Background
Pancreatitis, although uncommon during childhood, is associated with significant morbidity and mortality. Pancreatitis is characterized by inflammation of the pancreas, clinical signs of epigastric abdominal pain, and elevated serum digestive enzymes. Pancreatitis can be local or diffuse and is classified as acute, chronic, inherited, necrotic, or hemorrhagic. Occasionally, pancreatitis is complicated by the formation of a fibrous-walled cavity filled with pancreatic enzymes, termed a pseudocyst. See the images below.
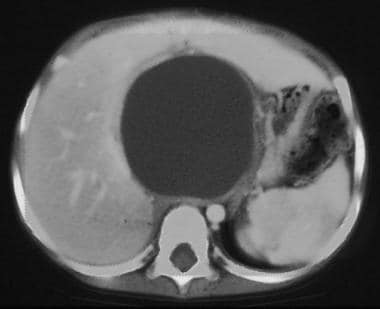 Pediatric Pancreatitis and Pancreatic Pseudocyst. This CT scan of the abdomen in the region of the pancreas demonstrates a large well-marginated cystic structure that represents a pancreatic pseudocyst.
Pediatric Pancreatitis and Pancreatic Pseudocyst. This CT scan of the abdomen in the region of the pancreas demonstrates a large well-marginated cystic structure that represents a pancreatic pseudocyst.
 Pediatric Pancreatitis and Pancreatic Pseudocyst. This real-time ultrasonography of the abdomen, with attention to the right upper quadrant, revealed a loculated fluid collection in the hilum of the liver. This was compatible with a pancreatic pseudocyst. Differential diagnosis included a large choledochal cyst.
Pediatric Pancreatitis and Pancreatic Pseudocyst. This real-time ultrasonography of the abdomen, with attention to the right upper quadrant, revealed a loculated fluid collection in the hilum of the liver. This was compatible with a pancreatic pseudocyst. Differential diagnosis included a large choledochal cyst.
Relevant Anatomy
The pancreas is divided up into a head, body, and tail, although no distinct anatomic borders indicate these divisions. Most of the pancreas is extraperitoneal, with just a portion of the tail coming through the mesenteric folds. The head is to the right of L2, the body overlies L1, and the tail rises up to the left of T12. The abdominal aorta and vena cava function to cushion the pancreas from injury against the vertebral bodies. However, with crushing or blunt abdominal trauma, the pancreas can be injured by compression against the vertebra.
Numerous congenital abnormalities of the pancreatic biliary system have been described. Pancreatic divisum, which occurs in 5-15% of the population, results from unsuccessful fusion of the embryonic ventral and dorsal pancreatic buds. As a result, the accessory duct of Santorini derived from the dorsal bud drains the majority of the pancreas. Because the accessory duct is smaller in caliber than the duct of Wirsung, inadequate pancreatic drainage may result in chronic pain and recurrent pancreatitis.
Etiology
Pancreatitis in children is uncommon and represents a diagnostic challenge for clinicians. Although most adult cases of pancreatitis are caused by alcohol abuse or gallstone disease, the etiology for pancreatitis in children is diverse. In up to 25% of cases the etiology of childhood pancreatitis is unknown. The predominant causes include the following [1] :
-
Abdominal trauma (23%) including motor vehicle collision, abuse, bicycle accident where the abdomen is compressed by the handlebars. In the United States, trauma is responsible for 15-37% of cases.
-
Anomalies of the pancreaticobiliary system (15%) including pancreaticobiliary malunion, congenital anomalies of the pancreato-biliary junction, pancreas divisum, congenital sphincter of Oddi abnormality, choledochal cysts, or choledocholithiasis
-
Multisystem disease (14%)
-
Drugs and toxins (12%) including azathioprine, tetracycline, L-asparagine, valproic acid, steroids and immunosuppressive agents
-
Viral infections (10%) such as mumps, rubella, coxsackie virus B, cytomegalovirus [CMV], human immunodeficiency virus [HIV])
-
Hereditary disorders (2%)
-
Metabolic disorders (2%) including hypertriglyceridemia, hypercalcemia, cystic fibrosis)
-
Hyperalimentation
Hereditary pancreatitis in children, the second most common congenital pancreatic disorder following cystic fibrosis, is characterized by an alteration in the long arm of chromosome 7, which yields an aberrant trypsinogen protein that may induce autodigestion of the pancreas.
