degree of dental display on repose and smile also should be recorded with the amount of gingival display.
Facial balance typically is assessed by dividing the face in thirds. The upper third is from the anterior hairline (trichion) to the glabella, the middle third from the glabella to the subnasale, and the lower third from the subnasale to the menton. When each of the thirds is equal, the face is said to be balanced and of "ideal" proportions. The lower third may be further divided into an upper third (subnasale to oral commissure) and a lower two thirds (oral commissure to menton). Additionally, in profile view the face should have a slight degree of convexity as measured from the glabella to the subnasale to the menton.
See the image below.
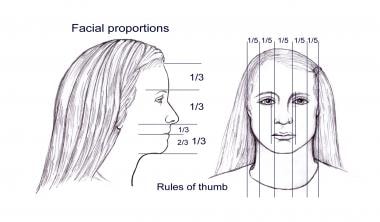 Ideal facial proportions believed to be in aesthetic balance. Such proportions are only guidelines, as ideal proportions change over time, and the ideal result varies with patient expectations.
Ideal facial proportions believed to be in aesthetic balance. Such proportions are only guidelines, as ideal proportions change over time, and the ideal result varies with patient expectations.
Excess facial convexity, flatness, or concavity is felt to be less than ideal. However, facial proportions are only idealized concepts and have changed over time. They merely provide a guideline that is not true for every patient; a wide range of aesthetic faces defies such absolute canons.
See the image below.
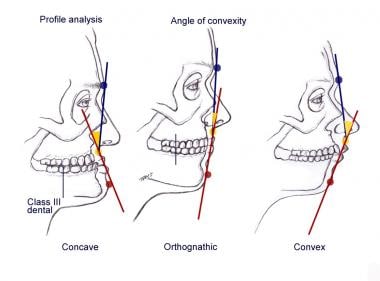 Profile analysis illustrating the degree of facial convexity or concavity from an acceptable orthognathic norm.
Profile analysis illustrating the degree of facial convexity or concavity from an acceptable orthognathic norm.
Maxillofacial deformities can be divided broadly into 3 major categories: (1) dental dysplasias, (2) skeletal dysplasias, and (3) dentoskeletal dysplasias.
Dental dysplasias
Dental dysplasias are limited strictly to malocclusions that result from abnormal spatial relationship of the dentition and not from the skeletal position of the upper and lower jaws. These can be corrected with orthodontic treatment.
Skeletal dysplasias
In patients with skeletal dysplasia only, the dentition is in good alignment, but the maxilla and/or mandible are dysplastic. Skeletal dysplasias require correcting the skeletal deformity without altering the occlusion. An example is a patient with retrogenia without retrognathia or a patient with hemifacial microsomia who has a normal maxillary-mandibular dental relationship but has an occlusal cant because of skeletal asymmetry.
Dentoskeletal dysplasias
In dentoskeletal dysplasias, the dentition is malpositioned within each arch and with each other; additionally, the skeletal relationship of the upper and lower jaws is abnormal. An example is a patient with a maxillary sagittal and transverse width deficiency from a facial cleft. Correction requires aligning the dentition within each arch with orthodontic treatment and restoring the maxillary-mandibular dental relationship with skeletal osteotomies and repositioning. In addition, dentoskeletal dysplasias can be classified further based on the position in space and on the volume or mass (whether deficient or in excess) of the individual elements. For example, the mandible can be of normal shape and volume but retrognathic in relationship to the maxilla, or it may be both retrognathic and volumetrically deficient.
