Practice Essentials
Mesenteric cysts most commonly occur in the small-bowel mesentery on the mesenteric side of the bowel. They can often be shelled out from between the leaves of the mesentery with care taken to avoid damage to the mesenteric vessels, or they may require concomitant bowel resection in order to ensure that the blood supply to the bowel is not compromised. [1, 2, 3] In a series from Egleston Children's Hospital in Atlanta, one third of patients required intestinal resection along with resection of the mesenteric cysts. [4] Omental cysts can always be removed without resecting the adjacent transverse colon or the stomach. [1, 2]
No specific laboratory studies aid in the diagnosis of mesenteric and omental cysts. Aside from imaging studies, no tests or diagnostic procedures are necessary. (See Workup.)
No medical therapy is available. In children with mesenteric or omental cysts, the most common indication for surgical intervention is the presence of an abdominal mass with or without signs of intestinal obstruction. Although the preferred treatment of mesenteric cysts is enucleation, intestinal resection is frequently required. If neither enucleation nor resection is possible, the third option is partial excision with marsupialization of the remaining cyst into the abdominal cavity. (See Treatment.)
Pathophysiology
Mesenteric and omental cysts can be either simple or multiple and either unilocular or multilocular, and they may contain hemorrhagic, serous, chylous, or infected fluid. [4] The fluid is serous in ileal and colonic cysts and chylous in jejunal cysts. The cysts can range in size from a few millimeters to 40 cm in diameter. (See the images below.)
 Small omental cyst arising on a pedicle from the greater omentum in the region of the transverse colon.
Small omental cyst arising on a pedicle from the greater omentum in the region of the transverse colon.
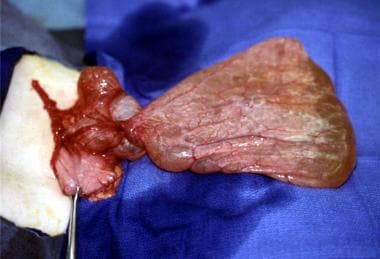
 Huge mesenteric cyst arising from the transverse colon mesentery. Resection was required to remove this cyst.
Huge mesenteric cyst arising from the transverse colon mesentery. Resection was required to remove this cyst.
Etiology
As proposed by Gross, [5] mesenteric and omental cysts are thought to represent benign proliferations of ectopic lymphatics that lack communication with the normal lymphatic system. [6] Cysts are thought to arise from lymphatic spaces associated with the embryonic retroperitoneal lymph sac; this makes them analogous to cystic hygromas, which arise in the neck in association with the jugular lymph sac. [7]
Another proposed etiology is lymphatic obstruction. [1] However, experimental occlusion of lymphatic channels in animals has not been found to produce mesenteric or omental cysts, because of the rich collaterals in the lymphatic system; this finding has shed doubt on the lymphatic obstruction theory. [7] Other etiologic theories that have been advanced include the following [4] :
-
Failure of the embryonic lymph channels to join the venous system
-
Failure of the leaves of the mesentery to fuse
-
Trauma
-
Neoplasia
-
Degeneration of lymph nodes
Another variation includes chylous mesenteric cysts, which have a slight male to female preponderance of 1.4:1; presentation is usually in the fourth decade of life. [8] Primary mesenteric hydatid cysts have also been reported; these are extremely rare and present with chronic lower abdominal pain. [9]
Mesenteric cysts have been reported in association with Costello syndrome, which consists of short stature; redundant skin of the neck, palms, soles, and fingers; curly hair; papillomata around the mouth and nares; and intellectual disability. [10]
Mesenteric cysts can occur anywhere in the mesentery of the gastrointestinal (GI) tract from the duodenum to the rectum, and they may extend from the base of the mesentery into the retroperitoneum. [4] In a series of 162 patients, 60% of mesenteric cysts occurred in the small-bowel mesentery, 24% in the large-bowel mesentery, and 14.5% in the retroperitoneum. [11] They most commonly occur in the ileal mesentery of the small bowel or the sigmoid mesentery of the colon.
Omental cysts are confined to the lesser or greater omentum. [2] Congenital omental cysts that present as abdominal distention have been reported. [12] Omental cysts may be a result of dermoid cysts [13] or teratomas. [14]
Epidemiology
Mesenteric and omental cysts are rare; the incidence is about 1 per 140,000 general hospital admissions and about 1 per 20,000 pediatric hospital admissions. In a study from Egleston Children's Hospital at Emory University from 1965 to 1994, 14 patients were treated for mesenteric or omental cysts, which represents a prevalence of about 1 case per 11,250 admissions. [4]
Approximately one third of mesenteric cysts occur in children younger than 15 years. [6] The mean age of children affected is 4.9 years. [6, 15, 2, 16, 17] Mesenteric cysts are 4.5 times more common than omental cysts.
Prognosis
Overall results in pediatric patients are favorable. The recurrence rate ranges from 0% to 13.6%, [6, 16, 17] averaging about 6.1% in a series of 162 adults and children. [11] Most recurrences occur in patients with retroperitoneal cysts or those who had only a partial excision. [16, 17]
Essentially no mortality is associated with mesenteric or omental cysts in children. In a series from Egleston Children's Hospital in Atlanta, no major postoperative complications, recurrences, or deaths occurred. [4]
-
Large mesenteric cyst arising from the small-bowel mesentery.
-
Huge omental cyst within the greater omentum.
-
Small omental cyst arising on a pedicle from the greater omentum in the region of the transverse colon.
-
Multiple mesenteric cysts, some filled with chyle, arising from the jejunal mesentery.
-
Huge mesenteric cyst arising from the transverse colon mesentery. Resection was required to remove this cyst.
-
Multiple jejunal mesenteric cysts surrounding a loop of jejunum. Intestinal resection was required to remove these cysts.
-
Ultrasound image demonstrating a thin-walled mesenteric cyst with an internal septum.