Practice Essentials
The presence of unilateral cleft lip is one of the most common congenital deformities. A broad spectrum of variations in clinical presentation exists. Unilateral cleft lip involves deformity of the lip in addition to the alveolus and nose. Patients with this deformity require short-term care and long-term care and follow-up from practitioners in multiple specialties. [1] Patients may need multiple surgical interventions, from infancy to adulthood, in order to achieve necessary function and aesthetic quality. [2]
No universal agreement has been reached as to the timing and technique of repair. Several methods are used with comparable long-term results, which serves as an indication that more than one treatment option exists for definitive repair. Treatment goals include the restoration of facial appearance and oral function, improvement of dental skeletal and occlusal relationships, improvement of speech, and the psychosocial state.
Workup in patients with unilateral cleft lip
Perform a thorough physical examination, not limited to the head and neck region, to uncover associated anomalies in the infant presenting with a unilateral cleft lip with or without a palatal cleft. Additional workup is determined by physical findings that suggest involvement of other organ systems.
Management of patients with unilateral cleft lip
Children born with a facial cleft benefit from multidisciplinary clinical care. This is a team-based approach allowing efficient coordination of all aspects of care. Beyond the lip repair are other issues such as hearing, speech, dental, and psychosocial integration. With the multidisciplinary approach, as the child grows, comprehensive care can be given from birth through adolescence.
The optimal timing of the surgical repair is still somewhat controversial. Some centers have advocated surgery in the early neonatal period, with a theoretical benefit in the scar appearance and nasal cartilage adaptability, thus minimizing the nasal deformity. To minimize anesthetic risks, some still adhere to the rule of 10s: perform surgical repair of cleft lip when the child has a hemoglobin of 10 g and a weight of 10 lb and is aged 10 weeks. In general, however, most centers prefer to perform the unilateral lip repair when the infant is aged 2-4 months; anesthesia risks are lower, the child is better able to withstand the stress of surgery, and lip elements are larger and allow for a meticulous reconstruction.
A number of surgical procedures for the repair of a unilateral cleft lip are well described, with a multitude of variations, including the LeMesurier quadrilateral flap repair, Randall-Tennison triangular flap repair, Millard rotation-advancement repair, [3, 4] and Skoog and Kernahan-Bauer upper and lower lip Z-plasty repairs. Many other variations exist; of particular note are the repairs by Delaire and by Poole.
History of the Procedure
In 1843, closure of the unilateral cleft lip with local flaps was described by Malgaigne. The following year, Mirault modified Malgaigne’s technique by using the lateral lip flap to fill the medial defect. All future methods of cleft lip closure are based on Mirault’s technique. LeMesurier and Tennyson modified this technique with a quadrilateral and triangular flap, respectively. In 1976, Millard published his definitive repair in which the lateral flap advancement into the upper portion of lip was combined with downward rotation of medial lip. [5] Other modifications have been published by Noordhoff, Mohler, and Onizuka. [6, 7] Fisher has described an anatomical subunit approximation for definitive cleft lip repair. Millard’s methods, including variations, remain among the most popular method for unilateral cleft lip closure. [7]
Cleft lip surgery has evolved from a simple adhesion of paired margins of the cleft to an understanding of the various malpositioned elements of the lip to a more complicated geometric reconstruction using transposition, rotation, and advancement flaps. [8]
Problem
The cleft affects the facial form as an anatomic deformity and has functional consequences. These include the child's ability to eat, speak, hear, and breathe. Consequently, rehabilitation of a child born with a facial cleft must involve a multidisciplinary approach and staged appropriately with the child's development, balancing the timing of intervention against its effect on subsequent normal growth.
Epidemiology
Frequency
The overall occurrence of cleft lip with or without cleft palate is approximately 1 in 750-1000 live births. Racial differences exist, with the incidence in Asians (1:500) being greater than in Caucasians (1:750), which is greater than in African Americans (1:2000). The incidence of cleft lip/palate is more common in males.
The most common presentation is cleft lip and palate (approximately 45%), followed by cleft palate alone (35%) and cleft lip alone (approximately 20%). Unilateral cleft lips are more common than bilateral cleft lips and occur more commonly on the left side (left cleft lip:right cleft lip:bilateral cleft lip = 6:3:1).
The risk of a newborn having a cleft lip increases if a first-degree relative also has a cleft. If one child already has a cleft lip, the chance of a second child being born with the deformity is 4%. If a parent has a cleft lip, the chance of a newborn having a cleft is 7%. If both a parent and a sibling have a cleft lip, the newborn's risk rises to 15%.
Etiology
Clefting has a multifactorial basis, with both genetic and environmental causes cited. The observation of clustered cases of facial clefts in a particular family indicates a genetic basis. Clefting of the lip and/or palate is associated with more than 150 syndromes. The overall incidence of associated anomalies (eg, cardiac) is approximately 30% (more common with isolated cleft palate).