Table. Typical Presentation of Maxillofacial Deformities (Open Table in a new window)
Deformity |
Clinical Features |
Skeletal Assessment |
Dental Assessment |
Maxilla: Sagittal deficiency |
Concave facial profile Retrusive upper lip Acute nasolabial angle Alar base narrow Lack of dental display |
SNA* decreased SNB† normal ANB‡ decreased |
Class III Maxillary dental crowding Maxillary incisors proclined Mandibular incisors normal or retroclined |
Maxilla: Sagittal excess |
Convex facial profile Obtuse nasolabial angle |
SNA increased SNB normal ANB increased |
-- |
Maxilla: Vertical excess (long face syndrome) |
Convex profile Lower facial height increased Alar base constricted Nasolabial angle obtuse Excessive incisor show Excessive gingival show Lip incompetence Mentalis strain with lip closure Chin vertically long, retruded |
Lower FH§ increased SNA decreased SNB decreased ANB increased Mandibular plane angle steep Palatal-occlusal plane increased |
Class II, Class I Anterior open bite Maxillary arch constricted Curve of Spee, flat-accentuated Dental crowding |
Maxilla: Vertical deficiency (short face syndrome) |
Concave facial profile Lower facial height decreased Acute nasolabial angle Alar base widened Lack of incisor show Edentulous appearance Chin protruded |
Lower FH decreased SNB increased ANB negative Palatal-occlusal plane decreased Mandibular plane angle acute |
Class II, Class I Deep bite Crowding Mandibular dentition Curve of Spee reverse |
Mandible: Deficiency |
Convex profile Retruded chin Everted lower lip Deep labiomental crease Mentalis strain with lip closure |
SNA normal SNB decreased ANB increased Ar-Gn¶ decreased |
Class II Mandibular incisors proclined Maxillary incisors retroclined Curve of Spee accentuated |
Mandible: Excess |
Concave profile Midface appears deficient Lower third broad Lower lip thin |
SNA normal SNB decreased ANB decreased |
Class II Maxillary incisors proclined Mandibular incisors retroclined |
* SNA = Sella-nasion-A point angle
† SNB = Sella-nasion-B point angle
‡ ANB = A point-nasion-B point angle
§ FH = Frankfort horizontal
¶ Ar-Gn = Articulare-gnathion
Indications
Indications for orthognathic surgery include facial dysmorphism with and without functional implications. As an illustration, an osseous genioplasty for a patient with retrogenia but without malocclusion should be considered for facial form. If the retrogenia is associated with retrognathism resulting in a malocclusion, orthognathic surgery is indicated for restoring the facial form and for functional occlusion. Airway and speech are other indications when considering the functional need for orthognathic surgery. Restoration of the normal anatomic relationship between the maxilla and mandible relative to the cranial base reestablishes the functional components (ie, form and function) of the facial skeleton.
Relevant Anatomy
As relevant skeletal and neurovascular anatomy can be found in many anatomic atlases, this section focuses on specific aspects pertinent to the procedures described.
With maxillary osteotomies, an understanding of the vascular blood supply to the mobilized maxilla is crucial. The arterial blood supply to the maxilla is derived from 4 primary sources: (1) the descending palatine branch of the maxillary artery, (2) the ascending palatine branch of the facial artery, (3) the anterior branch of the ascending pharyngeal artery from the external carotid, and (4) the alveolar branches of the maxillary artery. With complete mobilization of the maxilla, frequently the descending palatine vessels are disrupted and the mobilized maxilla derives its vascularity from the remaining sources, primarily the ascending palatine and pharyngeal vessels.
To avoid neurosensory deficits with mandibular osteotomies, the surgeon must be cognizant of the course of the inferior alveolar nerve from its entrance at the mandibular foramen on the medial aspect of the ramus to its emergence from the mental foramen between the first and second premolars. Vertically, the mandibular foramen typically lies approximately 8 mm inferior to the lingula mandibularis (the anterior wall of the mandibular foramen), and the lingula is approximately 5 mm above the occlusal plane. With the sigmoid notch as a reference point, the foramen is approximately 20 mm inferior. Regarding the anterior-to-posterior relationship, the foramen is located 20 mm from the anterior mandibular ramal border, a depth of approximately two thirds of the total mandibular ramal width.
