Overview
Pediatric thoracic trauma has unique features that differentiate it from adult thoracic trauma. Biomechanically, the smaller body mass of a child results in greater forces applied per unit of body area on traumatic impact. In addition, the force is applied to a body that has less fat, less elastic connective tissue, and closer proximity of vital organs, especially in the thorax. The blood volume of a pediatric patient is typically 7-8% of the total body weight. Thus, a relative small blood volume loss can lead to hypovolemia and shock.
Compliance of the pediatric thorax is much greater than that of the adult thorax, because of the pliability of the cartilage and bony structure. As such, the chest can absorb a large amount of kinetic energy from the impact, which is subsequently transferred to the intrathoracic structures. Often, the child has major intrathoracic injury with minimal or no injury to the structure of the chest. Rib fractures are rare and indicate a direct blow to the chest and extreme force.
Children often experience aerophagia and gastric distention, causing elevation of the diaphragm and severe compromise of vital capacity. In infants and young children, this can predispose to the sudden development of apnea when fatigued.
As a result of the proportionately smaller size of the chest compared with the abdomen or head in a young child, significant thoracic trauma is almost always accompanied by injury to other organ systems. Thus, thoracic injury is most appropriately defined as multisystemic injury. Multisystem injury is associated with increased mortality. [1]
Epidemiology
Trauma is the leading cause of mortality in patients younger than 18 years, accounting for more than 5000 deaths annually. Although thoracic trauma accounts for only 5-12% of admissions to a trauma center, [2] it is second only to head injury as the most common cause of death.
Multisystem involvement is reported in more than 50% of children with thoracic trauma and portends a worse prognosis. Mortality is 5% for isolated thoracic trauma, approaches 20% in patients with concomitant abdominal injuries, and exceeds 30% in patients with concomitant head injuries (see the image below).
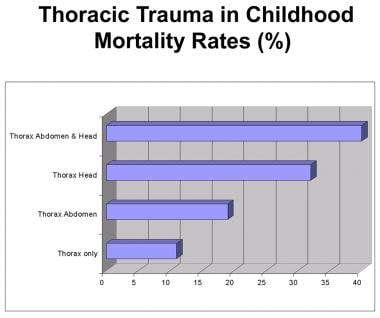 Pediatric Thoracic Trauma. Childhood thoracic injury is most appropriately defined as multisystemic injury. Mortality rates vary depending on the associated system.
Pediatric Thoracic Trauma. Childhood thoracic injury is most appropriately defined as multisystemic injury. Mortality rates vary depending on the associated system.
Analysis of the National Pediatric Trauma Registry reveals that blunt trauma accounts for approximately 85% of chest injuries serious enough to warrant treatment. [3] Almost three quarters of these chest injuries were caused by motor vehicle accidents, with the remainder attributable to motorcycle-related trauma, falls, and bicycle accidents. Penetrating injuries increase in war-torn countries.
Penetrating trauma constitutes 15% of chest injuries in children, with most caused by gunshots, knife wounds, and injury from other sharp objects. [4] Regardless of the mechanism of thoracic trauma, 15% of children do not survive. According to the analysis of the National Pediatric Trauma Registry, almost half of the deaths in patients with blunt injury result from associated neurologic injury, compared with children who have penetrating chest trauma, in whom all fatalities are from the chest injury itself. [3]
Initial Assessment
An exhaustive review of the management of airway, breathing, and circulation (ABCs) in childhood trauma resuscitation is beyond the scope of this article. Nevertheless, the principles of resuscitation do not change. Resuscitation of the child with thoracic trauma begins with a survey for immediate life-threatening injury.
Immediate life-threatening thoracic injuries include the following:
-
Airway obstruction and injury
-
Lung and chest wall injuries
-
Open pneumothorax
-
Tension pneumothorax
-
Hemopneumothorax
-
Flail chest
-
Widened mediastinum/aortic transection
-
Cardiac tamponade
Potential life-threatening thoracic injuries include the following:
-
Pulmonary contusion
-
Ruptured tracheobronchial tree
-
Ruptured diaphragm
-
Esophageal perforation
-
Myocardial contusion
Perform the primary survey and identify the injuries as quickly as possible. The immediate recognition of whether the child is agonal and hemodynamically stable and the knowledge of the mechanism of injury are implicit in the ABCs of resuscitation.
Knowledge of the mechanism of the injury is important because children who are agonal with signs of life (ie, spontaneous respirations, palpable pulses, response to stimuli, cardiac electrical activity) after penetrating trauma have a better survival rate than patients with blunt trauma. If the agonal child presents after a penetrating thoracic injury and has lost vital signs in the field or in the emergency department (ED), resuscitative thoracotomy is indicated.
