Background
Patients with large breasts experience a significant range of symptoms, some severe enough to interfere with activities of daily living. Patients with large heavy breasts commonly report significant neck and shoulder pain. They may develop grooves in their shoulders from the weight of their bra straps, experience difficulty wearing clothes, and find that the heaviness of their breasts interferes with sports activities. Some patients have even had to eliminate some activities from their lives because their large breasts get in their way. [1, 2]
Patients may present to plastic surgeons for reduction mammoplasty starting at puberty. If reduction mammoplasty is performed at an early age, such as age 14 years, the patient should be advised that she may require an additional procedure at a later time. If breasts are significantly large, surgery should be considered in the teenage years so the teenager's activities are not restricted, nor is she harassed.
The true genetics of breast development are not known. Even within the same family, one sister may have small breasts, while the other has large breasts.
This article addresses the inferior pedicle technique (see image below) for breast reduction, which is an alternative to free nipple and areola grafting. [3]
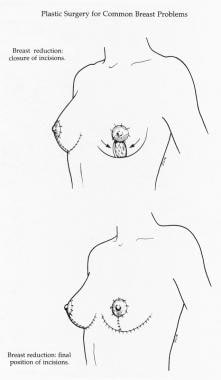 Breast reduction, inferior pedicle. Closure of incisions (top). Final position of incisions (bottom). Used with permission from Downey SE. Plastic Surgery for Common Breast Problems. In: Hindle WH, ed. Breast Care: A Clinical Guidebook for Women's Primary Health Care Providers. New York: Springer-Verlag New York Inc; 1999.
Breast reduction, inferior pedicle. Closure of incisions (top). Final position of incisions (bottom). Used with permission from Downey SE. Plastic Surgery for Common Breast Problems. In: Hindle WH, ed. Breast Care: A Clinical Guidebook for Women's Primary Health Care Providers. New York: Springer-Verlag New York Inc; 1999.
For details on other techniques, visit the Breast section of Medscape’s Plastic Surgery journal.
Indications
In general, a patient is considered a candidate for breast reduction if the size and weight of her breasts cause her significant neck and shoulder pain. Criteria have been established by some insurance companies as to the amount to be removed from each breast according to a patient's height and weight. More recently, however, insurance companies have relied more heavily on symptomatology, such as neck and shoulder pain, to approve the surgery. Small reductions in which the breasts are not reduced by at least 2 cup sizes are not usually covered by insurance and would likely be considered a breast lift or mastopexy.
Relevant Anatomy
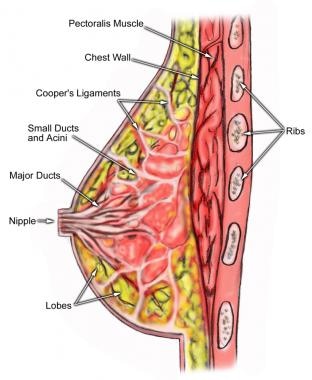
Breast shape varies among patients, but knowing and understanding the anatomy of the breast (see image below) ensures safe surgical planning. When the breasts are carefully examined, significant asymmetries are revealed in most patients. Any preexisting asymmetries, spinal curvature, or chest wall deformities must be recognized and demonstrated to the patient, as these may be difficult to correct and can become noticeable in the postoperative period. Preoperative photographs with multiple views are obtained on all patients and maintained as part of the office record.
For more information about the relevant anatomy, see Breast Anatomy.
Contraindications
The only real contraindication to breast reduction surgery is if the patient is not medically able to undergo the surgery.
Scars are the main risk that should be discussed with the patient. The scars from this procedure extend around the nipple-areolar complex (NAC), vertically between the NAC and the inframammary fold (IMF), and under the IMF. The scars are placed such that the scar around the NAC blends in when the color change occurs. The wound under the breast is placed under the fold to be hidden by the natural overhang of the breast. Fortunately, the vertical component of the scar tends to heal very well, even in patients who may form hypertrophic or very noticeable scars elsewhere.
Keloids are a risk in some patients. The most common place for keloid formation is in the IMF, principally in the medial portion. Patients who have a history of keloids should be warned of the risk for keloid formation. However, in general, the scars respond to steroid injection and pressure.
Patients with extremely large breasts have a higher risk of problems, principally loss of the NAC. This risk is almost negligible in women with smaller breasts; if these women smoke cigarettes, the risk is increased. In women with extremely large breasts, the possibility of a conversion to a free nipple graft should be discussed with the patient.
However, a retrospective study of a single surgeon’s experience indicated that the pedicled Robertson mammoplasty, an inferior pedicle technique involving a curvilinear skin extension onto the pedicle, is a safe and effective means of breast reduction in patients who are obese and have extreme macromastia. Patients in the report had a mean body mass index (BMI) of 36.45 kg/m2, with the mean resection weight being 1859.2 grams per breast and the sternal notch to nipple distance extending a mean 41.4 cm. No nipple necrosis occurred in association with the Robertson surgery, and no major complications leading to reoperation under general anesthesia arose. Minor complications requiring either local wound care or small office procedures occurred in 26.4% of patients, with 4.4% of patients undergoing small revisions under local anesthesia. [4]
The possibility of loss of nipple sensation exists in reduction mammaplasty, as does possible loss of the ability to breastfeed. Women have successfully breastfed following reduction mammoplasty, but patients should be warned that this may not be possible. In general, if loss of nipple sensation does occur, it usually improves over the course of the year or so following surgery.
A prospective, nonrandomized study by Muslu et al indicated that inferior pedicle breast reduction is a safe technique with regard to sensory changes. Although reduced skin sensation was found in the upper medial and lower lateral portions of the breast in women who underwent the procedure, a reduction that did not occur with superomedial pedicle breast reduction, the investigators found that neither the inferior nor the superomedial pedicle surgeries led to changes in the two-point discrimination test on the areola. [5]
-
Breast reduction. Markings and preoperative assessment. Used with permission from Downey SE. Plastic Surgery for Common Breast Problems. In: Hindle WH, ed. Breast Care: A Clinical Guidebook for Women's Primary Health Care Providers. New York: Springer-Verlag New York Inc; 1999.
-
Breast reduction, inferior pedicle. Closure of incisions (top). Final position of incisions (bottom). Used with permission from Downey SE. Plastic Surgery for Common Breast Problems. In: Hindle WH, ed. Breast Care: A Clinical Guidebook for Women's Primary Health Care Providers. New York: Springer-Verlag New York Inc; 1999.
-
Anatomy of the breast.