Background
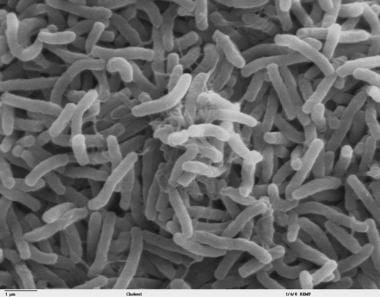
Cholera is an intestinal infection caused by Vibrio cholerae (see the images below). The hallmark of the disease is profuse secretory diarrhea. Cholera can be endemic, epidemic, or pandemic. Despite all the major advances in research, the condition still remains a challenge to the modern medical world. Although the disease may be asymptomatic or mild, severe cholera can cause dehydration and death within hours of onset.
See 11 Travel Diseases to Consider Before and After the Trip, a Critical Images slideshow, to help identify and manage infectious travel diseases.
Cholera is transmitted by the fecal-oral route. In the United States and other developed countries, because of advanced water and sanitation systems, cholera is not a major threat. Nevertheless, both clinicians and members of the general public, especially travelers, should be aware of how the disease is transmitted and what can be done to prevent it. [1]
Definitive diagnosis is not a prerequisite for the treatment of patients with cholera. The priority in management of any watery diarrhea is replacing the lost fluid and electrolytes and providing an antimicrobial agent when indicated. (See Workup and Treatment.)
Historical background
Cholera is an ancient disease. Throughout history, populations all over the world have sporadically been affected by devastating outbreaks of cholera. Records from Hippocrates (460-377 BCE) and the Indian peninsula describe an illness that might have been cholera
The 19th century English physician John Snow provided the first demonstration that the transmission of cholera was significantly reduced when uncontaminated water was provided to the population. During a recurrent epidemic of cholera in London in 1854, Snow identified water from the Broad Street pump as the likely source of the disease; removal of the pump handle contained the epidemic. [2]
Although not the first description, the discovery of the cholera organism is credited to German bacteriologist Robert Koch, who independently identified V cholerae in 1883 during an outbreak in Egypt. The genus name refers to the fact that the organism appears to vibrate when moving.
Since 1817, 7 cholera pandemics have occurred. The pandemics originated from cholera’s endemic reservoir in the Indian subcontinent. The first 6 occurred from 1817-1923 and were probably the result of V cholerae O1 of the classic biotype. Of these 6 pandemics, 5 affected Europe and 4 reached the United States, causing more than 150,000 deaths in 1832 and 50,000 deaths in 1866.
The seventh pandemic of cholera, and the first in the 20th century, began in 1961; by 1991, it had affected 5 continents. The pandemic continues today. This seventh pandemic was the first recognized to be caused by the El Tor biotype of V cholerae O1. The pandemic originated from the Celebes Islands, Indonesia, and affected more countries and continents than the previous 6 pandemics.
A new strain of cholera, V cholerae serogroup O139 (Bengal) emerged in the fall of 1992 and caused outbreaks in Bangladesh and India in 1993. Disease from this strain has become endemic in at least 11 countries.
Cholera has been rare in industrialized nations for the past century; however, the disease is still common in other parts of the world, including the Indian subcontinent and sub-Saharan Africa. Epidemics occur after war, civil unrest, or natural disasters when water and food supplies become contaminated with V cholerae in areas with crowded living conditions and poor sanitation.
Pathophysiology
V cholerae is a comma-shaped, gram-negative aerobic or facultatively anaerobic bacillus that varies in size from 1-3 µm in length by 0.5-0.8 µm in diameter (see the image below). Its antigenic structure consists of a flagellar H antigen and a somatic O antigen. The differentiation of the latter allows for separation into pathogenic and nonpathogenic strains. Although more than 200 serogroups of V cholerae have been identified, V cholerae O1 and V cholerae O139 are the principal ones associated with epidemic cholera.