In contrast, children with blunt thoracic trauma but no signs of life in the field should not undergo resuscitative thoracotomy. However, if a child has blunt trauma and the vital signs are lost in the ED, a resuscitative thoracotomy is indicated. [5, 6] Indications for thoracotomy in the ED include the following:
-
Penetrating trauma with vital signs but no response to resuscitative efforts, or vital signs present in the field but lost en route to the ED or upon admission
-
Blunt trauma with loss of vital signs en route to the ED or in the ED
The unstable child is one who has vital signs but also has clear signs or symptoms of cardiac or respiratory compromise. Poor skin perfusion (ie, capillary refill >2 sec), tachycardia, abnormal chest wall excursions, obvious mental status changes, and, possibly, hypotension all characterize instability in a child. A search for immediate life-threatening injuries is warranted. If injuries are not detected or diagnosis is delayed, these children may become agonal.
The stable child (ie, one with normal vital signs, adequate ventilation and oxygenation, normal capillary refill, adequate urine output) with thoracic trauma from a blunt or penetrating cause can be more thoroughly evaluated than others, with the added advantage of time. Injuries in stable children are potentially life-threatening, but the survival rate is generally better.
Airway Injuries
Airway injuries may be the result of oropharyngeal trauma, a foreign body, or pathology directly within the thorax that leads to a shift of the tracheobronchial tree. The two hallmarks of airway injury are obstruction and subcutaneous emphysema.
Oropharyngeal trauma is typically the result of a crush injury or direct blow. The resulting tracheal mucosal edema may be insidious, and breath sounds must be closely monitored.
Inspiratory stridor is the hallmark of airway obstruction at or above the level of the vocal cords. Blood, mucus, vomitus, teeth, or other foreign bodies may cause the stridor. This is a clinical diagnosis and must be emergently recognized and treated with removal of the obstruction.
Other signs and symptoms of airway obstruction include the following:
-
Agitation
-
Diaphoresis
-
Chest wall retractions
-
Asymmetry of respirations
-
Cyanosis
Ultimately, airway obstruction leads to bradycardia associated with severe hypoxemia. Expiratory stridor is typically the result of pathology below the cords. Children with blunt trauma who have expiratory stridor should be evaluated for a foreign-body aspiration (see the image below).
 Pediatric Thoracic Trauma. Posteroanterior chest radiograph shows aspiration of a television diode into the left mainstem bronchus. The child had blunt chest trauma as a belted passenger in a motor vehicle. Early symptoms included expiratory stridor. Retrieval was unsuccessful with a bronchoscope because the spokes of the diode were embedded in the bronchus. Left thoracotomy and bronchotomy were necessary to retrieve the diode.
Pediatric Thoracic Trauma. Posteroanterior chest radiograph shows aspiration of a television diode into the left mainstem bronchus. The child had blunt chest trauma as a belted passenger in a motor vehicle. Early symptoms included expiratory stridor. Retrieval was unsuccessful with a bronchoscope because the spokes of the diode were embedded in the bronchus. Left thoracotomy and bronchotomy were necessary to retrieve the diode.
Diminished breath sounds, wheezing, and loss of volume on plain chest radiography may not be present. A high index of suspicion is imperative. Objects may not be radiopaque, and bronchoscopy should be performed early to avoid pneumonia.
Subcutaneous emphysema
Subcutaneous emphysema can result from tracheal disruption in the neck or thorax (see the image below).
 Pediatric Thoracic Trauma. Subcutaneous emphysema of the chest and neck after tracheal disruption in a 13-year-old adolescent struck by a horse.
Pediatric Thoracic Trauma. Subcutaneous emphysema of the chest and neck after tracheal disruption in a 13-year-old adolescent struck by a horse.
Any positive pressure during expiration makes subcutaneous emphysema progress. If subcutaneous emphysema is unrecognized after intubation, it can also be worsened by positive pressure from mechanical ventilation.
Management of airway injuries
Standard management begins with head positioning, suctioning, in-line cervical spine stabilization, and administration of supplemental oxygen. Obviously, obstruction above the vocal cords must be recognized and removed. Intubation may be necessary; if intubation is not possible, needle cricothyrotomy or tracheostomy is indicated. In unconscious patients, control of the airway must always be the first management step.
Subcutaneous air solely in the neck may indicate pathology in the trachea. Rupture of the tracheobronchial tree (partial or complete) is relatively uncommon in children because of the elasticity of the chest wall, but a persistent air leak after decompression of a pneumothorax is suggestive of a bronchial tear. Typical points of disruption include fixed points such as the carina or segmental branches of the bronchus.
These injuries are commonly diagnosed with the aid of a bronchoscope, and the injury's location determines the subsequent treatment approach. However, bronchoscopy frequently leads to an underestimation of the magnitude of the injury. Delays in treatment can be life-threatening because both ventilation and oxygenation can be affected.
Nonoperative management may be attempted for small injuries that encompass less than a third of the airway circumference. Short longitudinal tears of a single airway are particularly likely to be successfully managed in this manner.
If the air leak is massive and ventilation is difficult, nonoperative management should not be attempted, even if the injury is less than one third of the circumference of the airway. Injuries to the cervical trachea should be approached via a transverse neck incision. If injury is to the distal trachea or right mainstem bronchus, it should be approached via a right thoracotomy; localized injury to the left mainstem bronchus should be approached via the left chest.
