Background
Until the advent of cutaneous laser resurfacing in the late 1980s, physicians long had used mechanical abrasion and various chemical peeling agents to restore a youthful look to the aged face.
Some authors reported on the use of continuous wave carbon dioxide lasers for resurfacing photoaged skin with good results; however, this technique was not adopted widely because of the significant thermal damage that accompanied the use of continuous wave lasers, which meant a high likelihood of potential scarring. [1]
Advent of short-pulsed high energy and scanned carbon dioxide lasers and other laser systems that limit skin heating has revolutionized laser skin resurfacing. [1, 2, 3, 4, 5] These lasers are capable of removing layers of photodamaged skin in an impressively precise fashion, leaving only a narrow zone of thermal necrosis.
Pathophysiology
Laser-tissue interaction
Carbon dioxide laser emits light at a wavelength of 10,600 nm that is absorbed strongly by water (the primary chromophore for carbon dioxide light that is abundant in skin). Approximately 90% of carbon dioxide laser energy is absorbed in the initial 20-30 µm of skin, yet traditional continuous wave lasers leave behind a thick zone of thermal damage measuring 0.2-1 mm in thickness. [6]
Theory of selective photothermolysis states that selective heating of the target chromophore can be achieved when using laser pulses shorter than the thermal relaxation time (TRT) of the chromophore (time required for chromophore to lose 50% of its heat to surrounding tissue). TRT for 20-30 µm of skin tissue is approximately 1 millisecond.
Using the theory of selective photothermolysis, carbon dioxide lasers with a pulse duration of less than 1 millisecond are capable of selectively vaporizing tissue with only a very thin zone of residual thermal necrosis measuring approximately 100 µm.
To have a clinical effect in the skin, laser energy must be absorbed by the target chromophore. Energy fluence (density) necessary to vaporize tissue is approximately 5 J/cm2 (ablation threshold).
Overall, delivering a 1-millisecond carbon dioxide laser pulse with an energy fluence of approximately 5 J/cm2 leads to tissue vaporization measuring 20-30 µm and residual thermal injury measuring 40-120 µm. This zone of thermal necrosis is sufficient to seal small dermal blood vessels and lymphatics, yet narrow enough to reduce incidence of scarring.
Laser technology and systems
Two different types of carbon dioxide lasers are promoted for the purpose of skin resurfacing. First is a high-power pulsed carbon dioxide laser that can deliver approximately 500 µJ of energy in each submillisecond pulse, resulting in energy fluence measuring 5-7 J/cm2. Some of these systems have a computerized pattern generator (CPG) that rapidly and precisely can place individual laser pulses in several different patterns.
The second type uses an optomechanical flash scanner connected to a conventional continuous wave carbon dioxide laser. This scanner efficiently distributes laser energy into a train of pulses with a dwell time shorter than skin TRT, thus mimicking truly pulsed carbon dioxide lasers. Recently, carbon dioxide resurfacing lasers with very short pulse duration (60 microsecond) have emerged; they ablate less tissue per pass and leave behind a narrower zone of thermal necrosis than original carbon dioxide resurfacing lasers. These laser systems appear to be equally effective in skin resurfacing when they achieve similar depths of skin injury.
Mechanism of action
As with other resurfacing modalities (eg, chemical peeling, dermabrasion), completely removing the epidermis and part of the dermis results in wound remodeling with subsequent new collagen and elastin fiber formation that translates into healthier, firmer, and tighter skin. Although aware of heat-induced collagen shrinkage during laser resurfacing procedure, whether this immediate shrinkage observed clinically persists or results in long-term collagen tightening is not known.
Presentation
See the list below:
-
Obagi skin classification: This classification is probably the most comprehensive skin classification system. It analyzes skin using the following criteria:
Skin color - Original (light white, dark black, dark Asian) or deviated (brunette, white, light black, medium black, light Asian, medium Asian, complex skin); carbon dioxide laser resurfacing not recommended for any skin color other than light white, white, or brunette
Skin thickness - Thick, thin, medium (excessively thick or thin skin is a relative contraindication to this procedure)
Skin firmness - Firm versus lax
Skin fragility - Tough versus fragile
Skin oiliness - Oily, normal, dry
-
Degree of photoaging: Assess by judging degree of wrinkling, precancerous growths such as actinic keratosis, benign skin growths such as seborrheic keratosis, solar elastosis, senile comedones, telangiectasia, yellowish discoloration, mottled hyperpigmentation, and skin laxity. In general, patients with early photodamage do not require carbon dioxide laser resurfacing. The ideal patient has mild-to-moderate photoaging.
-
History of herpes labialis infection: Start suppressive therapy with oral antiviral medications 1-2 days before procedure and continue until complete reepithelialization takes place.
-
History of frequent vaginal candidal infections: Administer prophylactic course of oral antifungal medications to affected patients.
-
Paucity of adnexal structures (skin poor in pores, hair follicles, oily glands): This can occur in some skin types or can be related to a previous deep resurfacing procedure or radiation therapy.
-
History of hypertrophic scars or keloids: Avoid resurfacing deeper than papillary dermis.
-
Significant lower eyelid laxity: Avoid aggressive carbon dioxide laser resurfacing on the lid to avoid postresurfacing scleral show and ectropion.
-
Allergies: Investigate allergies to local and systemic anesthetics properly.
Select patients with realistic expectations. Avoid patients with psychological instability, since they may not be able to withstand posttreatment course and potential complications.
Indications
Recognition of suitable candidates for carbon dioxide laser resurfacing is of paramount importance to avoid undesired outcomes. [3] Generally, middle-aged patients (40-65 y) with fair skin and fine-to-moderate static (nondynamic) wrinkles are ideal candidates. Select patients with realistic expectations, such as those who seek improvement rather than complete eradication of wrinkles or scars.
