Background
Eyebrow ptosis is a result of gravitational and involutional changes defined by eyebrows that rest lower than their normal position. Other causes of brow ptosis include facial palsy, tumors, and asymmetry related to trauma. The patient may present complaining of difficulty with vision because of secondary dermatochalasis, irritation of the eyes from lash ptosis (again caused by secondary dermatochalasis), or cosmetic concerns.
Many surgical approaches to the ptotic brow are available, including the direct brow lift, mid forehead lift, pretrichial lift, temporal lift, coronal lift, and endoscopic lift. This article reviews the assessment and planning of brow lifts in general and indications for the mid forehead lift in particular. [1] See the image below.
History of the Procedure
Lexer provided the first documented discussion of a forehead lift in 1910. Hunt subsequently described a coronal resection of tissue for lifting the forehead. The first known documentation of the mid forehead lift was provided by Joseph in 1931; he described both pretrichial and lower forehead incisional lifts. Passot described excision of skin behind the hairline and in 1933 combined it with denervation of the temporal branch of the facial nerve. Edwards proposed isolated temporal neurectomy in 1957. Bames described a direct eyebrow lift via which he also excised the corrugators, undermined the forehead up to the hairline, and crosshatched the frontalis muscle. This was a variation of the mid forehead incisional approach in that essentially the same technique was performed via a lower incision.
Pangman and Wallace described modern approaches to forehead lifts in 1961. They described a hairline approach as well as a coronal approach with the incision 1 cm posterior to the hairline. In 1962, Gonzalez-Ulloa included the forehead lift as a part of his facelift procedure.
In the late 1960s and early 1970s, reports by surgeons suggested that coronal forehead lift results were temporary and the procedure lost favor. However, these earlier approaches consisted of excision of forehead or scalp skin, occasionally without undermining, but always without interruption of the frontalis muscle action. However, in 1957, Bames had bluntly crosshatched the frontalis through the superciliary incision.
Other authors incised the frontalis through different approaches. Subsequently, in the mid-1970s, Griffiths, Hinderer, Marino, Skoog, Vinas, and other authors demonstrated that excision of a strip of frontalis muscle eliminated the dynamic factors that contributed to the formation of horizontal wrinkles and permitted more stretching of the superficial tissues. In 1975, Washio studied cadaver foreheads and concluded that removal of a transverse segment of muscle allowed significant passive elevation of the forehead. Subsequently, Tessier (in 1968) and LeRoux and Jones (in 1974) advocated complete removal of the frontalis muscle.
More recently, endoscopic approaches have added much to the understanding of effective forehead lifting techniques with minimal incisions. The anatomy of eyebrow ptosis and the neurologic details of the sensory and motor innervation of the forehead were described in more detail in the 1990s, leading to more accurate approaches to eyebrow ptosis repair.
With recent advances in endoscopic approaches, procedures such as coronal forehead lifts, mid forehead lifts, and direct eyebrow lifts are performed less often. However, appropriately selected patients may benefit from these procedures, and the limits of minimally invasive endoscopic access should also be recognized.
Problem
Eyebrow ptosis is essentially a result of gravitational effects. [2] Laxity of the forehead, eyebrows, and eyelids develops with time, resulting in inferior migration of the brow. With the downward movement of the eyebrows, the frontalis muscle attempts to compensate by elevating the brows, which results in horizontal furrows. Unlike the medial two thirds of the eyebrow, the lateral third does not have deep structural periosteal attachments, rendering it especially susceptible to temporal brow ptosis. In addition, the frontalis muscle fibers do not extend to the lateral brow, further contributing to the lack of lateral support. As a result of this underlying anatomic paradigm, observing severe temporal brow ptosis with secondary dermatochalasis causing hooding of the upper lid skin without any great medial brow ptosis is not uncommon.
