Background
One of the great debates in plastic surgery has focused on whether to place breast implants over or under the pectoralis major muscle. This author's strong feeling is that, in most instances, the implant should be placed in the subglandular position, that is, over the muscle. A subglandular implant is shown below.
History of the Procedure
Breast augmentation first was attempted in the early 1900s. The site of placement was always subglandular. Everything from ivory to ebony to paraffin was implanted and, of course, rejected. In the 1950s, Ivalon sponges were used. Although they were biocompatible, fibrous tissue grew into them, making them extremely hard. Breast augmentation was begun in earnest in the mid-1960s when silicone implants were introduced. Again, the placement always was subglandular.
The major problem with breast implants consistently has been hardness. The implants themselves do not become hard; the problem is that the human body recognizes that the implant is a foreign object. Since the body cannot reject the implant (silicone has no active binding sites), the defense mechanism is for the body to wall it off with a membrane consisting of myofibrils and collagen. This commonly is termed a capsule. If the capsule contracts around the implant, the consequence is similar to squeezing a balloon partially filled with water—it feels hard. This is known as fibrous capsular contracture. Why the capsule contracts in some patients remains a mystery. Even more mysterious is the fact that it frequently occurs in only one breast and not the other.
The early silicone implants had backing made of Dacron that was meant to hold the implant in place. What was not realized for several years was that the Dacron caused a severe tissue reaction, resulting in extreme capsular contracture. In the late 1960s, the idea of putting the implant under the muscle was introduced. This placement was popularized in the mid-1970s because of the belief that the breast felt softer with subpectoral implantation. Unfortunately, the characterization of the degree of hardness is difficult to quantify. Although the Baker system of classification is widely accepted for this purpose, determining just how much firmness a breast may have remains subjective, and therein lies the problem of finding the procedure that minimizes the problem.
Problem
The argument for subpectoral (under the muscle) placement is as follows:
-
The muscle covers the implant, thus any capsular contracture (breasts that feel hard) is less common
-
For the same reason, rippling (wrinkling) of the implant is less apparent
-
Mammograms are more accurate
-
In very small-breasted women, the outline of the implant is less visible
-
The surgery takes less time
The argument for subglandular (under the breast tissue) placement is as follows:
-
The breast is obviously over the muscle, thus the implant belongs there
-
Because of this, subglandular placement most often looks more natural
-
Because the muscle covers only one third to one half of the implant when the implant is placed below it, minimal advantages exist in placing the implant there (this does not apply for the rarely performed true submuscular implant that also uses the serratus anterior muscle for coverage)
-
Because most of the implant is not covered by muscle when placed below it, minimal advantages exist in placing the implant there; only a slight diminution of the incidence of capsular contracture and implant rippling occurs (although study results on capsular contracture rates in subglandular vs submuscular augmentation vary [1, 2, 3] )
-
Subpectoral placement requires cutting the muscle insertion; because of this and/or the pressure of the underlying implant, the pectoralis muscle becomes very atrophic and virtually is destroyed; the assertion that the implant "falls" into a more natural position within weeks of the surgery is false; actually, the muscle is atrophying (dying), causing the diminution of the initial upper pole fullness
-
If any degree of ptosis is present, a subglandular implant lifts the breasts much better
-
A properly performed mammogram shows 95% of breast tissue; magnetic resonance imaging (MRI), however, can visualize 100% of the breast and will, eventually, be the criterion standard for cancer detection
-
Lower risk of postoperative bleeding is involved
-
Significantly less postoperative pain occurs [4]
-
The procedure can be performed with intravenous sedation and local anesthesia, which is a safer alternative to general (complete) anesthesia
Nevertheless, approximately 50-60% of plastic surgeons perform submuscular implantations. This author places approximately 2% of implants under the muscle, usually only when requested by the patient. The difference in appearance is depicted in the image below.
Epidemiology
Frequency
Micromastia is a common occurrence.
Presentation
Determine the patient's motivation and expectation. Be wary of the patient who wants the surgery to please her partner. Try to match the patient's expectation to the effects that can be achieved. When a patient asks for very large breasts, the author inquires if she wants a natural appearance. The answer is almost always affirmative. In that situation, the author states that he will make the breasts as large as possible and still have them appear natural.
On physical examination, noting asymmetry is important because the patient may be unaware of the problem; she may only note it postoperatively and blame the surgeon. Differences in nipple and breast height, size, and shape are common.
Look for stretch marks and assess their depth. Also observe any thinning of the breast tissues since these problems cause a higher degree of rippling (wrinkling) of the implants.