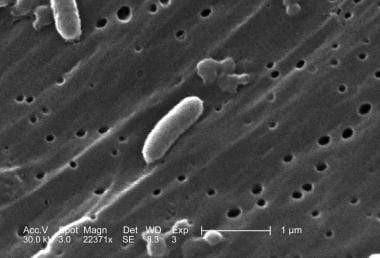 This scanning electron micrograph (SEM) depicts a number of Vibrio cholerae bacteria of the serogroup 01; magnified 22371x. Image courtesy of CDC/Janice Haney Carr.
This scanning electron micrograph (SEM) depicts a number of Vibrio cholerae bacteria of the serogroup 01; magnified 22371x. Image courtesy of CDC/Janice Haney Carr.
Currently, the El Tor biotype of V cholerae O1 is the predominant cholera pathogen. Organisms in both the classical and the El Tor biotypes are subdivided into serotypes according to the structure of the O antigen, as follows:
-
Serotype Inaba - O antigens A and C
-
Serotype Ogawa - O antigens A and B
-
Serotype Hikojima - O antigens A, B, and C
The clinical and epidemiologic features of disease caused by V cholerae O139 are indistinguishable from those of disease caused by O1 strains. Both serogroups cause clinical disease by producing an enterotoxin that promotes the secretion of fluid and electrolytes into the lumen of the small intestine.
To reach the small intestine, however, the organism has to negotiate the normal defense mechanisms of the GI tract. Because the organism is not acid-resistant, it depends on its large inoculum size to withstand gastric acidity.
The infectious dose of V cholerae required to cause clinical disease varies by the mode of administration. If V cholerae is ingested with water, the infectious dose is 103 -106 organisms. When ingested with food, fewer organisms (102 -104) are required to produce disease.
The use of antacids, histamine receptor blockers, and proton pump inhibitors increases the risk of cholera infection and predisposes patients to more severe disease as a result of reduced gastric acidity. The same applies to patients with chronic gastritis secondary to Helicobacter pylori infection or those who have undergone a gastrectomy.
V cholerae O1 and V cholerae O139 cause clinical disease by producing an enterotoxin that promotes the secretion of fluid and electrolytes into the lumen of the small intestine. The enterotoxin is a protein molecule composed of 5 B subunits and 2 A subunits. The B subunits are responsible for binding to a ganglioside (monosialosyl ganglioside, GM1) receptor located on the surface of the cells that line the intestinal mucosa.
The A1 subunit of cholera toxin activates adenylate cyclase to cause a net increase in cyclic adenosine monophosphate (cAMP). The increased cAMP then carries on the downstream effects. cAMP blocks the absorption of sodium and chloride by the microvilli and promotes the secretion of chloride and water by the crypt cells. [3, 4] The result is watery diarrhea with electrolyte concentrations isotonic to those of plasma.
Fluid loss originates in the duodenum and upper jejunum; the ileum is less affected. The colon is usually in a state of absorption because it is relatively insensitive to the toxin. However, the large volume of fluid produced in the upper intestine overwhelms the absorptive capacity of the lower bowel, resulting in severe diarrhea. Unless the lost fluid and electrolytes are replaced adequately, the infected person may develop shock from profound dehydration and acidosis from loss of bicarbonate.
The enterotoxin acts locally and does not invade the intestinal wall. As a result, few neutrophils are found in the stool.
The O139 Bengal strain of V cholerae has a very similar pathogenic mechanism except that it produces a novel O139 lipopolysaccharide (LPS) and an immunologically related O-antigen capsule. These 2 features enhance its virulence and increase its resistance to human serum in vitro and occasional development of O139 bacteremia.
Etiology
Cholera can be an endemic, epidemic, or a pandemic disease. Initiation and maintenance of epidemic and pandemic disease by V cholerae result from human infection and poor sanitation with assistance from human migration and seasonal warming of coastal waters.
Owing to the relatively large infectious dose, transmission occurs almost exclusively via contaminated water or food. V cholerae O1 has been shown to survive in crabs boiled for 8 minutes, but not in crabs boiled for 10 minutes. Transmission via direct person-to-person contact is rare.
Certain environmental and host factors appear to play a role in the spread of V cholerae.
Environmental factors
V cholerae is a saltwater organism, and its primary habitat is the marine ecosystem where it lives in association with plankton.
