Background
Maxillary augmentation denotes the genre of reconstructive surgeries that address the correction of maxillary hypoplasia. Maxillary hypoplasia results from the underdevelopment of the maxillary bones and produces midfacial retrusion, creating the illusion of protuberance of the lower jaw. As a result the profile appears prognathic.
History of the Procedure
Cinelli provided one of the earliest descriptions of correcting maxillary hypoplasia in 1958. [1] Correction of the premaxillary segment of a patient with an acute columella-labial angle and an overly long nose was undertaken by rotating a caudal septal cartilage flap onto the maxilla.
Problem
Maxillary hypoplasia can affect different subunits of the maxillary bone. If the entire maxilla is hypoplastic, it is termed maxillary micrognathia, while premaxillary hypoplasia refers to the part of the maxillary bone between the lateral maxillary incisor fissures. Many authors refer to this area when speaking of maxillary hypoplasia in relation to rhinoplasty. The anterior spine of the maxilla can be hypoplastic, requiring augmentation with a maxillary spine graft. Hypoplasia in the area of the alar-facial junction may also occur, while Byrd and Hobar defined perialar hypoplasia as a deficiency of the nasal base skeleton. [2] This deficiency results in ptosis and a diminished projection of the nasal tip. With an acute columella-labial angle, an edentulous appearance can be appreciated along with deepening of facial folds and posterior displacement of the alar base in relation to the cheek. Hinderer described para-alar implants for the correction of deep alar and nasolabial grooves. [3]
Medial maxillary hypoplasia, also known as nasomaxillary hypoplasia, can create a "dishpan face" appearance. [2] Hinderer described this as maxillary body hypoplasia resulting in a depression of the paranasal midface.
Hypoplasia of the maxillary bone in the medial inferior orbital region can result in a tear-trough deformity, occasionally observed with malar (zygoma) hypoplasia. At times, various authors interchange premaxillary with maxillary and perialar hypoplasia when referring to the same hypoplastic area.
Epidemiology
Frequency
Often, maxillary hypoplasia is observed in various ethnic groups, but it may not be appreciated as a cause of facial deformity if subtle.
Etiology
Congenital, acquired, or developmental maxillary hypoplasia can occur.
Pathophysiology
Craniofacial anomalies, Apert syndrome, and Crouzon syndrome include maxillary and cranial hypoplasia.
More localized anomalies, such as Binder syndrome, also known as maxillonasal dysplasia, refer to congenital maxillary hypoplasia. In Binder syndrome, the anterior nasal spine, nasal bone, and anterior maxillary hypoplasia are affected. These patients have a concave midface with a C-shaped profile; a blunted, short nose; and an acute columella-labial angle. [4] A 17-year retrospective study recommended surgery in the midteenage years in these patients, thereby allowing the midface to mature. [5] Gewalli et al had good results with both bone and cartilage in these patients. [6] Holmes et al preferred the use of serial silicone implants for prepuberty expansion and then placement of costochondral cartilage. [7]
Cleft palate and labial deformities are often coupled with premaxillary hypoplasia, [8] resulting in an acute columella-labial angle, ptosis of the nasal tip, and upper labial retraction, with possible exposure of the upper gingiva.
Etiologies of acquired hypoplasia are often from trauma or from malposition of the maxillary bone following surgery. Converse et al have postulated that during childhood, trauma can have a retarding effect on facial development. [9]
Developmental hypoplasia may be a sequela to dental extraction, with failure of the maxillary bone to properly mature and expand.
Presentation
Patients of Northern European ancestry, including English descendants, can have maxillary hypoplasia. [10]
Premaxillary hypoplasia is often observed in patients of Hispanic, African American, and Asian (mesorrhine) heritage. Platyrrhine (African American) noses can also appear flared with widened alae, insufficient dorsal nasal support, and underprojection of the nasal tip. [11]
Indications
Aesthetic considerations
The middle third of the face is the area delineated by a horizontal line connecting the lateral canthi to a horizontal line tangentially placed at the upper edge of Cupid's bow of the lip. [12] More common descriptions denote the middle third of the face to encompass from the glabella to the subnasale [12] or from the brow to the base of the nose. [13]
Classic ideal facial proportions divide the face into thirds from the hairline to the lower border of the chin and into fifths from one outer ear to other outer ear. Dividing the face into vertical thirds and horizontal fifths connotes symmetry. However, not all faces considered beautiful adhere to these aesthetic "rules." Aesthetically appealing facial features vary by sex, race, and the eye of the beholder.
