Overview
Pectus excavatum (PE), also known as funnel chest or trichterbrust, is by far the most common chest wall deformity, occurring in 1 of every 400 white male births. [1] Pectus carinatum (PC), the next most common chest wall deformity, is five times less common than pectus excavatum. [2] See the images below.
Pectus Excavatum
For more than half a century, the traditional method of repair for pectus excavatum (PE) was the modified Ravitch repair. In 1998, a minimally invasive method of repair, the Nuss procedure, was introduced. This article reviews the available literature regarding the efficacy and safety of both approaches.
Embryology and etiology
Several theories explain the cause of pectus excavatum; however, the etiology remains obscure. Some authors believe that pectus excavatum may be due to an overgrowth of costal cartilage, which displaces the sternum posteriorly. Abnormalities of the diaphragm, rickets, or elevated intrauterine pressure are also theorized to cause posterior displacement of the sternum. [3, 4, 5] Reports of pectus excavatum occurring with diaphragmatic agenesis and congenital diaphragmatic hernia may support this theory. [3, 6, 4] Scoliosis is reported in 21% of patients with pectus excavatum, and 11% of patients with pectus excavatum have a family history of scoliosis. [7]
The coexistence of pectus excavatum with other musculoskeletal disorders, such as Marfan syndrome, suggests that an abnormality of connective tissue may be involved. In addition, 40% of patients with pectus excavatum have a familial history, suggesting a possible genetic predisposition. [8]
Clinical presentation and evaluation
The appearance of pectus excavatum can range from a mild, shallow defect to one in which the sternum almost touches the vertebral bodies. The appearance of the defect is the result of two factors: (1) the degree of posterior angulation of the sternum and (2) the posterior angulation of the costal cartilages as they meet the sternum. If additional sternal or cartilaginous asymmetry is present, these defects become more challenging for the surgeon to manage. [9]
Pectus excavatum is generally present at birth or arises shortly thereafter. It is often progressive, and the depth increases as the child grows. [10] Pectus excavatum is more common in males than in females, with a male-to-female ratio of 6:1. Pectus excavatum can be associated with other congenital abnormalities, including abnormalities of the diaphragm. In 2% of patients, pectus excavatum is associated with congenital cardiac anomalies. In patients with the characteristic body habitus, the diagnosis of Marfan syndrome should be considered. In some instances, repair of a pectus excavatum may be performed concomitantly with other procedures; however, the authors have found that pectus repair in the setting of open cardiac surgery is rare. In patients who require extracardiac conduits, pectus excavatum repair may be considered to avoid external compression of the conduit.
Several methods have been developed to quantitate the severity of pectus excavatum, which usually involve measuring the distance from the sternum to the spine. Perhaps the most commonly used method is that of Haller et al; [11] this method uses a ratio of the transverse distance to the anteroposterior distance derived from chest CT scans. In the Haller system, a score of 3.25 or higher is associated with a severe defect that requires surgery.
Pectus excavatum generally has no discernible physiologic effect on infants or children. Some children have pain in the area of the sternum or costal cartilage, especially after vigorous exercise. Other children have palpitations that might be related to mitral valve prolapse that commonly occurs with pectus excavatum. A flow murmur may also be detectable in some patients. This flow murmur is related to the close proximity of the sternum to the pulmonary artery resulting in transmission of a systolic ejection murmur. [12]
Asthma is sometimes noted in children with both pectus excavatum and pectus carinatum (PC). Pectus excavatum does not seem to affect the clinical course of asthma in patients. A recent meta-analysis of studies examining the effect of pectus excavatum repair on pulmonary function revealed no statistically significant improvement in pulmonary function. No difference in pulmonary function was observed between surgical approaches. [13] The impact of pectus excavatum on the cardiopulmonary system continues to be debated.