Cholera has 2 main reservoirs, humans and water. V cholerae is rarely isolated from animals, and animals do not play a role in transmission of disease.
Primary infection in humans is incidentally acquired. Risk of primary infection is facilitated by seasonal increases in the number of organisms, possibly associated with changes in water temperature and algal blooms.
Secondary transmission occurs through fecal-oral spread of the organism through person-to-person contact or through contaminated water and food. Such secondary spread commonly occurs in households but can also occur in clinics or hospitals where patients with cholera are treated.
Infection rates predictably are highest in communities in which water is not potable and personal and community hygiene standards are low.
Host factors
Malnutrition increases susceptibility to cholera. Because gastric acid can quickly render an inoculum of V cholerae noninfectious before it reaches the site of colonization in the small bowel, hydrochlorhydria or achlorhydria of any cause (including Helicobacter pylori infection, gastric surgery, vagotomy, use of H2 blockers for ulcer disease) increases susceptibility.
The incidence of cholera appears to be twice as high in people with type O blood. The reason for this increased susceptibility is unknown.
Infection rates of household contacts of cholera patients range from 20-50%. Rates are lower in areas where infection is endemic and individuals, especially adults, may have preexisting vibriocidal antibodies from previous encounters with the organism. For the same reason, adults are symptomatic less frequently than children, and second infections rarely occur or are mild.
An attack of the classic biotype of V cholerae usually results in the generation of antibodies that protect against recurrent infection by either biotype. Those who have had El Tor cholera are not protected against further attacks. Attacks of V cholerae 01 do not lead to immunity against V cholerae 0139.
Asymptomatic carriers may have a role in transfer of disease in areas where the disease is not endemic. Although carriage usually is short-lived, a few individuals may excrete the organisms for a prolonged period.
Epidemiology
United States statistics
In the United States, cholera has virtually been eliminated because of improved hygiene and sanitation systems. Individuals living in the United States most often acquire cholera through travel to cholera-endemic areas or through consumption of undercooked seafood from the Gulf Coast or foreign waters. Between January 1, 1995, and December 31, 2000, 61 cases of cholera were reported in 18 states and 2 US territories. Thirty-seven were travel-associated cases; the other 24 cases were acquired in the United States. [5]
A unique strain of V cholerae O1 (biotype El Tor, serotype Inaba), which is related closely to, but distinguishable from, the strain of the seventh pandemic was recognized in Louisiana and along the Gulf of Mexico in 1973. Since then, this strain has become indigenous to the Gulf coast, although its environmental reservoirs and ecology remain unclear. Of note, none of the toxigenic V cholerae strains associated with the US Gulf Coast (01, 0141, and 075) have caused more than sporadic cases and small outbreaks of diarrhea in the United States. [6]
In October 2005, toxigenic V cholerae infection due to the consumption of contaminated and improperly cooked seafood was reported from Louisiana after Hurricanes Katrina and Rita. [7]
The incidence of Vibrio infection in the United States continues to be low, with highest number documented in the age group older than 50 years, which has been around 0.50 cases per 100,000 population from 2003-2008. The frequency of cholera among international travelers returning to the United States has averaged 1 case per 500,000 population, with a range of 0.05-3.7 cases per 100,000 population, depending on the countries visited.
International statistics
The number of patients with cholera worldwide is uncertain because most cases go unreported. Likely contributory factors are as follows:
-
Most cases occur in remote areas of developing countries where definitive diagnosis is not possible
-
Reporting systems often are nonexistent in such areas
-
The stigma of cholera, which has direct adverse effects on commercial trade and tourism, discourages reporting
-
Many countries with endemic cholera do not report at all
In 1990, fewer than 30,000 cases were reported to the WHO. Reported cases increased more than 10-fold with the beginning of the Latin American epidemic in 1991. In 1994, the number of cases (384,403) and countries (94) reporting cholera was the largest ever registered at the WHO. Even Europe experienced a 30-fold increase in cholera from 1993-1994, with reported cases increasing from 73 to 2,339 and deaths increasing from 2 cases to 47.