While certain aspects of facial beauty or facial handsomeness transcend culture, ethnicity, and time, other aspects are particular to one or more of these conditions. Facial features that are considered beautiful in today's world can differ not only between Eastern and Western cultures, but from age to age within a given culture.
Maxillary augmentation is indicated when any part of the maxilla is hypoplastic and creates an aesthetic or functional deficiency. Maxillary augmentation in the context discussed herein specifically denotes an adjunctive procedure for the premaxilla only used during rhinoplasties.
If malocclusion exists, surgeries that create osteotomies, such as Le Fort I-type fractures, anterior maxillary displacement, maxillary osteotomies, [5] and other orthognathic procedures, can be used. [14]
Often, maxillary augmentation is undertaken in orthodontic procedures and in elongation of the vertical length of the face. [15] Various materials such as calvarial and iliac bone grafts, [16, 17] as well as costal cartilage grafts, have been used, [18] but are not discussed in this article. Goh and Chen used silastic nasal implants in cases in which earlier surgery was required. [5]
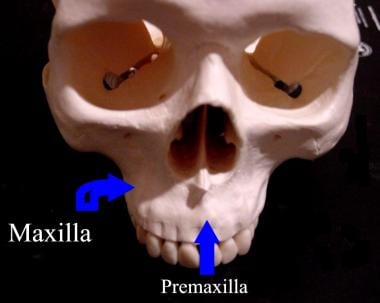
Relevant Anatomy
Each of the two maxillary bones is pyramidal and consists of 4 legs or processes: the zygomatic process, the frontal process, the alveolar process, and the palatine process. These processes emanate from the body of the maxillary bone. The premaxilla is found between the lateral maxillary incisor fissures anterior to the incisive foramen (see images below). The premaxilla includes the 4 incisor teeth and the nasal spine.
Within the body of the maxillary bone is the maxillary sinus. The orbital floor serves as the roof of the maxillary sinus and transmits the infraorbital neurovascular structures via the infraorbital groove and canal. These structures exit at the infraorbital foramen, superior to the canine fossa.
The frontal surface of the maxillary bone forms the anterior wall of the maxillary sinus and contains the infraorbital foramen. The lateral nasal wall forms the medial wall of the maxillary sinus and the alveolar and palatine processes form the floor of the sinus.
The alveolar process houses the teeth, and the palatine process forms most of the hard palate. The zygomatic process of the maxilla joins the zygoma, forming the infraorbital rim and most of the floor of the orbit. Lastly, the frontal process of the maxilla extends superiorly and joins with the nasal bone, the lacrimal bone, and the frontal bone.
The maxillary bone is composed of 4 vertical buttresses. One buttress is the lateral buttress, which is also referred to as the zygomaticomaxillary buttress; the anterior buttress is referred to as the nasomaxillary buttress. The posterior buttress is also referred to as the pterygomaxillary buttress. The final buttress, the median buttress, is also referred to as the frontoethmoidovomerian or frontoethmoidal vomerian buttress. The first 3 buttresses are dual or paired whereas the last buttress is single.
Contraindications
A major contraindication is an allergy to implant materials.
A relative contraindication is presented by patients who have extremely thin skin, making implant camouflage challenging.
-
Skeleton of the head. Superiofrontal view showing maxilla and premaxilla.
-
View of head skeleton from below showing incisive foramen, palate, and premaxilla.
-
Front view of Brink Peri-Pyriform (tm) silicone implant from Implantech.
-
Side view of Brink Peri-Pyriform (tm) silicone implant from Implantech.
-
Fanous premaxillary silicone implant