Environmental causes, such as viral infection (eg, rubella) and teratogens (eg, steroids, anticonvulsants), during the first trimester have been linked to facial clefts. The risk also increases with parental age, especially when older than 30 years, with the father's age appearing to be a more significant factor than the mother's age. Nevertheless, most presentations are of isolated patients within the family without an obvious etiology.
Midfacial development involves several sets of genes, including those involved in cell patterning, proliferation, and signaling. Mutations in any of these genes can change the developmental process and contribute to cleft development. Some of these genes include the DIX gene, sonic hedgehog (SHH) gene, transforming growth factor (TGF) alpha/beta, and interferon regulatory factor (IRF6).
Classification
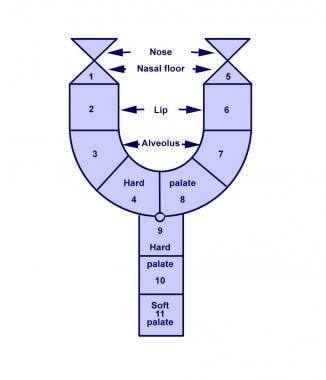
Kernahan developed a classification scheme in which the defect can be classified onto a Y-shaped symbol. In this diagram, the incisive foramen is represented as the focal point. This system has been applied to both cleft lip and palate.
Pathophysiology
While the normal embryologic development of the face is detailed in Head and Neck Embryology, a brief outline relevant to the formation of facial clefts follows.
In short, the branchial arches are responsible for the formation of several areas, including the mouth and lip. Mesenchymal migration and fusion occurs during weeks 4-7 of gestation. The first branchial arch is responsible for the formation of the maxillary and mandibular processes. The maxillary and mandibular prominences form the lateral borders of the primitive mouth or stomodeum.
Mesenchymal migration and fusion of the primitive somite-derived facial elements (central frontonasal, 2 lateral maxillary, mandibular processes), at 4-7 weeks gestation, is necessary for the normal development of embryonic facial structures. When migration and fusion are interrupted for any reason, a facial cleft develops along embryonic fusion lines. The embryonic development of the primary palate (lip and palate anterior to the incisive foramen) differs from the secondary palate (palate posterior to the incisive foramen).
The developing processes of the medial nasal prominence, lateral nasal prominence, and maxillary prominences form the primary palate. Fusion occurs, followed by "streaming" of mesodermal elements derived from the neural crest. In contrast, the secondary palate is formed by the fusion of palatal processes of the maxillary prominence alone. The difference in embryonic development suggests the possibility of differing degrees of susceptibility to genetic and environmental influences and accounts for the observed variation in incidences.
In summary, unilateral cleft lip results from failure of fusion of the medial nasal prominence with the maxillary prominence.
Presentation
For treatment purposes, unilateral cleft lip can be placed into one of three categories: microform/forme fruste, incomplete, or complete cleft lip.
-
Microform cleft (forme fruste): This defect is characterized by a "light" furrow along the vertical length of the lip with a small vermilion notch and minor imperfections in the white roll. A small component of vertical lip length deficiency and associated nasal deformity may be present.
-
Incomplete cleft lip: This defect is characterized by the varying degree of vertical lip separation. By definition, it has an intact nasal sill, commonly termed the Simonart band.
-
Complete cleft lip: This involves the full-thickness defect of the lip and alveolus (primary palate), extends into the base of the nose (no Simonart band exists), and is often accompanied by a palatal cleft (secondary palate). The premaxilla is typically rotated outward and projects anteriorly in relation to a relatively retropositioned lateral maxillary alveolar element. [9]
As a consequence of the clefting of the lip, an associated nasal deformity occurs. The structures of the ala base, nasal sill, vomer, and septum are distorted significantly. The lower lateral cartilage on the cleft side is positioned inferiorly, with an obtuse angle as it flattens across the cleft. The alar base is rotated outward. The developing nasal septum pulls the premaxilla away from the cleft, and the septum and the nasal spine are deflected toward the noncleft side. The cleft may continue through the maxillary alveolus and palatal shelf, extending to the palatal bone and soft palate.
A study by Buyuk et al found that patients with unilateral cleft lip and palate had a higher rate of dehiscence around the anterior maxillary teeth on the cleft and noncleft sides of the mouth than did normal controls. The study also found that the rate of fenestrations around these teeth was higher on the cleft side of patients than in controls. [10]
Further treatment planning
Orthodontic treatment can be initiated a few weeks following birth, prior to surgical intervention. Other adjunct procedures include lip adhesion, presurgical orthopedics, primary nasal correction, and nasoalveolar molding (NAM). These procedures attempt to reduce the deformity. NAM is the active molding and repositioning of the nasal cartilage and alveolar processes with an appliance. [11, 12] This orthodontic intervention takes advantage of the plasticity of the cartilage. Presurgical nasal alveolar allows repositioning of the maxillary alveolus and surrounding soft tissues in hopes of reducing wound tension and improving results. [13, 14]
Definitive repair is delayed until approximately 3 months of age; this varies, depending on physician comfort. A multidisciplinary approach should be carried out over several years for patients with unilateral cleft lip. This team should include practitioners from audiology, otolaryngology, and speech therapy, among other specialities.