Malek et al studied the impact of pectus excavatum on the cardiovascular system. Their meta-analysis revealed a significant improvement in cardiovascular function following surgical repair of pectus excavatum. Specifically, a 6-13% improvement in the cardiac output, stroke volume, and oxygen pulse was observed following pectus excavatum repair. Malek et al suggested that poor results reported in past studies could have been related to deconditioning following surgical repair or submaximal exercise testing. Patients with pectus excavatum who underwent incremental exercise testing prior to the repair reached their ventilatory threshold at 39% of VO2 max predicted, which improved postoperatively to 50% of VO2 max predicted. [14]
Indications for surgery
Although discerning a specific physiologic consequence of pectus excavatum is difficult, several surgical indications are noted. The sunken appearance of the chest wall has been associated with poor self-image in children, especially as they approach adolescence; the major indication is currently psychosocial. [15] Improvement of the appearance of the chest wall after the repair improves socialization. [15] In competitive athletes, in whom a slight decrease in exercise tolerance may impair their performance, surgeons may also choose to repair the pectus excavatum.
When performed in the setting of cardiac surgery, a single-stage repair of pectus excavatum has been reported using a sternal flap based on the internal thoracic arteries, followed by repair of the intracardiac defect and a traditional Ravitch repair. [16] Alternative approaches have included the Ravitch repair followed by a left parasternal approach to the cardiac defect. [17] A left thoracotomy approach has also been described for patients with unrepaired pectus excavatum and mitral or aortic valvular disease. [18] In the absence of a specific indication to make more room in the chest for a cardiac repair, the authors elect to repair a pectus excavatum subsequent to the intracardiac repair.
Other indications include a failed previous repair.
Surgical Repair of Pectus Excavatum
Surgical repair
Meyer performed the first surgical repair of pectus excavatum in 1911, [19] followed by Sauerbruch in 1913. [20] In 1949, Ravitch reported a technique that formed the basis of modern pectus excavatum surgery. Through a midline incision over the defect, excision of all deformed cartilage from the perichondrium, division of the xiphoid from the sternum, division of the intercostals bundles from the sternum, and transverse sternal osteotomy were performed. The sternum was displaced anteriorly and held into position by using wires. [21]
In 1958, Welch modified the procedure by preserving the perichondrial sheaths of the costal cartilages to allow for regrowth. He preserved the upper cartilaginous intercostal bundles and fixed the sternum anteriorly with silk suture. [22] Other surgeons further modified this approach by adding a metal strut to ensure stability of the sternum. [23, 24]
Haller et al (1970) described a technique of tripod fixation of the sternum. [11] This method uses a posterior sternal osteotomy, subperichondrial resection of the lower deformed cartilage, and oblique division of normal upper second or third cartilage. The obliquely divided cartilages are positioned to override themselves and are secured in a position anterior to the sternum.
A technique developed in France and primarily used in Japan divides the sternum from the cartilage. [25] The sternum is then flipped 180° and reattached to the cartilage as a free graft. This technique is not commonly used and has a higher complication rate compared with more conventional methods. [26]
Silicone implants have been introduced into the subcutaneous space above the sternum. [27] This results in cosmetic improvement but not physiologic improvement in the pectus excavatum.
Fonkalsrud et al have reported a technique of minimal cartilage resection and suture reattachment of the divided costal cartilages to the sternum and ribs. [28] This decreases the formation of postoperative osteoid in the destroyed perichondrial sheaths, preventing the development of asphyxiating thoracic dystrophy (Jeune syndrome). The surgeons further implanted cartilage chips in the space between the ends of the cartilage in order to facilitate early cartilaginous growth.