Few patients with a complex injury that involves the carina or both mainstem bronchi require cardiopulmonary bypass. Most tracheobronchial injuries can be primarily repaired, provided that the suture line is tension free. Because of the mechanisms of these injuries, blast effect and reduced blood flow to the perimeter of the injury must be suspected, and if necessary, a widened excision must be performed.
After closure of the airway defect, the endotracheal tube should be positioned so that the cuff of the tube does not abut the repair. Moreover, a vascularized tissue flap of pleura, pericardium, or muscle should be used to reinforce the repair.
Chest Wall and Lung Injuries
Compared with adults, children have more cartilage in their ribs, leading to an elastic and highly compliant thorax. This compliance diffuses the force of impact, leading to fewer rib fractures than result from similar trauma in an adult. Although splitting from pain is common in children, atelectasis is less common due to the propensity of children to cry.
Diagnosis of acute rib fractures is made with radiography. Multiple rib fractures in a child should always raise the suspicion of child abuse. Oral analgesics are usually sufficient for pain control. Rarely, an intercostal nerve block may be necessary.
Flail segments are defined as two or more ribs fractured in two or more places. The flail segment results in ventilation-perfusion mismatch, atelectasis, and progressive shunting. In general, patients with an unstable chest wall should be treated with positive pressure and pain control.
Bleeding from within the chest (see the image below) is rare in children, mainly because of the low incidence of rib fractures. When chest bleeding does occur, it can be insidious and life-threatening. Bleeding is typically from an intercostal vessel or vessels, parenchyma, or chest wall. Regardless of the source, a hemothorax must be evacuated to avoid atelectasis, ventilation-perfusion mismatch, fibrothorax, and a restrictive lung. Treatment involves tube decompression.
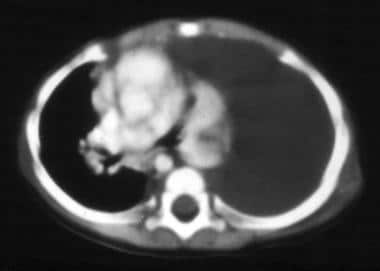 Pediatric Thoracic Trauma. CT scan of chest shows a hemothorax on the left side. This can be an insidious, life-threatening injury in children mainly because rib fractures are so rare.
Pediatric Thoracic Trauma. CT scan of chest shows a hemothorax on the left side. This can be an insidious, life-threatening injury in children mainly because rib fractures are so rare.
Initial hemorrhage of more than 20 mL/kg or continued blood loss of more than 2-3 mL/kg/hr for 3 consecutive hours may be an indication for open thoracotomy. Moreover, inability to adequately drain the chest and reexpand the lung is an additional criterion for thoracotomy. Lobectomy is far less common than stapling of bleeding or simple wedge resection.
Minimally invasive thoracoscopy for trauma has become more widespread. Video-assisted thoracic surgery (VATS) can be used as a diagnostic tool in an acute or subacute hemodynamically stable patient with hemothorax.
In certain patients with a large initial drainage or continuing blood loss from chest injury, VATS may aid in avoiding thoracotomy by visualizing a nonbleeding injury, evacuating a hematoma, allowing tamponade by fully expanding the lung, or cauterizing or ligating bleeding vessels. Moreover, in patients with empyema after chest injury, thoracoscopy can be effective in completely draining the pleural space and in removal of any organizing peel from the lung. [7]
Pneumothorax
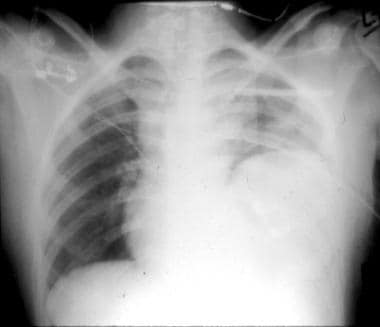
Pneumothorax may result from puncture of the lung by a rib, by a penetrating chest wall injury, by disruption of the pulmonary parenchyma, or by injury to the tracheobronchial tree. Neither simple pneumothorax nor tension pneumothorax is well tolerated in children because of the lack of fixation of the mediastinum. However, less than 15% of cases of childhood thoracic trauma require thoracotomy. An untreated simple pneumothorax eventually leads to a tension phenomenon (see the image below).
 Pediatric Thoracic Trauma. Tension pneumothorax of the right lung after blunt chest trauma. Note the mediastinal shift and deviation of the trachea.
Pediatric Thoracic Trauma. Tension pneumothorax of the right lung after blunt chest trauma. Note the mediastinal shift and deviation of the trachea.
If the pressure in the pleural space with tension pneumothorax becomes high enough, both respiration and hemodynamics are impaired. The increased intrapleural pressure shifts the mediastinum. This, in turn, compromises venous return, with an obligatory decrease in cardiac output. Pneumothorax is a clinical diagnosis and does not require radiographic confirmation for treatment.
Performing needle decompression through the second intercostal space at the level of the midclavicular line followed by tube decompression, or simply proceeding to tube decompression, is the treatment of choice. Chest radiography should follow to confirm tube position and reinflation of the lung. An open pneumothorax associated with a sucking chest wound causes pathophysiology because a path of less resistance is created for tracheobronchial air. To prevent this airflow, the wound must be covered and tube decompression must follow.
