Practice Essentials
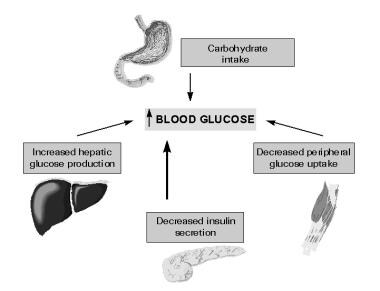
Although type 2 diabetes is widely diagnosed in adults, its frequency has markedly increased in the pediatric age group since the end of the 20th century. Most pediatric patients with type 2 diabetes belong to minority communities. A simplified scheme for the etiology of type 2 diabetes mellitus is shown in the image below.
Signs and symptoms
Distinguishing between type 1 and type 2 diabetes at diagnosis is important. Typical characteristics of type 2 diabetes include the following:
-
Slow and insidious onset
-
Most common in overweight or obese patients from a minority group (Native Americans, Blacks, and Pacific Islanders)
-
Signs of insulin resistance
-
Strong family history of type 2 diabetes: Familial lifestyle risk factors leading to obesity may be present, as may a family history of cardiovascular disease or metabolic syndrome
Physical findings may include the following:
-
Obesity (strongly associated with type 2 in children and adolescents)
-
Acanthosis nigricans
-
Retinopathy
See Clinical Presentation for more detail.
Diagnosis
Testing for type 2 diabetes should be considered when a patient is overweight and has any 2 of the following [1] :
-
Family history of type 2 diabetes in first-degree or second-degree relative
-
Minority race or ethnicity (eg, American Indian, Black, Hispanic, Asian or Pacific Islander)
-
Signs of insulin resistance or conditions associated with insulin resistance (eg, acanthosis nigricans, hypertension dyslipidemia, PCOS)
Recommendations for screening are as follows:
-
Initial screening may begin at age 10 years or at onset of puberty if puberty occurs at a young age
-
Screening should be performed every 2 years
-
A fasting plasma glucose test is the preferred screening study; if clinical suspicion is high but fasting blood glucose is normal (< 100 mg/dL), an oral glucose tolerance test should be considered
Glucose values may be interpreted as follows:
-
A random plasma glucose concentration of 200 mg/dL or greater in association with polyuria, polydipsia, or unexplained weight loss is diagnostic of diabetes [2]
-
In an asymptomatic patient, a fasting plasma glucose value of 126 mg/dL or greater or a 2-hour plasma glucose value of 200 mg/dL or greater during an oral glucose tolerance test is also diagnostic of diabetes [2]
Other laboratory results that usually suggest type 2 diabetes are as follows:
-
Elevated fasting C-peptide level
-
Elevated fasting insulin level
-
Absence of autoimmune markers (glutamic acid decarboxylase [GAD] and islet cell antibodies) [2]
Testing for albuminuria can be done by means of 1 of the following 3 methods:
-
Measurement of the albumin-creatinine ratio in a random spot collection
-
A 24-hour collection for albumin and creatinine determinations, which allows simultaneous measurement of creatinine clearance
-
Timed (eg, 4-hour or overnight) collection
Fasting lipid profiles should be obtained after stable glycemia is achieved and every 2 years thereafter if normal. Optimal values for children with type 2 diabetes are as follows [3] :
-
Triglycerides < 150 mg/dL
-
Low-density lipoprotein (LDL) < 100 mg/dL
-
High-density lipoprotein (HDL) >35 mg/dL
See Workup for more detail.
Management
The goal of therapy is to achieve and maintain euglycemia and near-normal hemoglobin A1c (HbA1c) levels (< 7%). More specifically, glycemic and nonglycemic goals may include the following [4] :
-
Fasting glycemia of less than 126 mg/dL
-
Resolution of polyuria, nocturia, and polydipsia
-
Healthy body weight
-
Maintenance of cardioprotective levels of lipids and blood pressure (LDL level < 100 mg/dL, triglyceride < 150 mg/dL, HDL level >35 mg/dL; blood pressure < 95th percentile for age, sex, and height)
-
Participation of the whole family as a unit
Treatments for pediatric type 2 diabetes include the following:
-
Diabetes education and lifestyle changes (diet, exercise, weight control)
-
Pharmacologic therapy with metformin, insulin, a sulfonylurea, or another hypoglycemic agent
-
Lipid-lowering agents and blood pressure medications to achieve cardioprotection, if necessary
To protect these patients from future cardiovascular disease, treatment should emphasize the following:
-
Improvement of glycemia, dyslipidemia, and hypertension
-
Weight management
-
Prevention of short- and long-term complications
-
Blood glucose monitoring 2-3 times daily (more often when insulin treatment is being adjusted)
-
Evaluation every 3 months at the diabetes clinic (more often, as necessary, when treatment is being adjusted)
HbA1c values should be monitored at each quarterly visit. HbA1c testing has the following advantages over glucose measurement:
-
It captures long-term glucose exposure
-
It has less biologic variability
-
It does not require fasting or timed samples
-
It is currently used to guide management decisions
Additional monitoring should be performed as follows:
-
Microalbuminuria and fasting lipid profile (annually)
-
Dilated eye examination (annually)
-
Blood pressure evaluation and careful neurologic examination (at each clinic visit)
See Treatment and Medication for more detail.