Other innovative strategies include the use of substernal mesh bands for asymmetric pectus excavatum defects, [29] transsternal and parasternal struts in the Willital-Hegemann method, [30] and extensive retrosternal mobilization with tension measurements in the Erlangen technique. [31]
Davis and Weinstrein presented a series of 69 consecutive patients with the pectus deformity who underwent a modified Ravitch repair. [32] Their modification included developing a generous subcutaneous flap over the muscle fascia, thus greatly limiting the skin incision for both pectus excavatum and pectus carinatum (PC) correction procedures. A median of four sets of costal cartilage were removed in both subgroups. After that, a posterior sternal table osteotomy was performed, with placement of a triangular wedge of rib bone harvested from a lateral rib for stabilization. Asymmetry was dealt with by adjusting the angle of the posterior osteotomy. Good-to-excellent results were reported in 81.3% of the patients. No deaths or significant intraoperative morbidities occurred. Seromas developed after discharge in 5 patients (7.2%), requiring aspiration.
The authors concluded that the modified Ravitch procedure remains a safe and effective approach to the repair of the pectus deformity in all of its presentations. Because the technique rarely uses a metal strut, a second procedure for strut removal is not necessary. [32]
Minimally invasive repair of pectus excavatum (ie, the Nuss procedure) involves inserting a custom-bent curved metal bar underneath the sternum through lateral chest incisions. The bar is then turned, placing the convexity of the bar upward correcting the pectus depression. The bar is then secured to the lateral aspect of the chest wall, ribs, or both and left in place for 2-4 years, after which it is removed in a second procedure. [33] See the images below.
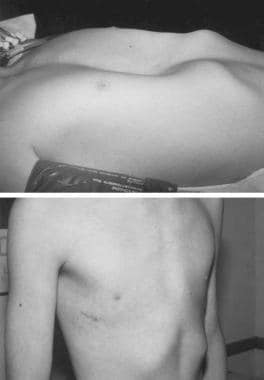 Preoperative (top) and postoperative (bottom) photograph of a 12-year-old boy prior to minimally invasive repair of pectus excavatum. Note the small lateral chest wall incision and the excellent appearance of the anterior chest with 100% correction of the pectus deformity.
Preoperative (top) and postoperative (bottom) photograph of a 12-year-old boy prior to minimally invasive repair of pectus excavatum. Note the small lateral chest wall incision and the excellent appearance of the anterior chest with 100% correction of the pectus deformity.
Several modifications to the Nuss procedure have been proposed. Implementation of a lateral stabilizing bar was perhaps the first major modification and was a response to a substantial number of bar displacements. Hebra et al (2001) proposed the use of a 3-point fixation method in conjunction with the stabilizing bar. [34] Bar dislodgement, which is more common in adult patients, can also be prevented by submuscular placement. [35]
A study by Park et al suggested that stabilization of the pectus bar using a combination of a claw fixator and hinge plate may be more effective than use of a conventional stabilizer. In the study, which involved the use of a pectus bar in 1816 pectus excavatum repairs, the investigators found that early bar dislocation rates in patients stabilized with the claw fixator/hinge plate combination was 0%, compared with 3.33% in those in whom a conventional stabilizer was used, 0.56% in patients who were stabilized with multipoint pericostal suture fixation, and 0.57% for those who were stabilized with the claw fixator alone. [36]
Another modification is the use of thoracoscopy to monitor safe passage of the clamp across the mediastinum. A survey of surgeons performing the Nuss procedure revealed that 61% now use thoracoscopy on a routine basis. [37] Bilateral thoracoscopy has been reported to have the lowest rate of operative complications. [38, 39]
Nuss et al have recommended increasing the bar removal time to 3-4 years after the first procedure to decrease the incidence of pectus excavatum recurrence. [33] Whether this prolongation will increase the number of positive outcomes has not been determined. Because of the various modifications, comparing results from one series with results from another can be difficult.