Pulmonary contusion
Pulmonary contusion is the most common thoracic injury in children and represents a defining contrast between children and adults. In contrast to rib fractures in adults after blunt trauma, the kinetic energy of blunt chest trauma is transmitted to the compliant chest wall in children. Thus, both pulmonary contusion and hemorrhage are far more common than pneumothorax. [8] Pulmonary contusion from a car or truck rollover injury in children is a common phenomenon.
Typical chest radiographic findings (see the image below) include multiple opacifications corresponding to intraparenchymal hemorrhage. Hypoxia from shunting and ventilation perfusion mismatch, in addition to radiographic findings, is characteristic of pulmonary contusion. Successful treatment involves aggressive pulmonary toilet and pain management. Resolution of the contusion within a few days is not uncommon. After comparing the clinical findings from chest computed tomography imaging and chest radiographs, Holscher et al concluded that CT did not add to the management of the trauma and increased the risk from radiation. [9]
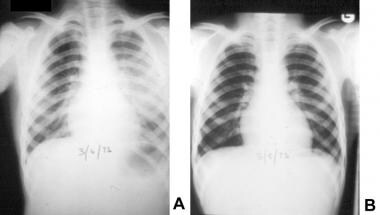 Pediatric Thoracic Trauma. Posteroanterior chest radiographs reveal the natural history of pulmonary contusion after blunt chest trauma. (A) On the day of the injury, multiple opacifications are present and correspond to multiple intraparenchymal hemorrhages. (B) After 2 days of pain management and aggressive chest physiotherapy, substantial resolution of the contusion is seen.
Pediatric Thoracic Trauma. Posteroanterior chest radiographs reveal the natural history of pulmonary contusion after blunt chest trauma. (A) On the day of the injury, multiple opacifications are present and correspond to multiple intraparenchymal hemorrhages. (B) After 2 days of pain management and aggressive chest physiotherapy, substantial resolution of the contusion is seen.
Sequelae of pulmonary contusion include pneumonia and posttraumatic pseudocysts. These typically resolve with antibiotics and time.
Penetrating pulmonary injury
Pulmonary injury secondary to penetrating trauma can vary from small pleural or parenchymal lacerations from a stab wound to massive pulmonary injury secondary to a gunshot wound. The basics of airway, breathing, and circulation management (ABCs) remain paramount.
If the patient has sustained a penetrating missile injury and injury to mediastinal structures is suspected, radiographic evaluation of the tracheobronchial tree, esophagus, and great vessels should be performed. Asymptomatic patients with normal chest radiography findings can be safely observed and discharged after an appropriate time interval (minimum of 6 hr).
Most pulmonary lacerations do not require surgery and can be treated with tube thoracostomy. Drainage of the pleural space with reapposition of the pleural surfaces often tamponades low pressure venous bleeding and seals small air leaks. Surgical exploration of thoracic wounds is not recommended because of the potential to cause pneumothorax and contaminate the pleural space.
Absolute indications for surgery include exsanguination and uncontrollable air leak from the chest cavity. If thoracotomy is necessary, parenchymal sparing techniques and nonanatomic resections are preferable.
A posterolateral thoracotomy is used to gain access to the hilum of the lung. Lung isolation is obtained with a double-lumen tube or bronchial blocker. As with all thoracotomies for penetrating thoracic trauma, the hilum and pulmonary vessels are controlled early to allow rapid vascular control, should an unsuspected central injury be present. Stapling with a generous margin around the area of injury should be performed.
Persistent bleeding from deep missile injuries can be opened and exposed by inserting the anvil of the linear stapler into the tract and firing the device to perform a tractotomy. [10] If extensive tissue loss is apparent, anatomic resection of the injured lobe may be necessary.
Air embolism is a potential complication of penetrating lung injury. Seizures and sudden cardiac arrest may be the only clues to this near-fatal event. Treatment involves thoracotomy, clamping of the hilum, and aspiration of air from the left ventricle and aorta.
Penetrating injury to the mediastinum can occur without a pneumothorax. Therefore, a stab wound between the nipples can injure the heart or great vessels without damaging either pleural space. Moreover, because the abdomen begins at the nipple line in children, injury below the diaphragm should be ruled out when a stab wound occurs at this level.
Traumatic asphyxia (see the image below) occurs in children because of their flexible thoracic wall and the absence of valves in the venous system of the inferior and superior vena cava. Direct compression of the chest wall may be sustained when a child is involved in a motor vehicle collision or crush injury. At the time of injury, if the glottis is closed and the thoracoabdominal muscles are tensed, the increased intrathoracic pressure is transmitted through the central venous system to organs such as the brain, liver, spleen, and kidneys.
The sudden increase in pressure produces subconjunctival hemorrhage and petechiae of the chest, shoulders, and head. In addition, capillaries in the upper body become atonic and dilated. Desaturation of the stagnant capillary blood produces a characteristic bronzed discoloration.