Indications
Patients born with a cleft lip should undergo surgical repair unless otherwise contraindicated. The goal of reconstruction is to establish normal morphologic facial form and function in order to provide the optimal conditions for the development of dentition, mastication, hearing, speech, and breathing, and psychosocial status.
Relevant Anatomy
Normal lip and nasal anatomy is essential for an understanding of the distortion caused by a facial cleft. The elements of the normal lip are composed of the central philtrum, demarcated laterally by the philtral columns and inferiorly by the Cupid's bow and tubercle. Just above the junction of the vermilion-cutaneous border is a mucocutaneous ridge frequently referred to as the white roll. Within the red vermilion of the lip is a noticeable junction demarcating the dry and wet vermilion, the increased keratinized portion of the lip that is exposed to air from the moist environment of the labial mucosa.
The primary muscle of the lip is the orbicularis oris, and it has two well-defined components: the deep (internal) and the superficial (external) components. The deep (internal) fibers run horizontally or circumferentially from commissure (modiolus) to commissure (modiolus) and functions as the primary sphincteric action for oral feeding. The superficial (external) fibers run obliquely, interdigitating with the other muscles of facial expression to terminate in the dermis. They provide subtle shades of expression and precise movements of the lip for speech.
The superficial fibers of the orbicularis decussate in the midline and insert into the skin lateral to the opposite philtral groove forming the philtral columns. The resulting philtral dimple centrally is depressed as there are no muscle fibers that directly insert into the dermis in the midline. The tubercle of the lip is shaped by the pars marginalis, the portion of the orbicularis along the vermilion forming the tubercle of the lip with eversion of the muscle.
In the upper lip, the levator labii superioris contributes to the form of the lip. Its fibers, arising from the medial aspect of the infraorbital rim, sweep down to insert near the vermilion cutaneous junction. The medial-most fibers of the levator labii superioris sweep down to insert near the corner of the ipsilateral philtral column and vermilion-cutaneous junction, helping to define the lower philtral column and the peak of the Cupid's bow.
The nasal muscles are equally important. The levator superioris alaeque arises along the frontal process of the maxilla and courses inferiorly to insert on the mucosal surface of the lip and ala. The transverse nasalis arises along the nasal dorsum and sweeps around the ala to insert along the nasal sill from lateral to medial into the incisal crest and anterior nasal spine. These fibers join with the oblique fibers of the orbicularis and the depressor septi (nasalis), which arises from the alveolus between the central and lateral incisors to insert into the skin of the columellar to the nasal tip and the footplates of the medial crura.
A unilateral cleft thus disrupts the normal termination of the muscle fibers that cross the embryologic fault line of the maxillary and nasal processes, resulting in symmetric but abnormal muscular forces between the normal equilibrium that exists with the nasolabial and oral groups of muscles. With an unrestrained premaxilla, the deformity accentuates with differential growth of the various elements. The alar cartilages are splayed apart and rotate caudally, subluxed from the normal position. Consequently, the nasal tip broadens, the columellar is foreshortened, and the alar bases rotate outwardly cephalad.
Contraindications
See the list below:
-
Malnutrition, anemia, or other pediatric conditions that result in the patient's inability to tolerate general anesthesia are contraindications to this procedure.
-
Cardiac anomalies that may coexist must be addressed prior to the lip repair.
-
Figure illustrates important anatomic landmarks used in all cleft lip repairs. Measurements of various distances are used to guide the surgeon in creating a symmetric lip.
-
The Rose-Thompson repair involves curved or angled paring of the cleft margins to lengthen the lip as a straight-line closure.
-
Hagedorn-LeMesurier repair. The medial lip element is lengthened by introducing a quadrilateral flap developed from the lateral lip element.
-
Tennison-Randall repair. The medial lip element is lengthened by introducing a triangular flap from the inferior portion of the lateral lip element.
-
Skoog repair. The medial lip element is lengthened by introducing two small triangular flaps developed from the lateral lip element.
-
Millard repair. The medial lip element [R] is rotated inferiorly and the lateral lip element [A] is advanced into the resulting upper lip defect. The columellar flap [C] is then used to create the nasal sill (see text for details).
-
Millard repair. Two of the most common variations described with utilization of the C Flap to correct the hemi-columellar deficiency (Millard II] and the nasal sill alar base region [Millard I]
-
Millard repair. With maximal rotation of the R flap, any residual lip length discrepancy can be corrected with an inferior Z-plasty or a triangular flap. In a secondary correction, further rotation of the R flap can be considered.
-
Millard modification of Kernahan striped-Y classification for cleft lip and palate. The small circle indicates the incisive foramen; the triangles indicate the nasal tip and nasal floor.