Background
In the past, type 2 diabetes mellitus was very rare in pediatric patients. However, coinciding with the increasing prevalence of obesity among American children, the incidence of type 2 diabetes in children and adolescents has markedly increased, to the extent that it now accounts for as many as one third of all new cases of diabetes diagnosed in adolescents. This trend is particularly pronounced in minority racial and ethnic groups. (See Epidemiology.) [5]
Complications
Although the natural history of type 2 diabetes mellitus in children is not well studied, the experience accumulated over years of treating adults may help to minimize the occurrence of complications in children. (See Prognosis and Clinical.)
Acute complications of type 2 diabetes include hyperglycemia, diabetic ketoacidosis, hyperglycemic-hyperosmolar state, [6] and hypoglycemia. Complications from insulin resistance include hypertension, dyslipidemia, and polycystic ovarian syndrome (PCOS). [7]
As many as 4% of patients with type 2 diabetes initially present in a hyperglycemic-hyperosmolar coma, which can lead to cerebral edema and death if not promptly recognized and treated. [6]
Long-term complications of type 2 diabetes mellitus include the following:
-
Nephropathy
-
Neuropathy
-
Retinopathy
-
Coronary artery disease
A retrospective study found that adults diagnosed with type 2 diabetes before age 45 years have a much higher risk of cardiovascular disease relative to age-matched control subjects. The investigators concluded that early onset type 2 diabetes appears to be a more aggressive disease from a cardiovascular standpoint. (See Prognosis, Clinical, and Treatment.) [8]
Etiology
In individuals without diabetes, approximately 50% of their total daily insulin is secreted during basal periods to suppress lipolysis, proteolysis, and glycogenolysis. In response to a meal, rapid insulin secretion (also called first-phase insulin secretion) ensues. This secretion facilitates the peripheral use of the prandial nutrient load, suppresses hepatic glucose production, and limits postprandial elevations in glucose levels. The second phase of insulin secretion follows and is sustained until normoglycemia is restored. A simplified scheme for the etiology of type 2 diabetes mellitus is shown in the image below.
Type 2 diabetes spans a continuum from impaired glucose tolerance and impaired fasting glucose to frank diabetes that results from progressive deterioration of insulin secretion and action. Although the first phase of insulin response is markedly reduced early in the course of the disease, ongoing disorganized basal insulin secretion associated with deterioration of peripheral insulin action occurs during the progression from normal to impaired glucose tolerance to frank diabetes. [9]
In parallel, as a result of decreased insulin sensitivity in the liver, endogenous glucose output increase adds to the already hyperglycemic milieu, worsening peripheral insulin resistance and beta cell function. Failure of the beta cell to keep up with the peripheral insulin resistance is the basis for the progression from impaired glucose tolerance to overt clinical type 2 diabetes. Longitudinal studies have demonstrated that during the transition between normal glucose tolerance to diabetes, 31% of a person's insulin-mediated glucose disposal capacity, as well as 78% of his or her acute insulin response, is lost.
The UK Prospective Diabetes Study found that beta cell function was 50% of normal at the time of diagnosis of type 2 diabetes in adults. [10] A case study of the progression of diabetes in an adolescent female found an almost 15% decline in beta cell function per year over the 6-year duration of diabetes, with no substantial changes in insulin sensitivity. [11] Further prospective studies in young persons with type 2 diabetes are needed in order to clarify the mechanism of disease in this population.