 Pediatric Thoracic Trauma. Traumatic asphyxia is produced by a sudden increase in intrathoracic pressure against a closed glottis or compressed tracheobronchial tree. (A) Bronze discoloration and petechiae on the chest, shoulders, and head are typical initial signs. (B) What is frequently overlooked is the potential pathology within the oropharynx, specifically under the tongue. Most of the petechiae should disappear in a few weeks.
Pediatric Thoracic Trauma. Traumatic asphyxia is produced by a sudden increase in intrathoracic pressure against a closed glottis or compressed tracheobronchial tree. (A) Bronze discoloration and petechiae on the chest, shoulders, and head are typical initial signs. (B) What is frequently overlooked is the potential pathology within the oropharynx, specifically under the tongue. Most of the petechiae should disappear in a few weeks.
Central nervous system and pulmonary dysfunction can be associated with traumatic asphyxia, but this is rare. These children should be monitored in the intensive care unit for 24 hours because of the potential for airway obstruction secondary to venous hypertension and petechiae generated under the tongue and oropharynx. Despite the cutaneous manifestations, most of the petechiae disappear in a few weeks.
Widened Mediastinum and Aortic Disruption
Blunt trauma can injure the aorta or branches of the aortic arch. Approximately 95% of patients with blunt tears of the thoracic aorta die before reaching the hospital. These are exceedingly rare injuries in children. The typical mechanism, as in adults, is a rapid deceleration injury sustained in a motor vehicle accident, an auto-pedestrian accident, or a fall from a height. Suspicion of this injury in a stable patient may only come from chest radiography depicting a widened mediastinum (see the image below).
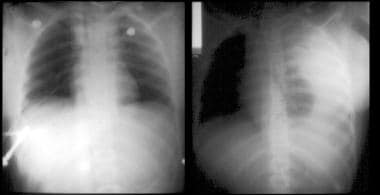 Pediatric Thoracic Trauma. Left: Plain chest radiographs depicts a widened mediastinum. Minutes after resuscitation, vital signs were lost in this 12-year-old child, who had a deceleration injury to the chest. Right: Image illustrates what happens when the aorta ruptures. This is frequently a lethal injury despite emergency thoracotomy and aortic cross-clamping. A large tear was found at the level of the ligamentum arteriosum.
Pediatric Thoracic Trauma. Left: Plain chest radiographs depicts a widened mediastinum. Minutes after resuscitation, vital signs were lost in this 12-year-old child, who had a deceleration injury to the chest. Right: Image illustrates what happens when the aorta ruptures. This is frequently a lethal injury despite emergency thoracotomy and aortic cross-clamping. A large tear was found at the level of the ligamentum arteriosum.
Radiographic signs of mediastinal pathology are as follows:
-
Straightening of the mediastinal borders, with loss of the anteroposterior (AP) window
-
Mediastinal diameter greater than that of the hemithorax
-
Right shift of an orogastric tube off the vertebral column
Radiographic signs of disruption of the aorta, which typically occurs at the ligamentum arteriosum, include the following:
-
Widened mediastinum
-
Left pleural effusion
-
Apical capping
-
Depression of the left main bronchus
-
Rightward shift of an orogastric tube off the vertebral column
-
Fractures of the first or second rib or scapula
Upper extremity hypertension, interscapular murmurs, and diminished or absent pulses in upper or lower extremities are common physical signs.
Aortography is the diagnostic procedure of choice if the child is stable (see the image below). Computed tomography scanning is an alternative in that it can be rapidly performed in concert with imaging of the brain, abdomen, and pelvis.
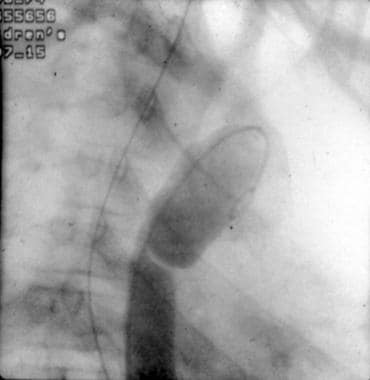 Pediatric Thoracic Trauma. Lateral aortograph shows a tear at the level of the ligamentum arteriosum. If the child is stable, aortography is the procedure of choice for evaluating the aorta in the presence of a widened mediastinum.
Pediatric Thoracic Trauma. Lateral aortograph shows a tear at the level of the ligamentum arteriosum. If the child is stable, aortography is the procedure of choice for evaluating the aorta in the presence of a widened mediastinum.
Treatment
If a contained hematoma is identified, open repair via a left posterolateral thoracotomy, either with primary anastomosis or placement of synthetic grafts, is the standard of care. In the acute setting, this is associated with significant morbidity and mortality due to multisystem injury. Delaying intervention with the use of beta-blockers and antihypertensive agents until the patient is more stable has improved results, but complications remain high. [11]
Successful surgical intervention is predicated on achieving proximal and distal control of the aorta. Historically, the "clamp-and-sew" technique was favored. However, due to the potential for ischemic injury to the spinal cord, several adjuncts have been developed to maintain distal aortic perfusion during surgical repair.