Epidemiology
Frequency
Objective criteria for brow ptosis remain ill-defined; no statistics are available for the incidence of significant brow ptosis. However, the authors contend that objective evaluation of brow position with aging would reveal a significant mischaracterization; almost every patient who presents with significant dermatochalasis has some degree of brow ptosis contributing to the problem. If one elevates the brows even moderately in a patient with a significant degree of dermatochalasis, one is struck by the contribution of brow ptosis. Even in relatively young patients in their 20s and 30s, brow ptosis is a common finding. This is especially so in patients leading an outdoors lifestyle, where constant use of the corrugator, procerus, and orbital orbicularis oculi muscles contributes to the decline of the brow.
When assessing aesthetic patients, note that brow ptosis results in horizontal as well as vertical redundancy of tissues. Every patient observed by the authors with upper eyelid ptosis or dermatochalasis, whether functional or cosmetic in nature, is assessed for brow ptosis. While not every patient is submitted to a brow lifting procedure or even given a recommendation to undergo a brow lift, the illustration of the effect of the brow on the upper eyelid helps to instill realistic expectations in the patient.
International
No firm statistics are available regarding brow ptosis in different races. However, the authors have observed a vast difference in the degree of brow ptosis in different races. When operating in Africa, they note that while ptosis is as common as in Caucasians, dermatochalasis and significant brow ptosis are observed much less often, even though most of these individuals work and live without appropriate ocular protection. Indeed, even in elderly African men who have worked outdoors all their lives, forehead horizontal wrinkles are relatively uncommon.
Asian populations naturally have heavy brows; the low insertion of the orbital septum to the levator aponeurosis in the eyelid results in a low eyelid crease. The effect of the brow on upper eyelid dermatochalasis is usually obvious. Accordingly, forehead lifts are required less commonly in most of these patients.
Etiology
Forehead, eyebrow, and eyelid relationships
Facial expression and patient mood may be determined by positional and relational changes of the forehead, eyebrow, and eyelids. Forehead rhytides project tiredness, sleepiness, or worry. A study by Forte et al indicated that, with regard to facial subunits, horizontal forehead rhytides have the sixth greatest impact on the perception of age when the face is viewed frontally. Forehead rhytides followed, in order of impact, full facial aging, middle-third facial aging, lower-third facial aging, upper-third facial aging, and vertical lip rhytides. [3]
Eyebrow position and shape are particularly powerful determinants of interpersonal perception. Low lateral eyebrows reflect surprise or sadness, while low medial position may suggest anger. Flat brow shape may suggest tiredness, while appropriately shaped and positioned eyebrows may be perceived as expressing happiness.
Similarly, dermatochalasis can affect the visual field but also suggests tiredness because of the effect of the excess skin and the secondary compensatory brow elevation. If an upper blepharoplasty is performed in the presence of brow ptosis, the patient must understand that this results in further lowering of the brow. Indeed, when the excess skin has been removed from the upper eyelid, the impetus for the patient to keep the brows up is lost, and brow ptosis appears to be much worse than that expected simply by performing the blepharoplasty.
Pathophysiology
The development of brow ptosis is multifactorial. Review of patient photographs and patient family photographs may reveal a striking resemblance between the patient and his or her parent(s). A common refrain heard in the plastic surgery clinic is "I am becoming my mother!" The cause of brow ptosis may be genetic, with patients and their parents sharing similar familial characteristics, similar bony anatomy, and the "aging clock."
A second contributing factor is probably lifestyle. Patients who participate in sports or many outdoor activities often have marked overaction of the corrugator and procerus muscles and associated frontalis overaction. These patients constantly pull the brow and forehead downwards and inwards. They develop impressive corrugator and procerus lines (often described by patients as "elevenses" because of the vertical parallel lines) and horizontal frontalis forehead lines. The eyebrows seem to be closer together in these patients; they also have the horizontal nasal bridge line of central forehead collapse. The brows may appear increasingly closer together with age; this is demonstrated through comparison of current and less recent photographs of patients.
The lack of lateral support by the frontalis muscle results in an exaggerated lateral brow droop with secondary lateral upper eyelid dermatochalasis, hooding of skin laterally, and crow's feet.
Presentation
Physical
Patients with brow ptosis may present for functional or cosmetic reasons. Secondary dermatochalasis may result in a superior visual field defect. Brow ptosis and dermatochalasis may independently contribute to superior and superotemporal field defects.