The use of thoracic epidural analgesia has also improved postoperative pain management in patients undergoing pectus excavatum repair of any type. [40] Meta-analysis has confirmed that postoperative epidural pain control can significantly decrease the incidence of pulmonary morbidity. [41] A predicted risk of 0.07% of permanent neurological complications is estimated in adults with thoracic epidural catheterization. [42]
Outcomes of surgical repair
Historically, reports of outcomes and patient satisfaction following the Ravitch repair and its variants have been excellent. In several large series, satisfactory results were reported in more than 90% of patients with a metal strut in the repair. [43]
Complications of open repair of pectus excavatum are infrequent (8%). [28] The most common complication is a pneumothorax. It tends to be small and can be observed. Large pneumothoraces usually require only aspiration of air. Wound infection, pericardial effusion, and pericarditis can also occur but are rare. In a series of 320 patients with pectus deformities corrected by modified Ravitch repair, mild recurrent pectus excavatum deformity occurred in only 3 patients. [44] These patients only required minor cartilage resection at the time of bar removal. No perioperative deaths were reported in this series.
The most serious complication of the classic Ravitch repair was impaired development of the thoracic cavity. Haller et al (1995) reported a series of 12 patients who underwent pectus excavatum repair and developed thoracic dystrophy. [45] In each instance, repair was performed in children younger than 4 years, and more than 5 ribs were resected. These patients presented with severe exercise intolerance and a clinically significant reduction in pulmonary function.
The early age at which the operation is performed is not the suspected cause of the thoracic dystrophy, rather the inappropriate surgical technique is now the suspected cause. This includes radical chondrocostal resection, extirpation of growth centers, and suturing together of the perichondrial strips retrosternally, causing cartilaginous growth behind the sternum. [46] Thus, most surgeons who perform the Ravitch procedure have modified the approach to a smaller incision, limitation of ribs resected, and to an older age population (adolescence or early adult).
A prospective, nonrandomized multi-center observational study of 327 patients was conducted to compare the outcomes of the standard modified Ravitch procedure with the outcomes of the Nuss procedure. [47] Outcomes were similar, and rates of complications were not statistically significant; however, higher complications with the Nuss procedure have been noted in the literature, either as a result of the technique or the learning curve normally expected with a newer thoracoscopic technique. If the latter is the case, these complications should diminish over time. Currently, an almost 40-year follow-up is available for the Ravitch procedure, confirming excellent results. [28, 48]
Complications reported with the Nuss procedure have included the following: [34, 1] cardiac perforation, delayed tamponade as a result of the bar eroding into the aorta, [49] and right ventricular injury, likely as a result of adhesions. [50] One case of bilateral empyema with pericarditis has also occurred. Three cases of thoracic outlet syndrome have been reported. At the time of the report, the bar had to be removed in one patient because of severe symptoms related to the brachial plexus and arm cyanosis, which was relieved with arm elevation. Haller et al (1995) found this complication in open surgery, primarily in younger patients. [51]
The Nuss procedure has been used to treat pectus excavatum in adult patients. [35] A higher complication rate (19-58%) has been reported in adults. Also, higher forces needed to correct the deformity can result in bar displacement in as many as 50% of patients, as well as early metal fatigue and fracture of the bar. As many as 32% of adults may require placement of an additional pectus bar. [52]
In a retrospective analysis, Pawlak et al compared the results of the Nuss procedure in the surgical treatment of pectus excavatum in 680 patients, with a mean follow-up of 33 months. Patients were divided into three age groups: group A (7-14 years of age), group B (15 to 20 years of age), and group C (older than 20 years of age). Good and very good corrective effects were obtained in 97.7% of the total patient population; the rate of early non-life-threatening complications increased with age (group A, 24.3%; group B, 37.8%; group C, 38.8%; P = 0.0063). [53]
Although failed or recurrent pectus excavatum repairs are technically more challenging, reoperative correction by the Nuss procedure is also possible. [54]
Pectus Carinatum and Other Rare Deformities of the Anterior Chest Wall
Introduction
Pigeon chest or pectus carinatum (PC) is the second most common congenital chest wall deformity. Pectus carinatum constitutes approximately 7% of all anterior chest wall deformities. It is more common in boys than girls (ratio, 4:1). It is typically apparent at birth and tends to worsen as the child grows. Pectus carinatum is typically thought of as a protrusion of the chest wall (the opposite of pectus excavatum [PE]) but actually represents a spectrum of deformities that involve the costochondral cartilage and sternum. Costochondral cartilage involvement may be unilateral or bilateral. In addition, the sternal protrusion may be superior or inferior. The defect may be asymmetrical, causing a rotation of the sternum with depression on one side and protrusion on the other.