The canal then courses within the mandible, measuring 2-2.5 mm in diameter. Its lowest point from the inferior mandibular border is in the region of the first and second molars, approximately 7.5 mm, before continuing anterior and superior to its emergence from the mental foramen, where it is approximately 8 mm from the inferior border. At the mental foramen, the canal extends caudally before emerging. Regarding the transverse position of the canal within the mandible, it is most superficial in the region of the third molar, approximately 2 mm from the buccal plate. In the region of the first molar, it is 4 mm from the buccal plate.
A number of basic dental concepts pertinent to orthognathic surgical procedures are important.
Dental notation
Universal Dental Notation is the most common system for numerically identifying permanent dentition. The maxillary dentition is numbered sequentially from 1-16 starting with the right maxillary third molar as 1. The numbering system continues from 17-32 beginning with the left mandibular third molar as 17.
Orientation terms
Orientation with respect to intraoral anatomy is referenced to the following terms:
-
Mesial - Toward the dental mid line
-
Distal - Away from the dental mid line
-
Labial - Toward the lips
-
Buccal - Toward the cheek
-
Apex - Toward the root tip
-
Lingual - Toward the tongue
-
Incisal - Toward the biting surface (anterior dentition)
-
Occlusal - Toward the biting surface (posterior dentition)
-
Angulation - Mesiodistal tipping of the long axis of the tooth
-
Inclination - Labiolingual or buccolingual tipping of the long axis of the tooth
Dental anatomic terms
See the list below:
-
Cusp - Pronounced elevation on the occlusal surface
-
Groove - Depression on the occlusal surface
-
Crown - Visible portion of the tooth covered by enamel
-
Cingulum - Bulbous convexity of the cervical one third of the lingual surface of anterior dentition
-
Cervix (neck) - Junction of the crown and root
-
Root - Portion of the tooth covered by cementum within the alveolar bone
-
Curvature of the dental arches - Normal reciprocal curvature in the dental arches with the maxilla convex and the mandible concave (allows the dentition maximal contact during function)
-
Curve of Spee - Normal curvature of the dental arch in the sagittal plane
-
Curve of Wilson - Normal curvature of the dental arch in the coronal plane
Occlusal classification
The classification of dental occlusions is based on Edward Angle's observation in 1899 that the key to occlusion is the relationship of the mandibular first molar to the maxillary first molar. [4]
-
Angle Class I (neutro-occlusion): The mesiobuccal cusp of the maxillary first molar articulates within the mesiobuccal groove of the mandibular first molar.
-
Angle Class II (disto-occlusion): The mandibular first molar articulates distal to the mesiobuccal cusp of the maxillary first molar. [5]
-
Angle Class III (mesio-occlusion): The mesiobuccal groove of the mandibular first molar is mesial to the mesiobuccal cusp of the maxillary first molar. [6]
Angle's original classification has been expanded to include the anterior dentition. Class II is subdivided further to include the angulation of the anterior dentition. In Class II, Division 1, the molar relationship is Class II, but the maxillary anterior teeth are flared labial. In Class II, Division 2, the molar relationship is Class II, but both the maxillary and mandibular anterior teeth are retruded with a deep bite. The terms Class I, II, and III also are used to relate the maxillary and mandibular canine relation.
The Angle classification relates only to maxillary dentition with the mandibular dentition. While it generally is assumed that a similar skeletal relationship of Class I, II, and III follows, this is not always the situation. A Class I molar relationship is possible with a Class II skeletal relationship by dental extractions and orthodontic alignment without regard to basal skeletal morphology.
Upper and lower arch dentition
Additional terms are used to describe the relationship between the dentition of the upper and lower arches.
-
Overjet - Horizontal distance between the incisal edges of the maxillary incisor to the mandibular incisor
-
Overbite - Vertical distance between the incisal edge of the maxillary incisor and the mandibular incisor
-
Crossbite - Lingual-buccal malposition of the normal relationship between the upper and lower dentition (negative overjet)
-
Deep bite - Condition of excessive overbite
-
Open bite - Condition of negative overbite (teeth do not meet)
Dental compensations
The anterior dentition typically inclines so as to partly offset the malocclusion and may allow some degree of anterior occlusion to occur depending on the maxillary-mandibular discrepancy. In prognathism, the lower incisors may be flared lingual and the upper incisors flared labial to compensate for the Class III malocclusion. Conversely, with mandibular deficiency the opposite occurs; the mandibular dentition is flared labial and the maxillary dentition flared lingual.
