History of the Procedure
Inferior turbinate surgery dates to the 1890s, when Jones first described it. In 1900, Holmes described the stages of inferior turbinate hypertrophy and his surgical experience with 1500 turbinectomies. Turbinectomy later fell out of favor because of rising concern over complications such as rhinitis sicca, atrophic rhinitis, and ozena. The enlarged nasal cavity resulting from turbinate resection was believed to increase nasal airflow and reduce the humidifying capabilities of the nasal mucosa, resulting in drying, crusting, and mucosal atrophy. However, several studies have reported large series of turbinectomies without these complications. This aspect of turbinate surgery remains controversial.
Problem
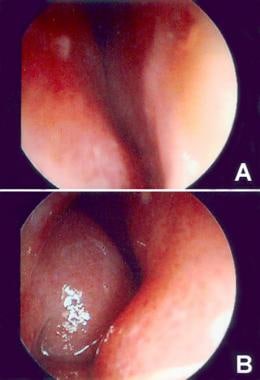
Nasal obstruction after rhinoplasty can result from alteration of the nasal valve or nasal vault narrowing as a result of osteotomies. Beekhuis concluded that nasal obstruction postrhinoplasty resulted primarily from inferior turbinate hypertrophy. [1] Changes in nasal airflow as a result of rhinoplasty may unmask inferior turbinate hypertrophy and obstruction that were not clinically significant or evident preoperatively. See the image below.
Etiology
Mink described the nasal valve in 1903. The nasal valve is formed medially by the septum and laterally by the caudal edge of the upper lateral cartilage and it accounts for approximately 50% of total upper airway resistance. The anterior tip of the inferior turbinate is found in the nasal valve region, and hypertrophy of this structure can cause exponential increases in airway resistance.
Inferior turbinate hypertrophy can result from mucosal hypertrophy, bony hypertrophy, or both. Bony hypertrophy causes a fixed structural obstruction and is best treated with surgery. More commonly, the problem is mucosal hypertrophy causing impingement on the nasal valve, increased nasal resistance, and nasal obstruction. This can be managed medically or surgically, depending on the degree of hypertrophy and responsiveness to medical management.
Pathophysiology
The nose is a complex and highly specialized organ that plays a role in olfaction, heat exchange, speech production, respiration, humidification, filtration, and antimicrobial defense.
Mucus production is provided by goblet cells and submucosal and seromucous glands. Mucus production is primarily controlled by parasympathetic innervation. The mucous blanket serves to humidify and clean the inspired air and eliminate debris from the nasal airway.
Nasal obstruction may be produced by overactivity of the parasympathetic innervation or underactivity of the sympathetic innervation. Resistance is important in nasal function and turbulence optimizes inspiratory air contact with the mucous membrane. Resistance must remain within certain limits for the perception of normal breathing. If it is too high or too low, a sensation of obstruction may occur. A cyclic alteration of constriction and dilation of the inferior turbinates, known as the nasal cycle, occurs approximately every 2-7 hours.
The nasal valve provides approximately 50% of total airway resistance. The nasal valve is the region of the nasal airway extending from the caudal end of the upper lateral cartilages and including the anterior end of the inferior turbinate. As airflow enters this constricted segment, it accelerates and the pressure drops (per Bernoulli principle), which can result in nasal valve collapse if the upper lateral cartilages are anatomically weak. The erectile tissue of the nasal septum and inferior turbinate can impinge on the nasal valve and increase resistance. Because the cross-sectional area of the nasal valve is small, minor changes in inferior turbinate congestion can have marked effects on resistance. A major determinant of resistance to airflow is the radius of the nasal vault. However, even in the presence of a normal radius, a sensation of obstruction can occur from turbulent airflow.
Presentation
History
Nasal obstruction is a common complaint. Discerning the etiology is important so that appropriate treatment can be initiated. History should address any alteration or unilaterality of the obstruction, which may indicate a dynamic versus structural problem.