According to the WHO, the number of cases surged again in 2005. From 2005 to 2008, 178,000-237,000 cases and 4000-6300 deaths were reported annually worldwide. [8] However, the actual global burden is estimated to be 3-5 million cases and 100,000-130,000 deaths per year. The 2008 outbreak in Zimbabwe lasted longer than a year, with more than 98,000 cases and more than 4000 deaths. [9] Outbreaks in Guinea and Yunnan province in China contributed to this increase. [10, 11]
The V cholerae O139 serogroup (also known as Bengal), which emerged from Madras, India in October 1992, has spread throughout Bangladesh and India and into neighboring countries; thus far, 11 countries in Southeast Asia have reported isolation of this serogroup. Some experts regard this as an eighth pandemic.
In mid-October 2010, a cholera epidemic broke out in Haiti, which has been worsened by heavy rains in 2011. As of June 20, 2011, 363,117 cases of cholera and 5,506 deaths have been reported. [12] The epidemic is the first in Haiti in at least a century, and the source may have been a United Nations peacekeeping team from Nepal that came to Haiti after the catastrophic earthquake that hit the Caribbean nation on January 12, 2010. [13, 14]
Analyses performed by US and Haitian laboratories indicate that the strain involved in the outbreak is V cholerae El Tor O1 from the ongoing seventh pandemic predominant in South Asia . This may have consequences beyond Haiti, since this strain is more hardy and virulent, with an increased resistance to antibiotics. [15]
Age-related differences in incidence
In nonendemic areas, the incidence of infection is similar in all age groups, although adults are less likely to become symptomatic than children. The exception is breastfed children, who are protected against severe disease because of less exposure and because of the antibodies to cholera they obtain in breast milk.
Prognosis
Before the development of effective regimens for replacing fluids and electrolyte losses, the mortality in severe cholera was more than 50%. Mortality is higher in pregnant women and children. Mortality rates are lowest where intravenous therapy is available. Average case fatality rates for Europe and the Americas continue to hover around 1%. At the Treatment Center of the International Center for Diarrheal Disease Research, Bangladesh, less than 1% of patients with severe dehydration die.
In Africa, a marked decline in case fatality rates has occurred since 1970; however, Africa continues to have the highest reported case fatality rates (approximately 4% in 1999) compared with the rest of the world. Low case fatality rates have been achieved in South America, presumably because of the availability of adequate treatment facilities and trained personnel.
Patient Education
Education in environmental control is critical for the prevention of cholera. The source of V cholerae in nature is human excrement, and the most common vehicle of infection is water. Environmental control must focus on keeping these elements apart.
In the developed world, much has been done in public health planning and in the engineering of water conservation and sewage disposal. However, in developing countries, contamination of water by human excrement is a daily hazard. Members of these populations experience a constant cycle of infection, excretion, and reinfection. Education about the sterilization of water and hand-washing techniques is critical but difficult.
Contamination via food is also an important consideration. The source of this contamination is impure water used to wash or flush vegetables and fruit. Water contamination occurs via sewage or soil that is used to fertilize crops. In this situation, training food handlers is necessary.
-
Electron microscopic image of Vibrio cholera.
-
Scanning electron microscope image of Vibrio cholerae bacteria, which infect the digestive system.
-
This scanning electron micrograph (SEM) depicts a number of Vibrio cholerae bacteria of the serogroup 01; magnified 22371x. Image courtesy of CDC/Janice Haney Carr.
-
This patient with cholera is drinking oral rehydration solution (ORS) in order to counteract the cholera-induced dehydration. Image courtesy of the CDC.
Tables
What would you like to print?
- Overview
- Presentation
- DDx
- Workup
- Treatment
- Approach Considerations
- Treatment Guidelines
- Cholera Cots
- Rehydration
- Maintenance of Hydration
- Antibiotic Treatment
- Fluid Replacement for Dehydration
- Oral Rehydration During First 4 Hours
- Oral Rehydration for Home Administration
- Oral Replacement Solution for Hydration Maintenance
- Antimicrobial Therapy for Cholera
- WHO Guidelines for Cholera Management
- Diet
- Deterrence/Prevention
- Vaccines
- Show All
- Medication
- Questions & Answers
- Media Gallery
- Tables
- References