Centric relation and centric occlusion
Centric relation is the most retruded position of the condyle within the glenoid fossa (terminal hinge position). It refers to the condylar-glenoid fossa relation but does not indicate the occlusion. Centric occlusion indicates the maximum intercuspal contact of the dentition and does not refer to the condylar position. In the ideal situation, when the patient is in centric occlusion (maximum), the condylar-glenoid is in proper centric relation.
Contraindications
Numerous risk factors may alter the treatment plan or preclude surgery, including underlying medical conditions, bleeding dyscrasias, systemic disease or local factors that may affect normal wound healing, compromised vascularity of the surgical region, a patient with unrealistic expectations, a noncompliant patient, and patients with poor oral hygiene.
-
Ideal facial proportions believed to be in aesthetic balance. Such proportions are only guidelines, as ideal proportions change over time, and the ideal result varies with patient expectations.
-
Profile analysis illustrating the degree of facial convexity or concavity from an acceptable orthognathic norm.
-
An overview of the clinical, radiographic, and dental evaluation used in planning orthognathic surgery.
-
Analysis of the dentofacial skeleton is based on identifiable radiographic landmarks on a lateral cephalometric x-ray.
-
Lateral cephalometric analysis of the facial skeleton based on Steiner analysis. The positions of the maxilla and mandible each are related spatially to the anterior cranial base and to each other. Note that normative values of the facial elements depend on a normal anterior cranial base inclination and length, which typically are altered in craniofacial conditions.
-
Lateral cephalometric analysis of the dentition within the skeletal framework.
-
Illustration of 2-dimensional (2D) versus 3-dimensional (3D) planning for orthognathic surgery. All images are of the same patient (with maxillary deficiency and mandibular prognathism). Unlike conventional 2D cephalometric analysis and treatment planning, 3DCT-based analysis provides a more accurate simulation of the surgery and affords analysis in all 3 planes. Note that in the upper images, the osteotomies have been made (left) and then the maxillary and mandibular segments have been moved (right).
-
Illustration of the role of presurgical dental decompensation in a patient requiring mandibular advancement. Dental decompensation is necessary to allow for proper degree of mandibular advancement and for postsurgical stability at the occlusal level. Note that the occlusion is made worse until corrected by skeletal advancement.
-
Presurgical orthodontic management requires appropriate dental decompensation, alignment of the dentition within the individual arches, leveling of the curve of Spee, and coordination of the maxillary and mandibular dentition for postoperative stability.
-
Illustration of the transverse maxillary Le Fort I osteotomy. The osteotomy is made with a reciprocating saw and completed at the pterygopalatine junction with a curved osteotome.
-
Variation of midfacial osteotomies to correct differing degrees of midfacial deformities involving the zygoma.
-
Illustration of the sagittal split ramal osteotomy. Place the horizontal osteotomy superior to the inferior alveolar nerve foramen and continue partially through the body along the oblique line to the region of the second and first molar to complete the vertical osteotomy. Make the osteotomy through the cortex with a reciprocating saw and complete it with an osteotome along the buccal surface.
-
Illustration of mandibular excess. The patient underwent bilateral sagittal split ramal osteotomy and mandibular setback.
-
Illustration of mandibular deficiency. The patient underwent bilateral sagittal split ramal osteotomy and advancement.
-
Illustration of maxillary deficiency with relative mandibular excess. The patient underwent a modified Le Fort I midfacial advancement that included the body of the zygoma.
-
Illustration of vertical maxillary excess, apertognathia, and mandibular retrognathia. The patient underwent Le Fort I anterior-posterior differential maxillary impaction with sagittal split ramal osteotomy and mandibular advancement.