Address symptoms of rhinitis. Obstruction, rhinorrhea, and sneezing may occur with allergic and nonallergic rhinitis. Elicit systemic symptoms of allergy such as watery itchy eyes, asthma, and seasonal variation. Initial general examination should note "allergic shiners" or a facial appearance that may indicate signs of chronic nasal obstruction. Vasomotor rhinitis is typically exacerbated by irritants, temperature or humidity changes, or psychological factors. Nonallergic eosinophilic rhinitis is generally perennial without allergen-induced symptoms. Atrophic rhinitis is characterized by nasal dryness and crusting, frequently with a foul odor. Rhinitis can also be associated with pregnancy and with systemic disorders such as hypothyroidism.
Medications can also cause rhinitis and nasal obstruction. Rhinitis medicamentosa results from rebound vasodilation after prolonged use of topical nasal decongestants. Typically the patient begins using the topical agent to treat an underlying disorder causing the nasal obstruction. Other medications causing increased nasal congestion include certain antihypertensives, antidepressants, antipsychotics, and oral contraceptives.
Examination
Physical examination of the external nose is, of course, critical. In addition to assessing nasal aesthetics, note the patency of the nasal valve and any alar collapse since these may need to be addressed to ensure functionality of the nose postrhinoplasty. The Cottle maneuver involves pulling the patient's cheek laterally to open the nasal valve angle. If nasal airflow symptomatically improves, this may indicate nasal valve pathology. A crooked nose may indicate prior trauma and this history should be elicited. A saddle nose deformity may indicate previous trauma, prior surgery, cocaine abuse, or an inflammatory process.
Additionally, the focus of the physical examination is anterior rhinoscopy, which reveals caudal septal deformities or inferior turbinate hypertrophy that may account for the patient's symptoms. If the patient has a significant caudal septal deflection, typically the inferior turbinate on the side opposite the deviation is enlarged. Apply topical decongestant to evaluate the response of the turbinate mucosa. This may assist in delineating mucosal versus bony hypertrophy.
If indicated based on history, symptoms, or signs, a more extensive examination of the nose can be performed via a rigid or flexible endoscope. This examination allows additional assessment of the septum posteriorly, the nasopharynx, and the sinus ostia. Nasal masses or polyps as a cause of obstruction can be evaluated. Purulent drainage may indicate sinusitis. Evidence of a septal perforation may indicate prior surgery, cocaine or topical decongestant abuse, or an inflammatory disease. Significant crusting or abnormality of the mucosal appearance may indicate a systemic disorder.
History or symptoms and signs of other systemic disorders that may affect the nose and turbinates warrant further investigation. Wegener granulomatosis and sarcoid can result in nasal obstruction and crusting. Infectious rhinitis can result from a variety of organism-caused conditions such as rhinoscleroma, tuberculosis, syphilis, rhinosporidiosis, histoplasmosis, and aspergillosis. If suspected, address a history of exposure and travel and perform further appropriate testing. A significant history of epistaxis may raise the concern of an inflammatory or neoplastic process.
Indications
Nasal obstruction may result from mucosal hypertrophy of the inferior turbinate, structural deformity of the nasal airway (septal deviation, bony inferior turbinate hypertrophy), or dynamic airway collapse.
Typically, in the patient with significant nasal septal deviation, unilateral compensatory turbinate hypertrophy may be present on the side opposite the deviation. However, if the septal deviation is S shaped or deflections exist bilaterally, then bilateral inferior turbinate enlargement may be present. If the hypertrophied turbinate is not addressed, nasal airway obstruction may persist despite correction of septal deformities.
Similarly, relative inferior turbinate hypertrophy occurs in patients with a narrow nasal vault either inherently or secondary to rhinoplasty maneuvers. Failure to perform reduction of the inferior turbinates may result in nasal airway obstruction despite correction of any septal deformities.