Cosmetic patients frequently focus on the dermatochalasis and must be educated on the contribution of brow ptosis to dermatochalasis. Complaints such as looking tired, angry, or unhappy and comments to that end from friends and colleagues are frequently causes for consultation. A patient presenting with a complaint that the brows are too low is uncommon. Corrugator and procerus muscle action leads to glabellar rhytides, again resulting in comments about anger and tiredness.
History
The preoperative workup of any surgical patient must be thorough. Specific details regarding forehead lifts are mentioned. Besides noting the patient's previous illnesses, medications, allergies, and history of unusual scarring, place emphasis on excluding thyroid disease, bleeding tendencies, and unusual edema. Patients with thyroid disease may require medical treatment, with surgical intervention reserved for when thyroid status has been stable for at least 6 months. Eyelid position, degree of fat herniation, and extent of eyelid edema fluctuates in patients with thyroid disease while they are undergoing treatment.
Examination of forehead and eyebrows
Whenever operating on any aspect of the face, examining the whole face and the relationship of relative structures is paramount. Even if the patient is specifically requesting eyebrow elevation or blepharoplasty, assessment of the relations of the various structures allows the surgeon to provide realistic expectations.
Examination of the forehead and brow includes assessment of the hairline, density of scalp hair, height of the forehead (distance between the brow and anterior scalp hairline), brow position and brow symmetry, upper eyelid skin crease and extent of dermatochalasis and fat herniation, individual brow malposition (eg, medial droop), extent of forehead rhytides (eg, transverse lines, glabellar lines, temporal lines, crow's feet), and position of the upper eyelid margin.
Determine if brow ptosis is present. No objective standard allows accurate assessment of the presence or absence of brow ptosis. However, a useful measurement is the distance between the inferior limbus of the cornea and the center of the brow. This distance is usually 22 mm or more. Anything less than 22 mm suggests brow ptosis, especially in women. The ideal brow position is very much an individual feature, determined best by the surgeon as well as the patient. The authors customarily review photographs of all patients from their younger days to see if an age exists when the brows were located in a position that the patient considers acceptable. Furthermore, the authors contend that brow shape may be the more critical determinant of brow ptosis, which is subjective. [4]
Measurement of brow ptosis
Measure the degree of brow ptosis medially, centrally, and temporally by holding a ruler with the zero mark at the upper border of the brow when it is relaxed and sequentially lifting the brow in the 3 positions until the desired position is achieved. Almost all patients have some degree of eyebrow ptosis asymmetry. This needs to be documented and shown to the patient in a mirror, since most patients are unaware of this fact. The surgeon can rest assured that postoperatively, the patient certainly notices any asymmetry, whether or not it was present preoperatively. [5]
Note the depth and distribution of the forehead, temporal, and glabellar rhytides. In particular, note the depth and distribution of the forehead rhytides when assessing a patient for a possible mid forehead lift. Note the density of the scalp hair and measure the distance between the brow and the anterior scalp hairline. Observing exact figures regarding the normal distance between the brows and the anterior hairline is difficult since a vast degree of racial and genetic variation is present. Whether a patient has a high forehead and whether the anterior hairline should be brought forward and downward should be determined for each patient individually. In general, men benefit from bringing their anterior hairlines forward, as do some women. Conversely, most women and many men do not do well with forehead scars that result from mid forehead lifts.
Inherent in the brow evaluation is an assessment of the upper eyelid. Assess the corneal reflex-lid margin distance, note the position of the upper eyelid skin crease, the extent of upper eyelid dermatochalasis that is not caused by brow ptosis, and the degree of upper fat herniation and lacrimal gland herniation.
Since most patients having a brow lift also undergo an upper eyelid blepharoplasty, possibly with correction of ptosis, lower eyelid (eg, laxity, snap back test, inferior scleral show) and cheek positions should be assessed on each patient. [6] This is discussed elsewhere in this journal (see Upper Lid Blepharoplasty). Similarly, assess the Bell phenomenon, corneal sensation, corneal staining, completeness of the blink, and tear film integrity.
