Practice Essentials
Hepatitis A is caused by hepatitis A virus (HAV), a positive-sense, single-stranded, nonenveloped RNA virus that belongs to the Picornaviridae family and the Hepatovirus genus. After fecal-oral transmission, the virus is then excreted into the bile. Its concentration is highest in the stool, especially during the 2 weeks preceding the onset of jaundice. This correlates with the period of peak infectivity. Children and adults can be assumed to be noninfectious 1 week after the appearance of jaundice.
Signs and symptoms of hepatitis A
The initial symptoms during the prodromal period include low-grade fever, nausea, vomiting, decreased appetite, and abdominal pain. Older children and adults are more likely to report pain in the right upper quadrant. Diarrhea may occur in young children. Two thirds of symptomatic patients have clinical jaundice.
See Presentation for more detail.
Diagnosis of hepatitis A
Liver inflammation during HAV infection can be detected by elevations in alanine aminotransferase (ALT), aspartate aminotransferase (AST), and gamma-glutamyltranspeptidase (GGTP) levels. Increases in ALT and AST levels are observed most consistently, and the values are usually 4-100 times the normal levels.
Although ultrasonography of the liver may be helpful when cholelithiasis is a consideration, imaging studies are generally not necessary.
See Workup for more detail.
Treatment of hepatitis A
No specific therapy is available. Treatment is therefore supportive.
Vaccination is indicated for primary immunization to prevent hepatitis A. It is also used for postexposure prophylaxis, either alone or in conjunction with immune globulin.
See Treatment and Medication for more detail.
Background
The earliest description of an illness consistent with viral hepatitis dates back to the second century. During the centuries that followed, epidemics of jaundice were reported, and outbreaks plagued military campaigns, both ancient and modern.
In the 1920s, a viral etiology was suggested for what was then known as infectious hepatitis. Various viral agents were isolated from urine, blood, and stool from patients with hepatitis in the first half of the 20th century; however, the 27 nm particles of the HAV were not described until 1973. [1]
This finding led to the development of serologic testing and, more recently, molecular techniques, such as polymerase chain reaction (PCR). These events resulted in greater knowledge of the epidemiology, transmission, and infectivity of HAV, as well as in the development of preventive measures, including active and passive immunization. Hepatitis A is now the target of routine childhood immunizations, starting at age 1 year (see Recommendations Updated for Universal Administration of Hepatitis A Vaccination in US Children).
Go to Hepatitis A, Pediatric Hepatitis B, Pediatric Hepatitis C, and Viral Hepatitis for complete information on these topics.
Pathophysiology
HAV infection is transmitted via the fecal-oral route, and viral replication occurs in the liver, leading to hepatic injury. The entire liver exhibits necrosis, which is most marked in the centrilobular areas, as well as increased cellularity in the portal areas. The regional lymph nodes and spleen may become enlarged. Liver injury is represented in 3 ways:
-
Direct cellular injury that elevates serum liver enzyme levels
-
Cholestasis that causes jaundice and hyperbilirubinemia
-
Inadequate liver function that lowers serum albumin levels and prolongs the prothrombin time (PT)
Etiology
Common-source outbreaks of hepatitis A from contaminated food or water may occur. [2] HAV is concentrated in filter-feeding shellfish, which may thrive close to sewage outlets, and widespread outbreaks can occur from a single contaminated source, such as uncooked vegetables that are distributed to restaurants or grocery stores. Statistically, eating out is actually less risky than home cooking.
Childcare centers may be sources of outbreaks from contaminated changing tables. These outbreaks may not be identified until an adult contact has a recognizable HAV infection, because young children are often asymptomatic or have anicteric illnesses.
Nosocomial outbreaks have occurred because of HAV shedding. Outbreaks of HAV infection have been increasingly reported among illicit drug users. International travel is another risk factor for HAV infection.
Vertical transmission of HAV (ie, from mother to neonate) and transmission by means of blood transfusion are extremely rare. Sexual transmission is possible, especially between men who have sex with men. Spread of HAV from nonhuman primates to humans has been reported.