Etiology
The pathogenesis of pectus carinatum, much like that of pectus excavatum, is obscure. Pectus carinatum has been postulated to represent an overgrowth of ribs or costochondral cartilage. A genetic predilection may be present because 26% of patients have a family history of chest wall deformity. Furthermore, 15% of patients also have scoliosis, congenital heart defects, Marfan syndrome or other connective tissue disorders.
Presentation
Pectus carinatum can be divided into three distinct types of deformities. Type 1 is termed chondrogladiolar protuberance (keel chest deformity) and is characterized by a symmetric protrusion of the body of the sternum (gladiolus) and costal cartilages. A lateral depression of the ribs results, which is known as runnels or Harrison grooves. Chondrogladiolar protuberance, which comprises 90% of pectus carinatum deformities, has been described as looking like the result of a giant hand crushing the chest from each side.
Symptoms from pectus carinatum are more common in adolescents and range from severe shortness of breath on minimal exertion, reduced endurance and exercise-induced asthma. Chest wall excursions are limited due to the fixed anteroposterior diameter of the thorax, resulting in increased residual volume, tachypnea, and compensatory diaphragmatic excursions. Surgical repair can result in an improvement of 9% in vital capacity. [2]
Treatment
The treatment of pectus carinatum is surgical, although successful applications of orthotic bracing has been reported. [55, 56] However, wearing a chest brace for 16-23 hours a day does raise patient compliance issues and is least successful in the more severe cases. [57] Patients who failed orthotic intervention had a higher Haller index (2.85 vs 2.05), a greater angle of sternal rotation (27.3º vs 14.8º), and an increased asymmetry index (1.23 vs 1.06). [58]
Minimally invasive surgical correction and noninvasive chest wall bracing are options for treatment of pectus carinatum. [59] Ventral chest wall dissection is performed by insufflation of carbon dioxide after insertion of two subpectoral trocars. Endoscopic-assisted rib resection is then performed, followed by axial reanastomosis of the divided cartilages. Transsternal struts are then placed using endoscopic guidance and sternotomies are performed using a combination of endoscopy and a mini–open incision (2.9-4.7 cm). [60] Operative times average 180 minutes, which compares favorably with open techniques.
In one study, de Beer et al tested the use of a dynamic compression brace for pectus carinatum in 286 patients who had a pressure of initial correction (PIC) of 10.0 pounds per square inch or less. The investigators reported that 78 patients completed brace treatment, 181 patients were still wearing the brace, and 27 patients abandoned treatment. Adverse events were minor; they included skin lesions (1%) and vasovagal reactions at the beginning of therapy (1%). [61]
Ravitch reported the first surgical repair of a carinatum defect in 1952. He described a method in which resection of abnormal cartilage was combined with double osteotomy of the sternum to elevate the defect. Other surgical attempts at repair were described in which part of the sternum was resected, up to and including a complete subperichondrial resection.
The modern method of repair is based on the procedure described by Ravitch and Vos in 1973. They performed subperichondrial resection of the abnormal cartilage and preserved the sternum. Transverse osteotomy of the sternum was made and, when combined with fracture of the posterior cortex of the sternum, allowed posterior displacement of the sternum. In 1987, Shamberger and Welch (1987) published their experience with this repair in 152 patients. [62] Satisfactory results were achieved in all but 3 patients (98%). Fonkalsrud (2004) reported a less extensive technique with minimal cartilage resection and suture reattachment of the cartilage segments to the ribs and sternum, combined with 2-3 transverse sternal osteotomies. [2] They used a temporary support bar anterior to the sternum and ribs for 6 months.