Chao et al stated that uncorrected eyelid ptosis is a common finding in patients who have undergone facial rejuvenation. Such ptosis is often missed, they said, because in many cases patients compensate for the condition by employing the frontalis muscle to lift the eyelids. In a study by these investigators, the rate of eyelid ptosis among 59 patients being evaluated for facial rejuvenation (mean age 63.7 years) was 57.6%. The authors cautioned that in order to achieve better surgical outcomes, plastic surgeons need to be aware that eyelid ptosis is prevalent among facial rejuvenation candidates. [7]
A summary of patient evaluation for forehead and brow elevation is as follows:
-
Hair - Density and distribution
-
Hairline - Frontal and temporal
-
Forehead height relative to facial proportions
-
Forehead height - Eyebrows to anterior scalp hairline
-
Forehead transverse rhytides - Distribution and depth
-
Forehead temporal rhytides
-
Crow's feet
-
Skin thickness, quality, and sebaceous quality
-
Eyebrow shape and symmetry
-
Eyebrow position (degree of medial, central, and lateral ptosis)
-
Eyebrow hair distribution - Evidence of plucking, loss, other changes
-
Eyebrow mobility (eg, paralysis, scarring, tumor)
-
Severity and distribution of glabellar and nasal root rhytides
-
Degree of dermatochalasis, hooding, and eyelid ptosis
Indications
General indications exist for performing a brow lift. [8]
-
Brow ptosis leading to secondary dermatochalasis with visual field restriction
-
Brow ptosis presenting together with significant upper dermatochalasis
-
Temporal brow ptosis causing temporal hooding of the skin
-
Brow ptosis resulting in a cosmetic deformity (eg, angry, sad appearance)
-
Brow ptosis from facial palsy
-
Patients who already have had upper dermatochalasis and who still complain of visual compromise, usually as a result of previously unrecognized brow ptosis
Specific indications for performing a mid forehead brow lift are as follows:
-
Men who have prominent forehead furrows
-
Patients, particularly men, in whom lowering the frontal hairline is desirable (because the procedure lowers the frontal hairline)
-
Patients with a high, sparse, or receding frontal hairline
Relevant Anatomy
Surface anatomy
The surface anatomy of the male and female brow differs. However, generally, the medial eyebrow is approximately 1 cm above the superior orbital rim in both sexes. In women, the eyebrow arches more dramatically, with the apex approximately over the lateral limbus. In men, the eyebrow curve is more subtle, with a straighter and gentler arch, but again, the maximal height is approximately at the lateral limbus. Manual elevation of the medial, central, and lateral portion of the eyebrow during examination allows determination of the best position of the eyebrow and of the contribution of eyebrow ptosis to dermatochalasis. Specifically, the redundant upper eyelid tissues over the medial canthus, the center of the eyelid, and the lateral canthus are assessed.
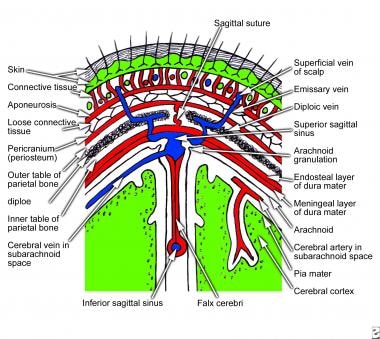
Scalp and forehead
The scalp has 5 layers: skin, superficial fascia (which is a fibrofatty layer adherent to the skin and to the underlying muscle and its aponeurosis), tendinous galea aponeurotica (and its associated occipitofrontalis muscle), loose areolar tissue that occupies the subaponeurotic space, and periosteum. The galea splits to form a sheath around the muscles. The fourth layer, the loose areolar tissue, contains small arteries and emissary veins. See the image below.