Risk factors
The major risk factors for type 2 diabetes in young persons are as follows: [12]
-
Obesity and inactivity, which are important contributors to insulin resistance
-
Native American, Black, Hispanic, Asian, or Pacific Islander descent
-
Family history of type 2 diabetes in first- and second-degree relatives
-
Age of 12-16 years, the mean age range of onset of type 2 diabetes in youths - These ages coincide with the relative insulin resistance that occurs during pubertal development
-
Low birth weight and high birth weight [13]
-
Not breastfed during infancy [16]
In a retrospective cohort study of more than 43,000 individuals, study participants who were prescribed antipsychotics were significantly more likely to develop type 2 diabetes within the first year of use compared with matched controls who were not prescribed these medications. The risk increased with higher medication doses and remained elevated for up to 1 year after the medications were discontinued. The association between antipsychotic use and type 2 diabetes remained highly significant when only participants younger than 18 years were assessed.
The study included 28,858 first-time users of antipsychotic medications and 14,429 matched control individuals who had recently initiated use of a psychotropic other than an antipsychotic, all from the Tennessee Medicaid program. All participants were 6 to 24 years of age. Antipsychotics used included risperidone, quetiapine, aripiprazole, and olanzapine. Medications used by the control group included mood stabilizers such as lithium, as well as antidepressants, psychostimulants, α-agonists, and benzodiazepines.
A total of 106 study subjects receiving antipsychotics were diagnosed and treated for type 2 diabetes (mean age, 16.7 years; 63% girls), translating into 18.9 cases per 10,000 person-years. Antipsychotic users had a 3-fold increased risk of developing type 2 diabetes by the end of the study compared with the group of nonusers. This risk was significant within the first year of follow-up. [17, 18]
Epidemiology
Occurrence in the United States
Although type 2 diabetes is widely diagnosed in adults, its frequency has markedly increased in the pediatric age group since the end of the 20th century. Depending on the population studied, type 2 diabetes now represents 8-45% of all new cases of diabetes reported among children and adolescents. [19] Most pediatric patients with type 2 diabetes belong to minority communities.
The SEARCH for Diabetes in Youth Study (a US multicenter, observational study conducting population-based ascertainment of cases of diabetes mellitus in individuals over age 20 y) found that the incidence of type 2 diabetes was highest among American Indians aged 15-19 years (49.4 cases per 100,000 person-years). Second and third highest incidence belonged to Asian-Pacific Islanders and Blacks, aged 15-19 years, with 22.7 cases per 100,000 person-years and 19.4 cases per 100,000 person-years, respectively. [20]
International occurrence
An increased prevalence of type 2 diabetes has also been recognized in countries other than the United States, including Japan, where the incidence of type 2 diabetes in school children after 1981 was found to be strongly related to an increasing prevalence of obesity. [21] Studies among the Indian, British, Chinese, Taiwanese, Libyan, Bangladeshi, Australian, and Maori populations also have shown increasing incidence of youth-onset type 2 diabetes. [22, 23, 24, 25, 26, 27, 28, 29]
Race-, sex-, and age-related demographics
Type 2 diabetes primarily affects minority populations. [20] From 1967-1976 to 1987-1996, the prevalence of type 2 diabetes increased 6-fold in Pima Indian adolescents and appeared for the first time in children and adolescents younger than age 15 years. [30] Similar increases in prevalence were observed among Japanese, Asian-American, and Black children. In several clinics across the United States, pediatric patients with a diagnosis of type 2 diabetes were from minority ethnic groups (Black, Asian, and Hispanic groups).
The prevalence of type 2 diabetes in the pediatric population is higher among girls than boys, just as the prevalence is higher among adult females than it is in adult males. [12]
The mean age range of onset of type 2 diabetes is 12-16 years; this period coincides with puberty, when a physiologic state of insulin resistance develops. In this physiologic state, type 2 diabetes develops only if inadequate beta cell function is associated with other risk factors (eg, obesity). [31]
A white paper by the FAIR Health organization that analyzed private claims from more than 21 billion 0- to 22-year-olds found that claim lines with a diagnosis of type 2 diabetes increased 109% between 2011 and 2015. The study also found that although obesity was diagnosed more frequently in females, type 2 diabetes were more frequently diagnosed in males; however, further study is warranted to analyze this association between prevalence of pediatric type 2 diabetes and gender as other studies have found conflicting results. [32, 33]
According to data from the SEARCH for Diabetes in Youth study, the overall prevalence of type 2 diabetes among American youths aged 10-19 years rose by 35% between 2001 and 2009 (from 0.34 per 1000 to 0.46 per 1000). Study data were obtained from 38 counties in five states, as well as American Indian reservations in Arizona and New Mexico, and included young people from several different racial-ethnic backgrounds.