A heparin-bonded Gott shunt may be used to shunt blood from the proximal aorta to the distal aorta or femoral artery without the use of a pump. Partial left-heart bypass uses a centrifugal pump that draws oxygenated blood from the left atrium, which is reinfused to the distal thoracic aorta or femoral artery. Like the Gott shunt, this technique avoids full systemic heparinization. Nevertheless, both of these techniques require that cannulas be present in the operative field, which often prevents adequate visualization in smaller children.
Femoral-femoral cardiopulmonary bypass using an oxygenator maintains lower-body perfusion, allows for systemic cooling with spinal cord protection, and allows for easy control of hypertension proximal to the aortic cross-clamp. The major disadvantage with this approach is the need for systemic heparinization, which may be a relative contraindication in patients with major associated abdominal injuries or intracranial hemorrhage.
The safety and efficacy of endovascular techniques has been established in adolescents and children. Endovascular stenting allows for definitive treatment of the vascular injury without the need for bypass and reduces the recovery time that is associated with a thoracotomy. Currently, long-term follow-up is required. [12, 13, 14, 15, 16, 17]
A diagnostic dilemma may result when clinicians encounter a stable transected aorta and associated life-threatening abdominal pathology. In a patient with a stable thoracic hematoma, treatment includes evaluation and repair of the abdominal injuries first, followed by a left thoracotomy for management of the transected aorta. In a child with a rapidly expanding hematoma of the chest and concomitant abdominal pathology, thoracotomy should be performed first.
Cardiac Injuries
Blunt injuries of the myocardium range from mild asymptomatic contusion to cardiac rupture. Myocardial contusion is the most common injury. The pathophysiology involves reduction in blood flow to a contused cardiac muscle, followed by ischemia.
The hallmarks of myocardial contusion are ischemic changes or atrial or ventricular premature contractions or wall motion abnormalities during echocardiography. Sequelae of myocardial contusion are uncommon in patients who demonstrate hemodynamic and cardiac stability upon admission.
No reliable standards for diagnosis have been determined. Studies such as creatine kinase–MB (CK-MB) fraction, troponin I, and echocardiography are generally not helpful in either diagnosis or treatment planning. The presence of dysrhythmias is suggestive; patients with ectopy or ischemic changes require monitoring in the intensive care unit for 24 hours after injury. Echocardiography is required for any new onset of a murmur. Repair is indicated if ischemia and myocardial dysfunction are severe and salvageable myocardium is found.
Most patients with rupture of the myocardium do not reach the hospital alive. However, the injury is occasionally contained by the pericardium, and the child presents in shock from a combination of hemorrhage and cardiac tamponade. [18] The mechanism of injury is likely sudden severe compression of the chest at the end of diastole. The right ventricle is most frequently involved (46%), followed by the left ventricle (35%), right atrium (26%), and left atrium (6%).
The prognosis of patients with left atrial and right-sided injuries is intermediate, whereas very few survive rupture of the left ventricle. Blunt cardiac rupture is treated surgically via sternotomy or left thoracotomy for isolated left atrial rupture.
Penetrating cardiac injuries
Penetrating wounds of the heart usually result in two pathophysiologic events. One is that blood leaks from the heart into the pleural space and causes a hemothorax. This diagnosis should be suspected in patients with hemodynamic instability from hemorrhagic shock or persistent bleeding from the chest tube.
The other scenario is accumulation of blood in the pericardial space. Often, the traumatic wound may be occluded by pressure in the pericardial space, preventing frank exsanguination. More commonly, however, the ongoing accumulation of blood leads to pericardial tamponade. Muffled heart sounds, distended neck veins, and hypotension constitute the diagnostic triad (ie, Beck triad) that defines cardiac tamponade.
Penetrating wounds can involve any of the four chambers of the heart but are most common in the right ventricle because of its anterior location. The presence of hemopericardium on transthoracic echocardiography or subxiphoid pericardial window mandates urgent sternotomy or thoracotomy for repair of cardiac injury.
Sternotomy is advantageous because it allows access to all cardiac chambers and, if necessary, institution of cardiopulmonary bypass. Repair should be performed using nonabsorbable sutures with atraumatic needles and pledgets to prevent sutures from pulling through myocardium. Nonmyocardial cardiac injuries are also possible. Rupture of the pericardium can occur with or without associated cardiac injury.
Laceration or thrombosis of the coronary arteries from blunt trauma is rare but possible. Diagnosis is made via electrocardiogram and cardiac catheterization.
For cardiac tamponade, subxiphoid needle pericardiocentesis is the treatment of choice. Directing a catheter at a 45° angle toward the left scapula and using a Seldinger technique to maintain the catheter in the pericardial space facilitates continued aspiration of the pericardial sac until emergency left thoracotomy or median sternotomy (depending on the associated pathology) can be performed. Aspiration of as little as 5 mL of nonclotted blood relieves the tamponade in infants.
Time constraints often do not permit application of an alligator clip to avoid puncture of the heart muscle. Radiographic or echocardiographic testing is not needed to make the diagnosis.
Commotio cordis results from a sudden impact of the heart against the anterior chest wall that results in cessation of normal cardiac function. The precordial blow that triggers commotio cordis is not usually perceived to be of a significant magnitude to cause death.
