Practice Essentials
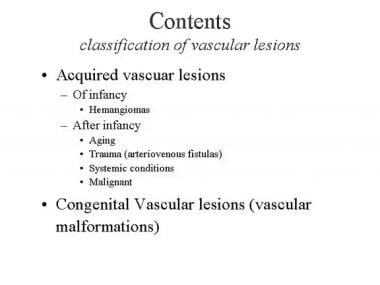
Vascular lesions of the skin are divided into congenital and acquired lesions. A classification of vascular lesions is shown in the image below.
Acquired and congenital vascular lesions are described as follows:
-
Acquired vascular lesions: The most significant acquired vascular lesions of infancy are hemangiomas. [1, 2] The lesions are composed of proliferating blood vessels and, although benign, have a potentially destructive character. Hemangiomas undergo a proliferative and an involution stage. Pyogenic granuloma is another acquired vascular lesion that is frequently observed during childhood. It is of minor aesthetic significance compared to hemangiomas. [3] After infancy, acquired vascular lesions are associated with aging (senile angiomas), trauma (arteriovenous fistulas), systemic conditions (spider angioma), and malignancy (Kaposi sarcoma).
-
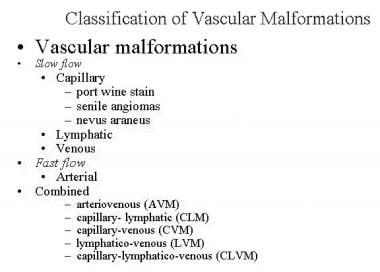
Congenital vascular lesions: The most common congenital vascular lesions are vascular malformations. Vascular malformations are the outcome of errors in vascular formation during embryonic life. They do not proliferate. The dilated blood vessels that build up these lesions gradually enlarge. Vascular malformations can be classified based on their type of blood flow into slow-flow lesions (capillary, venous, lymphatic), high-flow lesions (arterial), and lesions with a combined slow and fast blood flow (see the image below).
The nomenclature of vascular lesions is confusing, and one may find perplexing terms such as "capillary hemangiomas" in some textbooks. Terms such as "strawberry hemangiomas" for superficial lesions and "cavernous hemangiomas" for deep lesions are puzzling and probably should not be used. Instead, hemangiomas should be classified as superficial, deep, or mixed type, according to their location in the skin and subcutaneous tissue. The classification presented here is based on the type of blood vessel, type of flow, and clinical presentation of the lesion. [1] Exceptions are found to this classification; some hemangiomas are congenital, [4] and some vascular malformations are not present at birth. Congenital hemangiomas are discussed in the Outcome and Prognosis section.
Workup of hemangiomas
Imaging studies
The most important imaging tool for this condition is contrast-enhanced magnetic resonance imaging (MRI). [5, 6] This diagnostic test, which requires sedation or general anesthesia for children younger than 6 years, demonstrates the extent of the lesion and helps differentiate between hemangiomas and venous, lymphatic, and arterial lesions. It may also help differentiate between a vascular lesion and nonvascular lesions, such as those found in neurofibromatosis.
Doppler ultrasonography can assess the flow of hemangiomas. [7]
Histologic findings
These include the following{ref3 [8] :
-
Proliferating hemangiomas are composed of clusters of rapidly dividing endothelial cells
-
With regression, the cells flatten and mature
-
Mast cells appear in the late proliferating phase and early involuting phase
-
During involution, light microscopy demonstrates progressive deposition of perivascular and interlobular/intralobular fibrous tissue
-
Multilaminated basement membranes persist in the involuted phase
Management of hemangiomas
Medical therapy
-
Local antibiotic ointment or wet-to-dry dressing - Useful to clear the debris and decrease the likelihood of local infection during the involution stage when the lesion becomes ulcerated
-
Pressure garment
-
Recombinant interferon alfa-2a - May be indicated in patients in whom steroids are contraindicated or not effective [11]
-
Flash lamp pulsed dye laser - Has a moderate lightening effect on the capillary discoloration of hemangiomas
-
Intralesional fiber with the potassium-titanyl-phosphate (KTP) laser - Was demonstrated to induce involution of voluminous hemangiomas of the face and neck regions; [12, 13] intralesional photocoagulation treatment with the KTP and neodymium-doped yttrium aluminum garnet (Nd:YAG) lasers was also found to be effective and safe for the treatment of periorbital hemangiomas [14]
-
Carbon dioxide laser - Useful for treating subglottic hemangiomas; it may also be useful for resurfacing residual minor skin irregularities
-
Superselective catheterization and embolization - Infrequently used to treat hemangiomas with a defined nourishing artery