The greatest increase in the prevalence of type 2 diabetes from 2001 to 2009 was observed in Hispanic youths (from 0.45 per 1000 to 0.79 per 1000), followed by Blacks (from 0.95 per 1000 to 1.06 per 1000), and Whites (from 0.14 per 1000 to 0.17 per 1000). [34] There were no significant changes in prevalence for either American Indians or Asian Pacific Islanders.
Prognosis
After 30 years of postpubertal diabetes, 44.4% of people with type 2 diabetes and 20.2% of people with type 1 diabetes develop diabetic nephropathy. Overall, the incidence of nephropathy has declined among patients with type 1 diabetes since the end of the 20th century; however, it has not for persons with type 2 diabetes.
So far, no population-based follow-up study has been conducted to determine the long-term prognosis of type 2 diabetes among children and adolescents. Mortality rates and standardized mortality ratios in type 2 diabetes are likely higher than those in type 1 diabetes, given that the major cause of death in type 1 diabetes is end-stage renal disease.
Morbidity and mortality/Complications
Overall, morbidity and mortality associated with type 2 diabetes are related to short-term and long-term complications. A longitudinal, population-based study conducted from 1965-2002 in the Arizona Pima Indian population found that youth-onset type 2 diabetes is associated with substantially increased incidence of end-stage renal disease and mortality in middle age. [35]
In a comparative study among Japanese youths with type 1 and type 2 diabetes, the cumulative incidence of nephropathy among patients with type 2 diabetes was higher than it was in those with type 1 diabetes. Nephropathy also appeared earlier in type 2 diabetes than it did in type 1 diabetes. [36]
The SEARCH for Diabetes in Youth Study found that American youth with type 2 diabetes have a higher prevalence of elevated albumin-to-creatinine ratio (ACR) than do young persons with type 1 diabetes. The study also found that high blood pressure, hyperglycemia, and high triglyceride concentrations are associated with elevated ACR, independent of the type of diabetes. [37] Albuminuria is a risk factor for renal failure in pediatric type 2 diabetics. Youth with type 2 diabetes are at a fourfold increased risk of renal failure compared to pediatric patients with type 1 diabetes. [38]
Among the Pima Indians of Arizona, the risk of retinopathy is lower in patients with youth-onset type 2 diabetes than in those with adult-onset diabetes. [39]
The TODAY study was a recent multicenter clinical trial comparing treatment options in a large cohort of youth with recently diagnosed type 2 diabetes. [40] The trial showed that high rates of complications and comorbidities (hypertension, hyperlipidemia, retinopathy, and microalbuminuria) were already present in during the first few months of diagnosis and the rate of progression of these conditions increased progressively throughout the trial period. In fact, the common complications of type 2 diabetes seen in adults are also found in youth with type 2 diabetes but appear to progress on an accelerated timeline. Consequently, preventive measures, aggressive screening and a high index of suspicion are therefore required in order to curb these negative outcomes that could significantly burden this population during their third and fourth decades of life. [41, 42]
Patient Education
Education is an essential component of the treatment plan in type 2 diabetes; it is a continuing process involving the child, family, and all members of the diabetes team. The following strategies may be used:
-
Appropriate teaching of survival skills at diagnosis
-
Explanation and discussion about the possible causes of type 2 diabetes
-
Discussion about the need for blood glucose monitoring and the importance of compliance with the drug regimen
Practical skills training includes the following:
-
Insulin injections (if insulin is part of the treatment plan)
-
Blood and/or urine testing for ketone bodies
-
Hypoglycemia recognition and treatment
-
Emergency telephone contact procedure
-
Psychosocial adjustment to the diagnosis
-
Importance of regular follow-up
-
Basic dietary advice
Diabetes education is an ongoing process and should address the following issues:
-
Formal education during clinic visits or during diabetes classes
-
Educational holidays and camps
-
Support groups
-
Complications - Use times of crisis or acute complications as opportunities to reinforce the importance of some aspects of self ̶ diabetes management that may have been neglected
Educate the patient about the potential side effects of oral hypoglycemic agents (eg, the presence of ketonuria or of any condition predisposing to the accumulation of lactate in patients on metformin).
With regard to the patient’s sexual health, provide advice about contraception, genital hygiene, sexually transmitted diseases, and fungal infections. In pregnant patients with type 2 diabetes, emphasize the importance of good glycemic control before and during pregnancy and discuss the effect of maternal diabetes on the fetus.
-
Simplified scheme for the pathophysiology of type 2 diabetes mellitus.