Practice Essentials
Adipsia is a disease characterized by the absence of thirst even in the presence of body water depletion or salt excess. It is a rare condition that typically presents as hypernatremic dehydration. [1] The cause is usually a hypothalamic lesion, which can be congenital or acquired. The term hypodipsia refers to a partial deficiency of the thirst mechanism. See the image below.
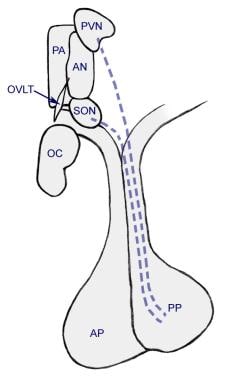 Anatomic relationships between pituitary and hypothalamic areas of interest with respect to regulation of antidiuretic hormone (ADH) secretion and thirst sensation. AN = Anterior (hypothalamic) nucleus; AP = Anterior pituitary; OC = optic chiasm; OVLT = Organum vasculosum of lamina terminalis; PA = Preoptic (hypothalamic) area; PP = Posterior pituitary; PVN = Paraventricular (hypothalamic) nucleus; SON = Supraoptic (hypothalamic) nucleus.
Anatomic relationships between pituitary and hypothalamic areas of interest with respect to regulation of antidiuretic hormone (ADH) secretion and thirst sensation. AN = Anterior (hypothalamic) nucleus; AP = Anterior pituitary; OC = optic chiasm; OVLT = Organum vasculosum of lamina terminalis; PA = Preoptic (hypothalamic) area; PP = Posterior pituitary; PVN = Paraventricular (hypothalamic) nucleus; SON = Supraoptic (hypothalamic) nucleus.
Pathophysiology
In humans, the thirst center is located in the hypothalamus. The primary physiological stimuli for thirst are hypertonicity (osmotic) and hypovolemia. After infancy, an additional social stimulus for thirst is usually observed, which is viewed as secondary.
Osmoreceptors in the anterior wall of the third ventricle, near the organum vasculosum mediate the osmotic regulation of thirst, near to or even common to the osmoreceptors that regulate secretion of aqueous vasopressin (AVP). This stimulus is known as osmotic thirst. [2]
In general, the threshold for AVP secretion is a small increase in serum osmolality from 280-290 mOsm/kg H2 O. In contrast, the stimulus for osmotic thirst stimulation is set much higher, typically when near-maximal urine concentrations are achieved (ie, at serum osmolalities around 295 mOsm/Kg H2 O). The purpose of this dichotomy appears to be so that thirst can act as a back up mechanism, when pituitary and renal mechanisms are insufficient to keep plasma osmolality within a tight 1-2% range. If thirst were the primary system, humans would need to constantly divert attention towards seeking water.
After activation of osmotic thirst, downregulation of this stimulus occurs in 2 phases: (1) an immediate but short-lived downregulation of thirst by the oropharynx and upper GI tract and (2) a less immediate but more sustained downregulation by drop in serum osmolality (negative feedback).
Hypovolemia and hypotension may also stimulate thirst through the activation of low-pressure (venous) and high-pressure (arterial) vascular stretch receptors (hypovolemic thirst). Impulses from these receptors are transmitted by the vagus and the glossopharyngeal nerves to the medulla and from there to the hypothalamus. In addition, the hypothalamus is directly stimulated by angiotensin II. Such a hypovolemic thirst occurs with depletion of plasma volume by at least 4-8% in humans and 10-15% in some species.
Thirst abnormalities may result either from specific functional lesions that impair the activation of thirst by hypertonicity or hypovolemia or from generalized lesions that impair the cognitive processes required for thirst perception.
Any lesion, congenital or acquired, that affects the anterior hypothalamus may lead to the abolition of thirst. Because the center for AVP secretion occupies a contiguous area, lesions of the thirst center may also affect AVP (also known as antidiuretic hormone [ADH]) production, storage, or secretion), leading to impaired urinary concentrating ability. Therefore, patients may present with a combination of adipsia and central diabetes insipidus (ie, absence of AVP secretion), also known as adipsic diabetes insipidus. [3, 4] Such patients can develop severe hypernatremia, though it is chronic and therefore asymptomatic in many cases. [5] However, these patients have a much higher risk of infection and death. [6] . In adipsia, AVP secretion may be either completely unaffected, partially abolished, or completely abolished. In a normal situation, AVP acts along with thirst to maintain serum osmolality within tight control.