The typical scenario is a child who collapses after sustaining a chest blow during a sporting event. Because of the heightened compliance of the pediatric chest, the kinetic energy from the blow is transmitted to the myocardium. Survival rates have been as low as 15%; however, with the awareness of this condition and increased availability of automatic external defibrillators at schools and athletic facilities, survival for athletes who sustain such injuries have improved. From 1970-1993, the survival rate was only 10%. The survival rate from 2006-2012 has increased to 58%. [19]
Surgical Strategies for Heart and Great Vessel Injury
Operative approaches to treat specific thoracic injuries are as follows:
-
Cardiac tamponade: left anterior or anterolateral thoracotomy (fifth intercostal space)
-
Heart, great vessels, or pulmonary hilum: median sternotomy and extension into the neck
-
Descending thoracic aorta: left posterolateral thoracotomy (fourth and fifth intercostal spaces)
-
Ascending aorta: median sternotomy (cardiopulmonary bypass is usually required to repair a blunt injury; penetrating injuries can be repaired without bypass)
-
Aortic arch: median sternotomy with extension into the neck for great vessel exposure
-
Innominate artery: median sternotomy with right cervical extension if necessary
-
Subclavian artery: cervical extension of median sternotomy for right subclavian artery injury or a supraclavicular approach for left subclavian artery injury (proximal control of either vessel is best via an anterolateral thoracotomy above the nipple)
-
Carotid artery injury: right cervical incision for right carotid artery injury or, as in innominate artery injury, median sternotomy with left cervical extension for left carotid artery injury
-
Pulmonary artery: respective side thoracotomy for hilar control
Diaphragm Rupture
An elevated left hemidiaphragm indicates a ruptured diaphragm until proven otherwise (see the image below). Aids to this diagnosis include the position of an orogastric tube on plain radiograph. In addition, bowel sounds in the chest are suggestive of the injury.
 Pediatric Thoracic Trauma. Posteroanterior chest radiography depicts an elevated left hemidiaphragm and bowel loops on the chest. Bowel sounds were audible in the chest. The injury involved blunt chest trauma at the level of the nipple; this finding enforced the concept that the abdomen in children begins at the level of the nipple. These injuries should be repaired from the abdomen because of the potential for associated intra-abdominal pathology.
Pediatric Thoracic Trauma. Posteroanterior chest radiography depicts an elevated left hemidiaphragm and bowel loops on the chest. Bowel sounds were audible in the chest. The injury involved blunt chest trauma at the level of the nipple; this finding enforced the concept that the abdomen in children begins at the level of the nipple. These injuries should be repaired from the abdomen because of the potential for associated intra-abdominal pathology.
Diaphragm injuries are far more common on the left than on the right because of the protection of the liver; they can go unnoticed, especially in an intubated patient. Moreover, relatively common injuries to the liver obscure suspected diaphragmatic injuries on the right side. [20] The diaphragm can rupture in any location, but ruptures of the central tendon and the lateral attachments of the torso wall are the most common.
Management of a ruptured diaphragm must account for the possibility of associated abdominal pathology. The abdomen begins at the nipple level in children, so a high index of suspicion is warranted after blunt or penetrating injury. Laparoscopy is helpful for penetrating injuries that are at or below the nipple and for which there is no apparent pathology on CT scanning of the abdomen. Diaphragmatic rupture that results from blunt trauma should be approached through a laparotomy because of the high incidence of intra-abdominal solid organ injuries.
If the patient is symptomatic and visceral ischemia is a possibility, the approach should always be through the abdomen. A thoracotomy approach may be advantageous for injury or hernias that present in a delayed fashion, especially of the right hemidiaphragm. This approach provides excellent exposure to allow for division of adhesions between trapped viscera and lung parenchyma.
When the tear is located, any herniated viscera should be returned to the abdomen and inspected for bleeding or ischemia. The rupture should be repaired with either monofilament nonabsorbable or absorbable sutures. If not already present, a chest tube should be placed on the affected side.
In the event that a tension-free repair cannot be primarily performed, a pedicled intercostal muscle flap can be used to bridge the defect in children. [21] . Other alternatives include fascia lata, bovine pericardium, or synthetic material such as Gore-Tex or Marlex.
Esophageal Perforation
Esophageal injuries can be due to various mechanisms. The most common cause is endoscopic trauma from esophagoscopy, dilation, or transesophageal echocardiography. Other causes include the following:
-
Blunt trauma
-
Barometric trauma (eg, Boerhaave syndrome, air-pressure injury)
-
Penetrating trauma
-
Caustic injury
-
Foreign body
Patients with perforations of the cervical esophagus can present with neck pain, cervical dysphagia, dysphonia, or bloody regurgitation. Intrathoracic perforations can rapidly contaminate the mediastinum, leading to chest pain, tachycardia, tachypnea, fever, and leukocytosis.
Expeditious diagnosis of esophageal injury is important because early diagnosis significantly reduces the rate of complication and mortality. Diagnosis of cervical esophageal perforation is aided by lateral roentgenography, which may reveal air in the prevertebral fascial planes. Plain radiography may reveal mediastinal widening with or without an air-fluid level, subcutaneous emphysema, and a pleural fluid collection.
