Practice Essentials
Congenital factor XIII (FXIII) deficiency, originally recognized by Duckert in 1960, is a rare autosomal recessive disease usually associated with a severe bleeding diathesis. Although acquired factor XIII deficiency has been described in association with chronic conditions such as hepatic failure, inflammatory bowel disease, and myeloid leukemia, the only significant cause for bleeding in children is an inherited deficiency. [1]
Factor XIII is a plasma transglutaminase that catalyzes the final step in the coagulation cascade, cross-linking the loose fibrin polymer into a highly organized structure. In addition, factor XIII covalently binds fibronectin, a2-plasmin inhibitor, and collagen to the fibrin plug; this enhances adherence to the wound site, resistance to fibrinolysis, and wound healing by providing a scaffold for fibroblast migration and proliferation. Fibrin-fibronectin cross-linking is necessary to support the formation of the cytotrophoblastic shell at the site of placental implantation, which accounts for the role of factor XIII in the maintenance of pregnancy. [2]
Signs of factor XIII deficiency
These include the following:
-
Persistent bleeding from the stump of the umbilical cord in newborns [3]
-
Soft tissue and subcutaneous bleeding
-
Neurologic findings commensurate with CNS hemorrhage
-
Bleeding in the oral cavity
-
Hemarthroses or periarticular bleeding
-
Poor wound healing
Workup in factor XIII deficiency
Assessment of clot stability is the most common screening test for factor XIII deficiency, even though sensitivity and specificity are low.
The two methods used to measure the enzymatic activity of factor XIII include measurement of synthetic amine incorporation into a fibrin clot, and measurement of ammonium ion release during the transglutaminase reaction. [4]
Factor XIIIa and factor XIIIb antigen levels can be quantified by means of enzyme-linked immunosorbent assay (ELISA).
Appropriate imaging studies are required in the evaluation of suspected bleeding.
Management of factor XIII deficiency
Fresh frozen plasma (FFP), cryoprecipitate, and factor XIII (FXIII) concentrates have been used for replacement of factor XIII and the treatment of acute bleeding. For years, the treatment of choice has been plasma-derived factor XIII concentrate that is pasteurized to provide virologic safety and is less likely than plasma to cause systemic reactions.
Recombinant factor XIII-A2 (Tretten) was approved by the US Food and Drug Administration (FDA) in December 2013 and presents an alternative in the treatment of congenital factor XIII A-subunit deficiency.
Pathophysiology
The factor XIII zymogen circulates in plasma as a tetramer composed of 2 catalytic A subunits and 2 carrier B subunits (A2 B2). The A subunits are synthesized in megakaryocytes and monocyte precursors in the bone marrow and placenta; A2 dimers are present in circulating platelets and monocytes. The B subunits are synthesized in hepatocytes. The A2 and B2 dimers assemble in the plasma to form a heterotetramer, which has a long plasma half-life of 7-12 days. Activation of the zymogen to factor XIIIa depends on limited thrombin cleavage of the A subunits followed by calcium-dependent dissociation of the B subunits, exposing the A subunit active site (as shown in the image below).
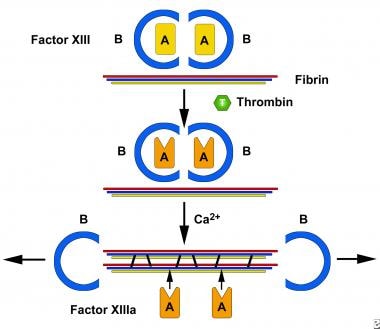 Activation of factor XIII (FXIII) by thrombin and calcium is a 2-step process. Thrombin cleaves an arginine-lysine bond in the A subunit and calcium causes dissociation of the B subunit, exposing the active site on the A subunit (XIIIa).
Activation of factor XIII (FXIII) by thrombin and calcium is a 2-step process. Thrombin cleaves an arginine-lysine bond in the A subunit and calcium causes dissociation of the B subunit, exposing the active site on the A subunit (XIIIa).
Factor XIIIa catalyzes the formation of covalent bonds between glutamine and lysine residues on the fibrin a and g chains, enhancing the mechanical strength of the fibrinpolymer.
Investigators have demonstrated other substrates for factor XIIIa, including proteins such as osteopontin, factor V, thrombospondin, vinculin, and endothelial cell receptors αvβ3 integrin and VEGFR-2. These observations have suggested physiologic and pathologic roles for factor XIII in angiogenesis, atherosclerosis, and inflammation. By cross-linking bacterial surface proteins to fibrinogen, factor XIIIa causes bacteria to be immobilized and killed. Wound healing is promoted by factor XIIIa via cross-linking of the provisional matrix, a process that influences the extracellular matrix–leukocyte interaction. [5]
Inherited factor XIII deficiency is usually due to mutations in the gene encoding the catalytic A subunit, located on chromosome 6. More than 40 different mutations have been identified, half of which are missense mutations. [6] In patients homozygous for this defect, the A subunit is absent in plasma, platelets, and monocytes, resulting in a severe bleeding diathesis; the concentration of B subunits is relatively normal. The impaired cross-linking of extracellular matrix proteins at sites of wound healing or placental implantation can lead to abnormalities in these processes, resulting in abnormal or delayed healing and spontaneous abortion.
Mutations have also been found in the gene encoding the B subunit, located on chromosome 1; however, this has been reported in only 5 families to date. With the absence of the carrier B subunits, the plasma half-life of the A subunits is shorter (ie, 3 d), resulting in decreased plasma levels of both A and B. However, because of the presence of A subunits in platelets and monocytes, the phenotype is less severe.
Epidemiology
Frequency
International
The prevalence of factor XIII deficiency is about 1 case per 2 million in the general population. Worldwide, the prevalence is highest in the Sistan and Baluchistan province of Iran. [7] In addition to Iran, population-specific mutations due to founder effects have been reported in Pakistan, India, Tunisia, and Finland.
A study by Gebhart et al of Austrian patients with mild to moderate bleeding disorders found that out of 418 individuals with these conditions, just one (0.2%) had factor XIII deficiency. Factor VIII, IX, and XI deficiencies occurred in 11 (2.6%), 3 (0.7%), and 3 (0.7%) patients, respectively. [8]
Mortality/Morbidity
The mortality and morbidity are primarily related to bleeding; intracranial hemorrhage can be life threatening. The spontaneous abortion rate in women with severe factor XIII deficiency approaches 80%.
Sex
This is an autosomal recessive disease; the male-to-female ratio is 1:1.
Age
Because the clinical bleeding is severe in most patients with hereditary factor XIII deficiency, the diagnosis is made at an early age, often during infancy.
-
Activation of factor XIII (FXIII) by thrombin and calcium is a 2-step process. Thrombin cleaves an arginine-lysine bond in the A subunit and calcium causes dissociation of the B subunit, exposing the active site on the A subunit (XIIIa).