Epidemiology
United States statistics
In 2006, the national annual incidence in the United States was 1.2 cases per 100,000 population (see the image below). [3] Before vaccination became widespread, rates were higher than 9 cases per 100,000 population. [4]
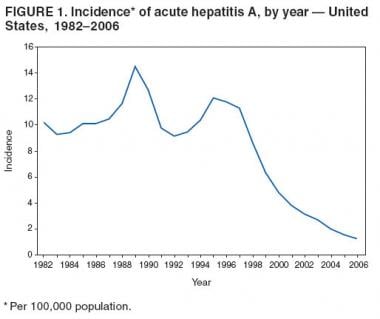 Incidence of acute hepatitis A virus in the United States from 1982-2006. (Image from "Surveillance for Acute Viral Hepatitis --- United States, 2006." MMWR March 21, 2008. 57(SS02);1-24)
Incidence of acute hepatitis A virus in the United States from 1982-2006. (Image from "Surveillance for Acute Viral Hepatitis --- United States, 2006." MMWR March 21, 2008. 57(SS02);1-24)
By 2011, the yearly number of cases of HAV infection in the United States had decreased to 1398. However, between 2016 and 2018, an estimated 15,000 cases of HAV infection were reported. These cases were generally related to outbreaks associated with homelessness and illicit drug use. Other outbreaks during this period occurred among men who have sex with men or were associated with foodborne transmission. [5]
Nearly one-third of adults have serologic evidence of prior HAV infection. Higher rates are associated with lower socioeconomic status, crowding, and poor sanitation. Outbreaks may occur in association with poor food hygiene or undercooked food.
International statistics
In developing countries, infection is highly endemic; nearly 100% of the population in some countries has serologic evidence of past HAV disease during childhood.
In a surveillance study of 1156 HAV cases from 6 sites in the United States’ Emerging Infections Program, from 2005 through 2007, the majority of infections were due to international travel or exposure to travelers. Many of the cases that implicated travel or contact with travelers as a risk factor involved travel to Mexico. [6]
Age-related differences in incidence
In the United States, prior to targeted vaccination programs, the highest rate of infection occurred in children aged 5-14 years. Since the advent of widespread vaccination, as many as 80% of infections have been in adults. Interestingly, the classic symptoms of hepatitis are less likely in younger patients. Young children, especially those younger than 5 years, may be asymptomatic or may have anicteric illness that appears to be a nonspecific viral infection.
Sex-related demographics
HAV has no sex predilection. Homosexual males may have a higher risk of infection than heterosexual males.
Race-related demographics
Before targeted vaccination programs, certain well-defined populations were considered high-risk groups, including Native Americans, Alaskan natives, and some Hispanic people. Epidemics occurred in these groups every 5-10 years, as susceptible people entered or were born into the population. In addition, overall rates of infection in nonepidemic years were also greater in these populations than in the United States as a whole.
Since 2003, racial and ethnic differences have virtually disappeared. For example, a nearly 99% decrease was noted in the incidence of HAV among Native Americans as the result of a widespread targeted vaccination campaign among high-risk groups.
Prognosis
The prognosis is excellent. In most patients, HAV infection is self-limited, and complete recovery occurs. In fact, many cases are asymptomatic. Except in the setting of fulminant hepatitis, sequelae are rare. Fulminant hepatitis due to HAV is uncommon and has a case-fatality rate of 0.4%.
Relapsing HAV infection occurs in approximately 10% of patients 1-4 months after the initial episode and results in full recovery.
Chronic active hepatitis, which can be seen in hepatitis B virus (HBV) or hepatitis C virus (HCV) infection, does not occur in HAV infection. A chronic carrier state is not seen with HAV infection.
Complications
Complications are few. Fulminant hepatitis with massive hepatic necrosis and liver failure due to HAV infection is rare. Cholestatic hepatitis occurs in a small percentage of patients. It is identified by persistent hyperbilirubinemia, pruritus, and constitutional symptoms that last for 12-16 weeks in the absence of biliary obstruction on sonograms.
Patient Education
Patients and parents should be educated regarding the transmission of HAV and instructed in proper hygiene. Indications for postexposure prophylaxis should be explained, and affected individuals should be identified and treated appropriately. Local and state health departments are instrumental in epidemiologic identification of the appropriate contacts who need postexposure prophylaxis.
Physicians should be prepared to explain transmission and prevention issues to the staff at the patient’s school and childcare center. This can help identify individuals who may need prophylaxis, as well as alleviate unnecessary worries for those who are not at risk.
For patient education resources, see the Hepatitis Center and the Liver, Gallbladder, and Pancreas Center, as well as Hepatitis A.
-
Incidence of acute hepatitis A virus in the United States from 1982-2006. (Image from "Surveillance for Acute Viral Hepatitis --- United States, 2006." MMWR March 21, 2008. 57(SS02);1-24)