When a leak is suspected, a contrast study should be performed. Water-soluble contrast agents (eg, Gastrografin) are advocated for first-line screening. If no perforation is initially detected with a water-soluble agent, the examination should be repeated with dilute barium sulfate.
A broad clinical spectrum of esophageal trauma is recognized, ranging from contained small leaks that are recognized early to large leaks with severe mediastinal infection. The general principles of management are directed toward limiting contamination, encouraging healing of the perforation by repair or drainage, and maintaining nutrition of the patient.
The treatment algorithm centers on whether preexisting esophageal disease is present and whether the perforation is contained. Rarely, a well-contained leak can be managed with careful observation, nothing by mouth (NPO), broad-spectrum antibiotics, and intravenous feeding. The barium swallow is repeated at weekly intervals. If the leak is not contained, the site of perforation dictates further management.
Esophageal injury in the neck, if seen early, is repaired and reinforced with adjacent muscle or tissue and drained. If the leak is seen late, only the abscess is drained without an attempt to repair the injury. Esophageal leaks into the chest are managed by thoracotomy and repair, whether discovered early or late. This is a paradigm shift, in that it was previously felt that late repair was associated with failure and increased mortality.
In general, the upper and mid esophagus are best approached through the right side of the chest, whereas the lower third of the esophagus and the esophagogastric junction are best approached through the left side of the chest. Some pleural or intercostal muscular covering should accompany debridement and primary repair. Wide drainage of both the mediastinum and pleural space is mandatory.
If inflammation is substantial and if the injury is extensive, cervical esophagostomy is necessary, followed by eventual esophageal replacement. Surgeons should attempt to use the native esophagus in a growing child by all means possible.
Video-assisted thoracoscopic drainage for esophageal perforation with mediastinitis in children has been shown to be feasible and effective. [22] Peng et al reported no deaths in 8 children treated with thoracoscopic mediastinal debridement, with a mean hospital length of stay of 34 days. Delay between onset of primary perforation and hospitalization ranged from 2-12 days (median length, 5.2 days). All patients had a localized collection on contrast study. These authors concluded that perforations in children heal with debridement and drainage alone. Although these data are encouraging, they have not been validated.
-
Pediatric Thoracic Trauma. Childhood thoracic injury is most appropriately defined as multisystemic injury. Mortality rates vary depending on the associated system.
-
Pediatric Thoracic Trauma. Posteroanterior chest radiograph shows aspiration of a television diode into the left mainstem bronchus. The child had blunt chest trauma as a belted passenger in a motor vehicle. Early symptoms included expiratory stridor. Retrieval was unsuccessful with a bronchoscope because the spokes of the diode were embedded in the bronchus. Left thoracotomy and bronchotomy were necessary to retrieve the diode.
-
Pediatric Thoracic Trauma. Subcutaneous emphysema of the chest and neck after tracheal disruption in a 13-year-old adolescent struck by a horse.
-
Pediatric Thoracic Trauma. CT scan of chest shows a hemothorax on the left side. This can be an insidious, life-threatening injury in children mainly because rib fractures are so rare.
-
Pediatric Thoracic Trauma. Tension pneumothorax of the right lung after blunt chest trauma. Note the mediastinal shift and deviation of the trachea.
-
Pediatric Thoracic Trauma. Posteroanterior chest radiographs reveal the natural history of pulmonary contusion after blunt chest trauma. (A) On the day of the injury, multiple opacifications are present and correspond to multiple intraparenchymal hemorrhages. (B) After 2 days of pain management and aggressive chest physiotherapy, substantial resolution of the contusion is seen.
-
Pediatric Thoracic Trauma. Traumatic asphyxia is produced by a sudden increase in intrathoracic pressure against a closed glottis or compressed tracheobronchial tree. (A) Bronze discoloration and petechiae on the chest, shoulders, and head are typical initial signs. (B) What is frequently overlooked is the potential pathology within the oropharynx, specifically under the tongue. Most of the petechiae should disappear in a few weeks.
-
Pediatric Thoracic Trauma. Left: Plain chest radiographs depicts a widened mediastinum. Minutes after resuscitation, vital signs were lost in this 12-year-old child, who had a deceleration injury to the chest. Right: Image illustrates what happens when the aorta ruptures. This is frequently a lethal injury despite emergency thoracotomy and aortic cross-clamping. A large tear was found at the level of the ligamentum arteriosum.
-
Pediatric Thoracic Trauma. Lateral aortograph shows a tear at the level of the ligamentum arteriosum. If the child is stable, aortography is the procedure of choice for evaluating the aorta in the presence of a widened mediastinum.
-
Pediatric Thoracic Trauma. Posteroanterior chest radiography depicts an elevated left hemidiaphragm and bowel loops on the chest. Bowel sounds were audible in the chest. The injury involved blunt chest trauma at the level of the nipple; this finding enforced the concept that the abdomen in children begins at the level of the nipple. These injuries should be repaired from the abdomen because of the potential for associated intra-abdominal pathology.
-
Pediatric Thoracic Trauma. Subcutaneous emphysema and pneumothorax.