Muscles
The forehead and eyebrow regions are composed of 5 major muscles: the occipitofrontalis, orbicularis oculi, depressor superciliaris, corrugator supercilii, and procerus. The occipitofrontalis has 4 bellies, 2 occipital and 2 frontal, connected by the epicranial aponeurosis, also termed the galea aponeurotica. The occipital bellies arise from the highest nuchal line on the occipital bone and pass forward to insert on the galea. The frontal portion has no bony insertion but arises from the skin and superficial fascia of the eyebrow, passes through the orbital orbicularis oculi muscle, and inserts on the galea approximately midway between the coronal suture and the brow.
The orbicularis oculi muscle has 3 parts, the orbital, preseptal, and pretarsal orbicularis oculi muscle. The orbital portion overlies the orbital rim and arises from the anterior limb of the medial canthal tendon and the surrounding periosteum. The fibers sweep superiorly and inferiorly around the eye and meet laterally over the zygoma. The preseptal portion of the orbicularis oculi has superficial heads from the medial canthal tendon and deep heads from the posterior lacrimal crest. The fibers that sweep laterally form the lateral palpebral raphe.
The pretarsal fibers arise from the medial canthal tendon and Horner muscle. These fibers pass laterally to unite at the lateral canthal tendon. The orbicularis oculi muscle closes the eyelids, thereby pulling the skin of the forehead, temple, and cheek toward the eyes. The superior orbital portion of the orbicularis oculi muscle is a particularly powerful depressor of the brow, as is evident in patients with blepharospasm.
The frontalis muscle inserts into the eyebrow where it interdigitates with the corrugator supercilii muscles. The corrugator supercilii muscles originate from the nasal process of the frontal bone at the superomedial orbital rim. The muscle inserts into the medial cutaneous portion of the eyebrow, interdigitating with the frontalis muscle. The corrugator muscles produce vertical glabellar furrows.
The procerus muscle appears as a continuation of the inferior medial end of the frontalis muscle. It arises from the lower part of the nasal bone, and its action pulls down the medial end of the eyebrow and produces horizontal wrinkles of the skin. Some surgeons have suggested that the medial part of the corrugator muscle is an elevator of the medial brow, although this view is not accepted widely.
Several recent studies have demonstrated the presence of a distinct layer of fibroadipose tissue posterior to the orbicularis oculi and frontalis muscles and anterior to the orbital septum. This retro-orbicularis oculi fat (ROOF) tissue is best developed in the eyebrow but may continue inferiorly into the eyelid, nearly to the point where the orbital septum joins the levator aponeurosis. The ROOF is more fibrofatty than postseptal eyelid fat. It gives temporal eyelid and brow fullness, which persists after upper blepharoplasty and trimming of postseptal fat. Sculpting of the fibrofatty ROOF gives sharper orbital margin definition than simply elevating the brow and removing orbital fat. However, this must be performed judiciously to avoid an excessively harsh skeletonized look.
Although only recently stressed in the literature, this retro-orbicularis fat first was described in 1909 by Charpy, who mistook it to be a lateral orbital fat pocket. Eyebrow fat pads are larger in patients with thyroid orbitopathy and require particular attention when performing cosmetic upper eyelid and brow surgery.
The muscle plane of the eyebrow is secured to the frontal bone periosteum by a firm attachment on the underside of the fat pad, often known as the deep galeal insertion, particularly over the medial two thirds of the orbit. The submuscular fibroadipose layer appears to enhance eyelid and eyebrow mobility. This allows wide excursion of the eyebrow above and below the orbital rim with appropriate muscular contracture. A constant artery and vein are found in the mid forehead area, just above the brow. These are branches of the temporal artery and temporal vein, respectively. These vessels are encountered within the deeper part of the brow fat pad.
Motor nerves
The facial nerve emerges from the stylomastoid foramen and enters the anteromedial surface of the parotid gland. It then passes forward within the gland, superficial to the retromandibular vein and external carotid artery, and divides into 5 terminal branches. The frontal branch of the facial nerve emerges from the upper border of the gland and supplies the anterior and superior auricular muscles, the frontal belly of the occipitofrontalis, the orbicularis oculi, and the corrugator supercilii. The frontal branch travels superiorly in the musculoaponeurotic layer. Temporal to the nerve in this layer are the superficial temporal artery and vein. The surface markings of the frontal branch are 1.5 cm above the lateral eyebrow and 2 cm lateral to the lateral orbital rim.