Surgical therapy
Surgical therapy may be considered in several circumstances, including the following:
-
When intraoperative and postoperative bleeding can be controlled
-
When surgery does not place an organ at risk (eg, injury to the eye or facial nerve)
-
When the expected aesthetic and/or functional outcomes of the procedure are similar to or superior to the aesthetic outcome of spontaneous involution
-
When the aesthetic and/or functional outcomes of the procedure are inferior to the predicted outcome of spontaneous involution and the psychosocial effect on the child having to live through childhood with a disfiguring deformity is significant
Epidemiology
Frequency
Approximately 80% of hemangiomas grow as a single tumor, [15] and 20% proliferate in multiple sites. Hemangiomas are far more common in females than in males, with a female-to-male ratio of 3-5:1. The incidence in white infants is 10-12% and is 22% in preterm infants who weigh less than 1000 g. The incidence is lower in infants with darker skin. [15] Prenatal associations include older maternal age, placenta previa, and preeclampsia. [16]
Etiology
Formation and remodeling of blood vessels are controlled generally by paracrine signals, many of which are protein ligands that bind and modulate transmembrane receptor tyrosine kinases. [17] Negative regulators include angiostatin, Endostatin, and thrombospondin. Among the positive regulators are vascular endothelial growth factor (VEGF), fibronectin, 5-integrin, vascular endothelial cadherin, and transforming growth factor-1 (TGF-1). [17, 18]
Several studies indicate that hemangiomas are the outcome of an angiogenic growth factor effect. [17, 19, 20] Basic fibroblast growth factor (bFGF) and VEGF messenger RNAs are up-regulated in proliferative hemangiomas. [21] TGF-β 1 messenger RNA remains low in both proliferative and involuted hemangiomas. [19] VEGF is localized predominantly in pericytes and endothelial cells during the proliferative phase. [20] bFGF is found in endothelial cells in both the proliferative and early involutional phases. [20] Other studies indicate that the angiogenic peptide, bFGF, is elevated in the urine of infants with proliferating hemangiomas. [15] Its levels subsequently diminish and return to normal during natural involution or during accelerated regression induced by antiangiogenic therapy. In contrast, in patients with vascular malformations, normal concentrations of bFGF are found in the urine. [15]
Pathophysiology
See Etiology.
Presentation
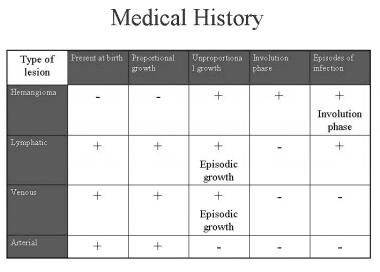
Diagnosis of a vascular lesion is based on the medical history, physical examination, and imaging. The type of lesion can usually be determined based on the first 2 items. Imaging is mostly useful for confirming the clinical diagnosis, estimating the extent of the lesion, and determining the feasibility of surgical resection.
Medical history
Medical history is described in the image below.
When obtaining the medical history, ask the following 4 questions:
-
Was the lesion present at birth?
-
Did proportional or disproportional growth of the lesion occur after birth?
-
Did a phase of involution occur?
-
Has an episodic enlargement occurred at any point?
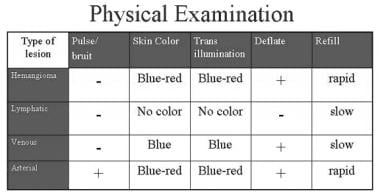
Physical examination
Physical examination of a patient with a vascular lesion includes inspection, palpation, and transillumination.
A complete body examination should be performed to exclude syndromes that include skin hemangiomas. One such syndrome is neonatal hemangiomatosis, which refers to infants with multiple cutaneous hemangiomas. Such patients may have intrahepatic hemangiomas that can cause congestive heart failure (CHF), hepatomegaly, and anemia. [15]
Hemangiomas may be associated with other underlying conditions; lumbosacral hemangiomas may be overlying an occult spinal dysraphism as a tethered cord, lipomeningocele, and diastematomyelia. Facial hemangioma may be associated with posterior fossa abnormality, malformations of great arteries, and ocular abnormalities. PHACE syndrome is the association of Posterior fossa malformations, Hemangiomas, Arterial abnormalities, Coarctation of the aorta, and Eye abnormalitieS. [22] Subglottic hemangioma should be suspected in an infant with a facial hemangioma who presents with dyspnea and stridor.