Pathophysiology
The specific inciting factors causing pancreatitis remain to be elucidated. Pancreatitis may be induced by primary acinar cell injury as a result of viral infections, drugs, ischemia, and direct trauma.
Pancreatitis may originate from a disruption of the ductal system and subsequent excretion of digestive enzymes from the acinar cells of the pancreas. Normally these cells release inactive enzymes into collecting ducts, which then drain into the main or accessory pancreatic ducts emptying directly into the duodenal lumen. If obstruction or disruption of these ducts occurs, the pancreatic secretions are activated within the parenchyma of the pancreas and initiate autodigestion of the pancreatic tissue.
Interstitial edema is an early finding. Exacerbation of pancreatitis may result in pancreatic necrosis, blood vessel occlusion or disruption inciting hemorrhage, and systemic inflammatory response syndrome with multiorgan failure. Collections of pancreatic secretions often become walled off by granulation tissue to form a pseudocyst either within or adjacent to the pancreas. Predominantly, the pseudocyst is localized in the lesser sac behind the stomach. The stomach, duodenum, colon, small bowel, or omentum may abut or form part of the pseudocyst capsule.
Epidemiology
As a result of limited case reporting and underdiagnosis by physicians, the frequency and true incidence of pancreatitis in children is unknown, but is estimated to be 13 per 100,000 children. [2] Pseudocysts complicate acute pancreatitis in approximately 10-23% of cases. [3] The incidence of pancreatic pseudocysts is greater than 50% when associated with traumatic injury to the abdomen.
Prognosis
In general, the prognosis of children with acute pancreatitis is excellent, although pseudocysts have been reported to complicate 10-23% of acute episodes. In addition, when associated with abdominal trauma, the frequency rate of pseudocyst identification is higher than 50%. Approximately 60% of pancreatic pseudocysts that are caused by blunt trauma require surgical intervention.
Cases of uncomplicated acute pancreatitis usually resolve within 2-4 days. The management of acute pancreatitis is predominately supportive medical therapy, with intravenous hydration, pain control, and bowel rest. Parenteral nutrition may be required for prolonged episodes. Diagnosis of the specific cause of pancreatitis is important to elucidate, as there is a 9% recurrence rate, most of which are diagnosed with idiopathic recurrent pancreatitis or structural anomalies.
The most frequent cause of acute pancreatitis in pediatrics is related to medication administration. If a medication is suspected, it should be stopped immediately and other alternatives should be investigated. Etiologies related to trauma, systemic disease, or anatomic variants are important to determine and direct further medical or surgical interventions. Surgical management is used to address complications of pancreatitis, including hemorrhage, necrosis, ductal fistulae, and pseudocysts.
Surgical management of pancreatic pseudocysts is highly successful. Recurrence rates and mortality rates are low. Internal drainage is associated with lower recurrence rates compared to percutaneous or endoscopic drainage. Transendoscopic and percutaneous drainage of pancreatic pseudocysts have been predominately performed in the adult population, and further investigation and comparison of these techniques in children is warranted to determine the optimal management of this disease.
Complications
Although pseudocyst formation is an uncommon sequela of acute or chronic pancreatitis in children, complications of pancreatic pseudocysts include spontaneous rupture, hemorrhage, gastric outlet obstruction, [4] and infection. Pseudocysts can be medically managed with pancreatic rest or surgically by internal or external drainage. While under medical therapy, rupture is the major complication associated with pseudocysts larger than 10 cm.
-
Pediatric Pancreatitis and Pancreatic Pseudocyst. This CT scan of the abdomen in the region of the pancreas demonstrates a large well-marginated cystic structure that represents a pancreatic pseudocyst.
-
Pediatric Pancreatitis and Pancreatic Pseudocyst. This real-time ultrasonography of the abdomen, with attention to the right upper quadrant, revealed a loculated fluid collection in the hilum of the liver. This was compatible with a pancreatic pseudocyst. Differential diagnosis included a large choledochal cyst.