The nerve actually divides into several branches over the zygomatic arch and it is safer to assume that the nerve occupies a width of approximately 2 cm of the arch approximately 2 cm from the lateral orbital rim. Branches of the frontal nerve enter the corrugator supercilii muscle at its lateral end just before the muscle passes into the frontalis and orbicularis muscles. See the image below.
Sensory nerves
The supraorbital nerve (see the image above) runs cephalad, deep to the corrugator supercilii muscle immediately after exiting the supraorbital rim, either from a foramen just superior to the orbital rim or from a notch in the middle third of the rim. The supraorbital nerve is shown in anatomy textbooks to run over the frontalis muscle to the occipital area. In cadaver studies, Knize recently has shown that this is not the case. [9] He found that the supraorbital nerve divides into the medial (superficial) and lateral (deep) divisions. [9]
The superficial division divides into multiple branches that penetrate the frontalis muscle and pass cephalad over the frontalis muscle to supply at most 3.5 cm of the frontal scalp. The deep division courses laterally between the periosteum and the galea aponeurotica. The deep division has few fine branches and runs up to the coronal suture.
The supratrochlear nerve exits the orbit just lateral to the corrugator supercilii muscle's bony origin, enters the muscle, and divides into 3-4 smaller branches. These branches course cephalad on or just deep to the anterior surface of the corrugator supercilii muscle and then penetrate the frontalis muscle and run on its medial ipsilateral surface toward the scalp.
Multiple fine branches of the infratrochlear nerve are present on the medial side of the corrugator supercilii muscle near its origin, although they generally do not enter the corrugator supercilii muscle. The supratrochlear nerve supplies a mid line vertical strip approximately 1 cm wide. The infratrochlear nerve innervates the skin between the medial canthus and the nasal bridge. Blocking this nerve during a forehead lift is important, since dissecting in this region is necessary to correct the horizontal nasal furrows.
The location of the supraorbital nerve and the supratrochlear nerve with respect to the mid line is approximately 2.7 cm and 1.7 cm, respectively. Marker sutures may be placed at these points to identify these nerves in brow lifts.
Fascia
The relation of the frontal nerve to the various forehead fascial planes is important to understand. Three fascial layers within the temporal region are in close relation to the frontal branch of the facial nerve: the temporoparietal fascia (superficial temporal fascia) and the deep temporal fascia, which consists of a superficial and a deep layer. The temporoparietal fascia represents a cephalad extension of the superficial musculoaponeurotic system (SMAS) across the zygomatic arch and is in continuity with the galea above, the frontalis anteriorly, and the occipitalis posteriorly. This fascial layer is either superficial or lies superficially to the zygomatic arch and encompasses the frontal branch of the facial nerve and superficial temporal vessels.
The frontal branch of the facial nerve lies on the undersurface of this layer. The nerve is superficial in its course across the zygomatic arch and is separated from the underlying zygomatic arch by the superficial layer of the deep temporal fascia and the loose areolar plane.
The temporoparietal fascia is separated from the superficial and deep layers of the deep temporal fascia by a loose areolar plane, which is termed the subaponeurotic plane. This loose areolar layer is the level of dissection commonly used when operating within the temporal region, and its degree of thickness is generally not appreciated. Dissection is possible beneath the undersurface of the temporoparietal fascia or directly on top of the surface of the superficial layer of the deep temporal fascia. The subaponeurotic plane is avascular and contains no crossing blood vessels. It is continuous superiorly with the subgaleal plane, which extends inferiorly to overlie the zygomatic arch.
The deep temporal fascia is a thick, dense, connective-tissue layer overlying the temporalis muscle. Superiorly it is in intimate contact with the temporalis muscle and exists as a single layer. Although it is a single sheet of fascia, it can be split by careful dissection into two separate layers.