Relevant Anatomy
Lateral nasal wall
The lateral nasal wall is composed of the nasal, frontal, occipital, lacrimal, ethmoid, maxillary, and palatine bones. The inferior turbinate constitutes a separate bone and articulates with the maxilla, lacrimal, ethmoid, and palatine bones. The superior and middle turbinates project off the ethmoid bone. The lacrimal process of the inferior turbinate forms the medial wall of the nasolacrimal duct, which drains into the inferior meatus.
Nasal valve
The nasal valve is formed laterally by the caudal end of the upper lateral cartilages and medially by the septum. The anterior tip of the inferior turbinate lies in the area of the nasal valve.
Nasal mucosa
The nasal vestibule, constituting the first 1-2 cm of the nasal cavity, is lined with keratinized, stratified squamous epithelium containing hair follicles and sebaceous and sweat glands. At the mucocutaneous junction (limen nasi), the epithelium transitions to pseudostratified ciliated columnar cells. This epithelium lines most of the sinonasal tract with the exception of the olfactory mucosa.
Blood supply
The arterial blood supply to the nose originates from the maxillary and facial branches of the external carotid artery and from the ophthalmic branch of the internal carotid artery. The anterior facial vein, sphenopalatine vein, and ethmoid vein supply venous drainage. The nasal vasculature is composed of arterioles, submucosal capillary beds, and venules. Specifically, the nasal vasculature of the inferior turbinate is a sinusoidal network of large capacitance vessels. These sinusoidal vessels are found primarily in the inferior turbinate and the anterior septum. The result is that the inferior turbinate functions as erectile tissue.
Constriction of postsinusoidal venules results in engorgement of the sinusoids and an enlargement of the nasal turbinates. In addition, multiple direct arteriovenous anastomoses bypass the capillary beds. This allows significant increases in blood flow and heat exchange without a great increase in nasal blood volume, which facilitates the temperature regulatory function of the inferior turbinates. The nasal mucosal vasculature is intimately related to its autonomic innervation.
Innervation
In general, the nose is innervated by the olfactory nerve, branches of the ophthalmic and maxillary divisions of the trigeminal nerve, parasympathetic secretomotor fibers, and sympathetic fibers. The autonomic nerve supply to the nose regulates vascular tone, turbinate congestion, and nasal secretion. Parasympathetic fibers synapse in the sphenopalatine ganglion before innervating nasal mucosa. These fibers travel with the facial nerve, exiting at the geniculate ganglion as the greater superficial petrosal nerve. The vidian nerve is formed by the union of the greater superficial petrosal and deep petrosal nerves and carries the fibers to the sphenopalatine ganglion, where they synapse.
Sympathetic fibers also pass through the sphenopalatine ganglion but do not synapse there. The sympathetic fibers exit the spine and travel in the cervical sympathetic trunk, synapsing in the superior cervical ganglion. Postsynaptic fibers contribute to the sympathetic plexus of the internal carotid artery from which the deep petrosal nerve originates. It then joins with the greater superficial petrosal nerve to form the vidian nerve and its fibers pass through the sphenopalatine ganglion and along branches of the trigeminal nerve and nasal blood vessels. Thus, branches of the sphenopalatine ganglion carry sympathetic, parasympathetic, and trigeminal fibers.
Contraindications
The inferior turbinates are very vascular structures and one of the risks of surgery is hemorrhage. Patients with coagulopathies are clearly at increased risk of complications. Similarly, patients should not be taking any medications or herbs that affect their coagulation cascade.
Take care when resecting turbinate tissue in patients who have preexisting reports of nasal dryness and crusting secondary to the concern about atrophic rhinitis.
-
(A) Endoscopic view of left nares showing caudal septal deflection to the left. (B) Endoscopic view of right nares showing compensatory right inferior turbinate hypertrophy.
-
Lateral outfracture.
-
Intramural cautery.
-
Submucous resection.
-
Partial inferior turbinectomy.
-
Inferior turbinoplasty.
-
Total inferior turbinectomy.