Complications and outcomes
In general complication rates for the open resection technique are low. Excellent results were noted in 97% of patients at a follow-up of 8 years, [2] with seroma occurring in 2 of 154 patients and one pneumothorax. Long-term complications of asphyxiating thoracic dystrophy were not seen in this group because preservation of the costal cartilages maintained thoracic flexibility.
In the minimally invasive repair of pectus carinatum group, 33 of 37 patients reported an excellent outcome, and 4 patients reported a good outcome after a follow-up of 29 months. These results were maintained even after strut removal. [60]
Poland Syndrome
Poland syndrome, named after Albert Poland who first described this entity while attending medical school, refers to a spectrum of disorders that involve hypoplasia of the chest wall. This may involve (alone or in combination) the pectoralis major, pectoralis minor, serratus anterior, ribs, and soft tissue. Deformities of the arm and hand may also be observed.
The incidence of Poland syndrome is approximately 1 case per 32,000 live births, and its occurrence is almost always sporadic or nonfamilial. It is 3 times more common in boys than in girls and involves the right side in 75% of patients. Multiple theories regarding the etiology have been proposed, which include abnormal migration of embryonic tissue, hypoplasia of the subclavian artery or in utero injury from attempted abortion. However, none of these theories are widely accepted.
Rare associations of Poland syndrome with other diseases have been noted. Leukemia has been observed in some patients with Poland syndrome. An association with Möbius syndrome (unilateral or bilateral facial palsy and abducens oculi palsy) has been reported.
The presentation of patients with Poland syndrome varies according to the type of defect, with most presenting with cosmetic complaints. In patients with notable bony defects, lung herniation may be noted early in childhood, especially with coughing or crying. Some patients may have a functional flail chest and present with respiratory compromise. The lung itself is otherwise normal in these patients. In patients with significant muscular and soft tissue involvement, Poland syndrome may become evident secondary to exercise intolerance.
Treatment of patients with Poland syndrome depends on the type of defect. Ravitch first described the reconstruction of the chest wall in patients with rib aplasia with autologous rib graft in 1966, and this remains the standard repair. [63] This repair involves exposure of the chest wall through a transverse incision and subperichondrial rib resection on both sides, with care taken not to violate the pleural cavity. The third, fourth, and fifth costal cartilages are removed in their entirety, whereas the sixth and seventh costal cartilages are resected to the point where they join the costal arch. A transverse osteotomy through the sternum is performed which allows correction of the sternal rotation. Rib grafts taken from the contralateral fifth or sixth rib are used to reconstruct the chest in patients with rib aplasia. Recent modification has included changing to a vertical limited skin incision. [64]
Breast reconstruction may be required in female patients. Techniques include implants and latissimus dorsi flaps, often in conjunction. Reconstruction is performed after puberty to optimize the match between the normal and reconstructed breast.
Endoscopically assisted reconstruction of Poland syndrome has been reported. Initially tissue expanders are inserted followed by a second-stage latissimus dorsi harvest and reconstruction using only endoscopic techniques. [65]
Outcomes of surgical correction of Poland syndrome depend on the type of defect and the expectation of the patient. Some variants of Poland syndrome, such as diffuse rib aplasia without depression, are not surgically correctable at all. Therefore, patients should be carefully counseled before surgery.
Jeune Syndrome
Jeune syndrome, or asphyxiating thoracic dystrophy, is a failure of chest wall growth in utero resulting in a narrow chest cavity and pulmonary hypoplasia. In 1954, Jeune first described the syndrome in a newborn. Although some patients with this syndrome may not live past infancy, many cases are now recognized with prolonged survival, and surgical options have been developed that allow for the potential of chest wall growth.