Below the level of the superior orbital margin is the temporal line of fusion where the deep temporal fascia splits into two separate sheets of fascia, a thick outer layer and a thinner deep layer. Continuing inferiorly to the zygomatic arch, the two layers of deep temporal fascia remain separated from each other by a fat pad. This fat pad is the superficial temporal fat pad or Yasargil fat pad. The Yasargil fat pad is enveloped by the two layers of the deep temporal fascia and extends from the temporal line of fusion down to the zygomatic arch and as far forward as the lateral orbital wall.
The temporalis is covered by the deep layer of the deep temporal fascia. The buccal fat pad traverses upward beneath the zygomatic arch and extends as the deep temporal fat pad, overlying the inferior portion of the temporalis muscle and its tendon over approximately 2-4 cm above the zygomatic arch.
The deep temporal fascia is adherent to the periosteum at the superficial temporal crest line. At this point, the superficial temporal fascia joins the galea. This fascial junction is termed the conjoint fascia or the conjoint tendon and needs to be divided effectively by sharp or blunt dissection when performing a forehead elevation in the subperiosteal plane. [10]
For more information about the relevant anatomy, see Scalp Anatomy, Forehead Anatomy, Facial Nerve Anatomy, and Facial Anatomy in Cutaneous Surgery.
Contraindications
Patients without forehead furrows may be poor candidates for the mid forehead approach. Furthermore, even in the presence of reasonably impressive mid forehead furrows, scars can be significant, and before and after photographs must be shown to the patient to ensure that he or she is willing to accept the ensuing scars. The procedure is also contraindicated in patients with low frontal hairlines.
Finally, with advances in endoscopic techniques, many patients who would previous have undergone mid forehead lifts now are operated on using modified endoscopic techniques. [11] The aim in all functional or cosmetic forehead lifts is to achieve the desired repositioning of the brows and the forehead with minimal visible scarring.
-
Mid forehead brow lift. Transverse forehead incisions may be broken as shown to improve the appearance of the final result. Courtesy of Bhupendra Patel, MD, FRCS.
-
Mid forehead brow lift. Dissection is performed in the subcutaneous plane. Courtesy of Bhupendra Patel, MD, FRCS.
-
Mid forehead brow lift. Transverse incisions are made in the galea to access the corrugator and procerus muscles. These incisions are kept in the middle to prevent injury to the supraorbital nerve branches. Courtesy of Bhupendra Patel, MD, FRCS.
-
Mid forehead brow lift. Once exposed, the corrugator and procerus muscles are attenuated. Courtesy of Bhupendra Patel, MD, FRCS.
-
Mid forehead brow lift. The galea is shortened as desired and sutures are placed. Courtesy of Bhupendra Patel, MD, FRCS.
-
Mid forehead brow lift. Elevation of the cutaneous structures is obtained and appropriate trimming is performed. Courtesy of Bhupendra Patel, MD, FRCS.
-
Mid forehead brow lift. Meticulous subcuticular closure is achieved with no tension on the skin edges. Courtesy of Bhupendra Patel, MD, FRCS.
-
Several different incisions for mid forehead lifts have been proposed. Here, incisions are placed at different heights to prevent a long horizontal scar. Courtesy of Bhupendra Patel, MD, FRCS.
-
Mid forehead brow lift. Preoperative. A 68-year-old man with markedly overactive corrugator and procerus muscles. Note the particularly heavy sebaceous forehead skin and evidence of long standing overactivity of the orbital orbicularis oculi muscles, all conspiring to create a particularly menacing appearance. Such a patient would not do well with an endoscopic forehead lift. Courtesy of Bhupendra Patel, MD, FRCS.
-
Mid forehead brow lift. Postoperative. Note that even 5 months following the repair, some pinkness of the incision site is present. When a patient has a great degree of actinic keratosis and secondary telangiectatic vessels, such as in this man, such persistent pinkness in the incision site is not uncommon. However, a reasonable elevation of his brows and weakening of his uncommonly powerful corrugator and procerus muscles has been achieved. Courtesy of Bhupendra Patel, MD, FRCS.
-
Coronal section of scalp that shows layers of the scalp.
-
Diagram of the sensory and motor supply of the face.