In rats, areas within the caudate nucleus appear to regulate water intake through norepinephrine-sensitive alpha receptors. [7] In a single case report in a dog, antithyroid antibodies led to hypothyroidism and adipsia, both of which resolved with levothyroxine therapy. [8] "Sickness behavior" is a condition in animals in which systemic infection leads to a highly regulated set of responses such as fever, anorexia, adipsia, inactivity, and cachexia. The neuroimmune communication may involve the interaction of cytokines with peripheral nerves. [9] In rat models, lipopolysaccharide is used to induce adipsia as part of sickness behavior. [10]
Although many different diseases can affect the anterior hypothalamus, adipsia is seen very infrequently even among patients with known anterior hypothalamic lesions. The reason adipsia is uncommon in such situations and the instances when adipsia is more likely to occur remain unknown.
Rarely, some children have adipsia without a definable structural lesion (essential adipsia). [11, 12, 13] A constellation of adipsia, obesity, hyperprolactinemia, and hypothyroidism was reported in one child. [13]
In hypodipsia, the exact pathological abnormalities are not known. AVP levels are normal, suggesting that neuronal pathways affecting thirst are selectively affected, either at the osmoreceptor level or further downstream.
Etiology
The most common neoplastic lesions associated with adipsia are germinomas, [14] histiocytomas, and gliomas.
Congenital lesions that are associated with adipsia include the following:
-
Microcephaly
-
Ectrodactyly-ectodermal dysplasia-cleft lip/palate (EEC) syndrome
-
Empty sella syndrome
-
Malformation of the septum pellucidum
-
Holoprosencephaly
The following can also produce adipsia:
-
Meningoencephalitis
-
Subarachnoid hemorrhage
-
Hydrocephalus
-
Pseudotumor cerebri
-
Psychogenic abnormalities [15]
Epidemiology
International statistics
Adipsia is an extremely rare condition. Fewer than 200 cases have been reported worldwide, although more cases are likely unreported. Mavrakis et al collated and described 70 reported cases in which thirst and AVP secretion were both abolished. [16]
Interestingly, a number of cases are reported in the veterinary literature, largely due to intracranial tumors, similar to causes in humans.
Age-related demographics
Adipsia occurs in all age groups. Congenital malformations and traumatic lesions predominate in children, neoplastic lesions occur in all age groups, and psychogenic causes are more common in adults, particularly elderly persons. In children, adipsia without demonstrable structural lesions is very rare and has been reported in only 6-7 patients. [17]
Prognosis
Prognosis is unfavorable unless behavioral therapy is successful. Most patients remain homebound or institutionalized and may develop further neurological handicaps.
Morbidity/mortality
Adipsia leads to considerable difficulty in the management of water balance. Its common consequence is hypernatremic dehydration, which, when severe, is associated with hemodynamic and CNS manifestations. Adipsia has a higher morbidity than diabetes insipidus, in which the thirst mechanism is intact. [18]
Complications
Existing neurological deficits can be exacerbated by acute episodes of severe hypernatremia and cerebral hemorrhage.
Extrarenal losses of volume during episodes of gastroenteritis, more common in children, may lead to rehospitalization for worsening hypernatremia or other disorders of serum electrolytes.
-
Anatomic relationships between pituitary and hypothalamic areas of interest with respect to regulation of antidiuretic hormone (ADH) secretion and thirst sensation. AN = Anterior (hypothalamic) nucleus; AP = Anterior pituitary; OC = optic chiasm; OVLT = Organum vasculosum of lamina terminalis; PA = Preoptic (hypothalamic) area; PP = Posterior pituitary; PVN = Paraventricular (hypothalamic) nucleus; SON = Supraoptic (hypothalamic) nucleus.