Rhytides
Carbon dioxide laser resurfacing (as the sole treatment) can achieve excellent results in patients with mild-to-moderate surface texture changes and fine superficial or moderate static wrinkles but not in those with deep furrows or severe dermatoheliosis. See before and after images below.
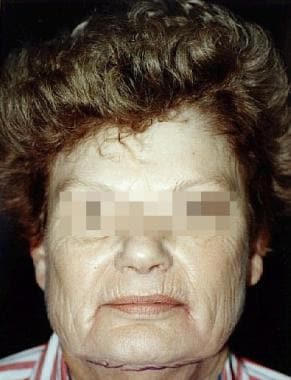 Before carbon dioxide laser resurfacing. Female patient with advanced dermatoheliosis and skin laxity before full face laser resurfacing with UltraPulse carbon dioxide laser.
Before carbon dioxide laser resurfacing. Female patient with advanced dermatoheliosis and skin laxity before full face laser resurfacing with UltraPulse carbon dioxide laser.
 Female patient with advanced dermatoheliosis and skin laxity 6 months after carbon dioxide laser resurfacing.
Female patient with advanced dermatoheliosis and skin laxity 6 months after carbon dioxide laser resurfacing.
Carbon dioxide laser resurfacing combined with botulinum toxin A (BOTOX®) for dynamic rhytides or with cervicofacial rhytidectomy and/or brow lifting for advanced skin and/or muscle laxity also can produce excellent clinical improvement in these conditions. [7]
A retrospective study by Wright and Struck indicated that facelift can be performed safely in combination with ablative fractional carbon dioxide laser resurfacing. The study included 86 patients who underwent laser resurfacing in addition to extended supraplatysmal dissection with superficial musculoaponeurotic system (SMAS) plication. Complete reepithelialization was reported in all patients by one week postprocedure, with no skin flap loss or delay in wound healing. [8]
Scars
Acne scars can be classified into 3 basic types: (1) shallow depressed scars, (2) wide-base atrophic scars, and (3) ice-pick scars. The first 2 types of acne scars generally are amenable to carbon dioxide laser resurfacing; however, fibrotic or ice-pick scars often require punch excision, punch grafts, or punch elevation. Scar base lifting and injection of filling substances for atrophic acne scars (performed as a separate procedure at a different time) also can be combined with laser resurfacing for optimal results. [9]
Varicella and smallpox scars also may be improved with carbon dioxide laser resurfacing.
Dermatoheliosis
Carbon dioxide laser resurfacing has proved to be a valuable method for facial rejuvenation of photodamaged skin with detectable improvement of fine lines and wrinkles, mottled dyspigmentation, rough skin texture, and solar lentigines. Carbon dioxide laser resurfacing can eradicate precancerous growths such as actinic keratosis, although prevention of future development of actinic keratosis has not been substantiated.
Additional indications
Other indications for carbon dioxide laser skin resurfacing include the following:
-
Verruca vulgaris/plana
-
Angiofibroma (fibrous papule of nose)
-
Junctional and compound nevi
-
Small syringomas
-
Epidermal melasma
-
Rhinophyma
Relevant Anatomy
Extensive knowledge of skin microanatomy, histology, physiology, structure, and function is essential in all resurfacing procedures.
Skin is a dynamic organ that undergoes continuous changes throughout life as outer layers are shed and replaced by inner layers. Skin also varies in thickness among anatomic location, sex, and age of the individual. This varying thickness primarily represents a difference in dermal thickness, as epidermal thickness is rather constant throughout life and from one anatomic location to another. Skin is thickest on the palms and soles of the feet (1.5 mm thick), while the thinnest skin is found on the eyelids and in the postauricular region (0.05 mm thick). For more information about the relevant anatomy, see Skin Anatomy.
Familiarity with relative skin thickness (ie, thick, thin, medium) in various parts of the face is valuable to avoid penetrating too deeply, which results in unnecessary skin injury and potential complications.
Contraindications
Absolute contraindications
See the list below:
-
Active bacterial, viral, or fungal infections
-
Unrealistic expectations
-
Uncooperative patient
Relative contraindications
See the list below:
-
Poor general health
-
Oral isotretinoin (Accutane) use within previous 6 months
-
Fitzpatrick skin phototypes 5-6
-
Reticular dermis-level resurfacing procedure within preceding 2-3 months
-
Unwillingness to accept possibility of postoperative erythema or hypopigmentation
-
Significant eyelid laxity
-
Excessively thick or thin skin
-
Collagen vascular disease
-
Human immunodeficiency virus (HIV) or hepatitis C infections
-
Tendency for keloid or hypertrophic scar formation
-
Before carbon dioxide laser resurfacing. Female patient with advanced dermatoheliosis and skin laxity before full face laser resurfacing with UltraPulse carbon dioxide laser.
-
Female patient with advanced dermatoheliosis and skin laxity 6 months after carbon dioxide laser resurfacing.
-
Depigmentation periorbitally, periorally, and on the forehead following carbon dioxide laser resurfacing.
-
Before carbon dioxide laser resurfacing. Female patient with skin and muscle laxity, photoaging, and blepharochalasis. Patient underwent combined upper and lower laser blepharoplasty, perioral and periorbital carbon dioxide laser resurfacing, superficial musculoaponeurotic system (SMAS) facelift, and full face blue peel.
-
Six months after procedure. Female patient with skin and muscle laxity, photoaging, and blepharochalasis. Patient underwent combined upper and lower laser blepharoplasty, perioral and periorbital carbon dioxide laser resurfacing, superficial musculoaponeurotic system (SMAS) facelift, and full face blue peel.