Jeune Syndrome is inherited in an autosomal recessive pattern, and no chromosomal abnormalities have been seen in association with it. The pattern of expression and the degree of pulmonary hypoplasia vary, which accounts for the longevity in certain patients.
Lateral thoracic expansion is an interesting technique that has been developed by Davis et al to enlarge the thoracic cage in patients with Jeune syndrome. [64] The procedure involves separating the ribs from their periosteum, dividing them, and then plating them together using titanium struts to increase chest diameter. One side is addressed at a time, after radiological evidence of healing (periosteal new bone formation) is noticed. Although the chest wall is enlarged in size, it still remains a fixed cylinder, and respiratory efforts entirely depend on diaphragmatic movement. However, the increase in thoracic volume provides a clinical improvement and many years of growth and freedom from ventilator-dependence have been reported. [64]
An acquired form of thoracic dystrophy has been recognized as a complication of pectus excavatum (PE) when repaired in younger children (see Pectus Excavatum). Reports of operative chest expansion in this group of patients have demonstrated encouraging short-term results. [64]
Sternal Defects
Sternal defects can be categorized into four types, all of which are rare: thoracic ectopia cordis, cervical ectopia cordis, thoracoabdominal ectopia cordis, and cleft sternum. Thoracic ectopia cordis, or naked heart, is the result of failure of somatic structures to form over the heart, leaving it completely exposed. The sternal anomalies run a spectrum from completely split to almost completely intact with a central defect. The survival rate of patients with thoracic ectopia cordis has historically been poor. Only 3 successful repairs in 29 attempts have been described.
Cervical ectopia cordis differs from thoracic ectopia cordis by the amount of superior displacement of the heart. Craniofacial abnormalities are often present and extremely severe. No survivors or successful repairs have yet been documented.
Patients with thoracoabdominal ectopia cordis have an inferiorly displaced heart underlying an inferiorly cleft sternum. The heart is covered by membrane or thin skin. Inferior displacement of the heart results from a semilunar defect in the pericardium and diaphragm. Abdominal wall defects are also common. The association of cardiac, pericardial, diaphragmatic, abdominal wall and sternal defects is also referred to as pentalogy of Cantrell. Surgical repair of thoracoabdominal ectopic cordis has been more successful when compared with the other forms of ectopic cordis.
Alloplastic materials (methyl methacrylate struts) have been used in the reconstruction of the sternal defect, and a successful 10-year follow-up of a case has been reported. [66] Initial pectoral skin flaps were used for coverage of the exposed heart, followed by definitive reconstruction. Costochondral flaps added rigidity to the repair, and a muscle flap was also used for closure of the defect. Autologous ribs have been used with minimal morbidity.
Cleft sternum is the least severe of the four anomalies because the heart is covered and is in a normal position. Overlying the heart is a partially or completely cleft sternum, and a partial split is more common than complete split. Several associations are seen with cleft sternum, but cardiac defects are rare. A bandlike scar often extends from the sternum to the umbilicus or superiorly to the neck. Hemangiomas of the head and neck can also be found.
In most infants, cleft sternum usually does not cause any detectable symptoms. On occasion, respiratory symptoms result from the paradoxical motion of the sternal defect. The primary indication for repair is to protect the heart. Repair is performed through a midline incision, and the two halves of the sternum are approximated with nonabsorbable suture. In incompletely cleft sternums, a wedge of cartilage is sometimes removed from the base of the cleft to facilitate approximation. Repair is best performed in infants because the chest wall is most pliable. [67, 68]
-
A 16-year-old boy with severe pectus excavatum. Note the appearance of the caved-in sternum and lower ribs.
-
Pectus carinatum. Photograph courtesy of K. Kenigsberg, MD.
-
Preoperative (top) and postoperative (bottom) photograph of a 12-year-old boy prior to minimally invasive repair of pectus excavatum. Note the small lateral chest wall incision and the excellent appearance of the anterior chest with 100% correction of the pectus deformity.