Note any degree of ptosis and advise the patient regarding how much will remain postoperatively. Except in extreme situations, the author prefers not to perform a mastopexy, since most patients are satisfied with the augmentation and whatever lift it provides and do not want the additional scarring. Failing that, a nipple lift is often sufficient. Obviously, locate any breast masses or discharge. During the physical examination, discuss the patient's desires and the size of the implant.
Indications
Micromastia (ie, small breasts) is obviously the reason patients seek an enlargement procedure. However, surprisingly, what may appear to be ample breasts to the surgeon may seem quite small to the patient requesting augmentation.
A patient occasionally requests surgery because of asymmetry.
In many cases, subglandular implants lift a drooping breast without the need for additional visible scarring.
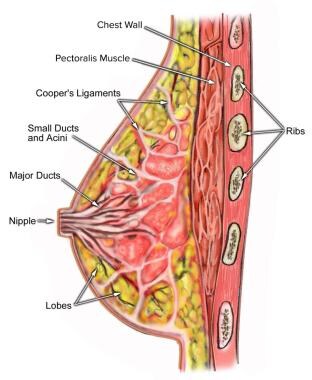
Relevant Anatomy
Breast shape varies among patients, but knowing and understanding the anatomy of the breast (see the image below) ensures safe surgical planning. When the breasts are carefully examined, significant asymmetries are revealed in most patients. Any preexisting asymmetries, spinal curvature, or chest wall deformities must be recognized and demonstrated to the patient, as these may be difficult to correct and can become noticeable in the postoperative period. Preoperative photographs with multiple views are obtained on all patients and maintained as part of the office record.
The female breast covers the anterior chest wall from approximately the second rib superiorly to the fourth or fifth rib inferiorly. Its upper one half overlies the pectoralis major muscle, the serratus anterior its lower one half, and some of the axillary fascia laterally.
The breast is essentially a skin organ. It is attached intimately to the skin by suspensory ligaments (Cooper ligaments). This is because developmentally it forms from the ectoderm of the anterolateral body wall, and epithelial proliferation from that site creates the gland. For this reason, opening the natural plane between the muscle and the breast is easy; an implant can be inserted into this space.
The blood supply of the breast is derived from branches of the axillary artery, the intercostal arteries, and the internal mammary artery. Few if any vessels penetrate into the gland from the underlying gland.
Its nerve supply comes from the anterior and lateral cutaneous branches of the fourth, fifth, and sixth thoracic nerves. One of the larger lateral cutaneous branches often can be visualized and preserved during augmentation surgery.
For more information about the relevant anatomy, see Breast Anatomy.
Contraindications
The one absolute contraindication to subglandular augmentation is an irradiated breast. Because of interference with the blood supply caused by radiation, a subpectoral placement is much safer.
Another reason to consider placing the implant under the muscle is very thin breast tissue, as can occur after pregnancy.
Some surgeons also believe that a subpectoral implantation should be used in extremely small-breasted patients, although the author feels this is necessary only in a very few patients.
Because a small amount of the breast may be obscured during a mammogram, a patient with a strong history of breast cancer probably should be augmented under the muscle, as should a patient undergoing postmastectomy reconstruction when the contralateral breast also is being augmented.
Although the author much prefers silicone gel implants, patients with a history of autoimmune diseases are advised to have saline implants.
-
Breast augmentation, subglandular. A cup to large B cup.
-
Breast augmentation, subglandular. A cup to C cup.
-
Breast augmentation, subglandular. A cup to C cup.
-
Breast augmentation, subglandular. Very small A cup to C cup.
-
Breast augmentation, subglandular. Very small A cup to large B cup.
-
Breast augmentation, subglandular. A cup to large D cup.
-
Breast augmentation, subglandular. Small B cup to D cup.
-
Breast augmentation, subglandular. A cup to Large B cup.
-
Breast augmentation, subglandular. A cup to D cup.
-
Breast augmentation, subglandular. This patient had previous implants behind the muscle. Same implants placed in front of the muscle.
-
Breast augmentation, subglandular. This patient wanted a lift and much larger breasts. A cup and slight drooping to C cup.
-
Breast augmentation, subglandular. This patient wanted a modest enlargement and less drooping. A cup and slight drooping to B cup.
-
Breast augmentation, subglandular. This patient wanted a large C and less drooping. Small B cup and moderate drooping to D cup.
-
Breast augmentation, subglandular. This patient wanted much less drooping. B cup and significant drooping to D cup.
-
Breast augmentation, subglandular. Small B cup and significant drooping to D cup.
-
Anatomy of the breast.