Differential diagnosis
Hemangiomas may be confused with deep lymphatic or venous vascular malformations. The presence of the lesion at birth supports a diagnosis of a vascular malformation, although congenital hemangiomas are observed at birth. MRI can help distinguish between a vascular malformation and a hemangioma. The differential diagnosis also includes gliomas and other benign and malignant tumors. The first image below shows a 1-year-old girl who presented with a 3-month history of a right facial lump. The lesion was initially managed as a hemangioma. However, MRI indicated that this was not a vascular lesion, and excisional biopsy through an upper buccal incision disclosed nodular fasciitis. The second image below shows the differential diagnosis of orbital hemangioma.
Pyogenic granuloma, which is also one of the most common acquired vascular lesions of childhood, has a typical history of a nonhealing and occasionally bleeding wound. It has a growth phase similar to that of hemangiomas but is usually much smaller and may appear after the first year of life. [3]
Indications
Most hemangiomas do not require treatment. They regress spontaneously by the time the individual is aged 10-12 years. [15]
Indications for early intervention are primarily functional, such as obscuration of vision or breathing difficulties.
Uncontrolled bleeding and pain caused by an ulcerated hemangioma may also be an indication for intervention (see the images below). Facial hemangiomas, especially aggressive, rapidly spreading hemangiomas, may necessitate early pharmacologic or surgical intervention to decrease the long-term aesthetic deformity (see the first image below). Very large hemangiomas may be associated with platelet trapping, thus requiring early intervention.
Parental concerns and psychosocial effects of the deformity on the growing child should also be taken into consideration and may warrant earlier treatment. The indications for treatment and a regional approach to the management of facial hemangiomas are presented in Surgical therapy.
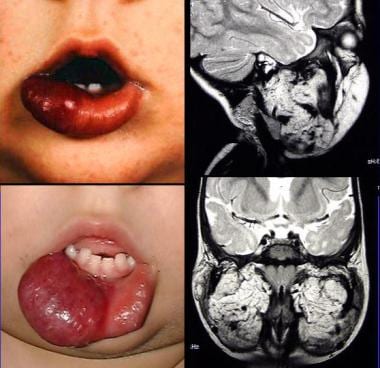
Relevant Anatomy
Hemangiomas are composed of abnormal vessels located at the skin and/or subcutaneous tissue. The lesion can extend far beyond the skin and invade adjacent structures such as the floor of the mouth and the cheek muscles. The image below shows a lower lip hemangioma in an infant aged 6 months (upper left) and following proliferation at age 16 months (lower left). MRI shows extension of the lesion into the floor of the mouth and cheek.
Contraindications
Surgical therapy may be contraindicated in several circumstances, including the following:
-
Intraoperative and postoperative bleeding cannot be controlled.
-
Surgery places an organ at risk (eg, injury to the eye or facial nerve).
-
Expected aesthetic and/or functional outcomes of the procedure are similar or inferior to the aesthetic outcome of spontaneous involution.
-
Aesthetic and/or functional outcomes of the procedure are similar to the predicted outcome of spontaneous involution and the psychosocial effect on the child living through childhood with a disfiguring deformity is not significant.
-
Hemangiomas. Classification of vascular lesions.
-
Hemangiomas. Classification of vascular malformations.
-
Hemangiomas. Diagnosis - Medical history.
-
Hemangiomas. Diagnosis - Physical examination.
-
Deep cheek hemangiomas.
-
Superficial cheek hemangiomas.
-
Upper lip hemangiomas.
-
Treatment with steroids of orbital hemangioma.
-
Panfacial hemangiomas.
-
Resection of a bleeding forehead hemangioma.
-
Lower lip hemangioma with intraoral extension.
-
Hemangiomas. Relaxation time - MRI T1, T2.
-
Hemangiomas. Diagnosis MRI.
-
Left orbital hemangioma.
-
MRI of orbital hemangioma.
-
Proliferating hemangioma - Light microscopy.
-
Hemangiomas. Facial nodular fasciitis misdiagnosed as a vascular lesion.
-
Differential diagnosis of orbital hemangiomas.
-
The effect of compression on a chest hemangioma.
-
Use of a bicoronal approach to resect a forehead hemangioma.
-
Types of nasal hemangiomas.
-
Resection and primary closure of a nasal bridge hemangioma.
-
Open rhinoplasty approach to resect a nasal tip hemangioma.
-
Lower lip hemangioma.