Background
Genital complaints in prepubertal girls are not rare, and all clinicians who examine children need to be familiar with the conditions that can cause genital redness, itching, discharge, bleeding, and pain. Physicians, nurse practitioners, nurses, and physician assistants who examine children must know the wide variations of normal in the appearance of the genital tissues so as to avoid unnecessarily raising the suspicion of sexual abuse if the child gives no disclosure.
Most cases of genital redness, itching, discharge, bleeding, or pain in prepubertal girls have benign causes and respond to the removal of irritants. [1] However, because a genital complaint such as discharge or bleeding may be caused by trauma to the area or a sexually transmitted infection, assessment of each patient requires the clinician to be sensitive to possible unspoken concerns of parents regarding suspicions of molestation. [2, 3]
When a child makes a statement or a disclosure of abuse and describes sexual touching, all 50 US states mandate that the clinician report suspected child sexual abuse to the local child protective services agency, law enforcement, or both. However, if concerns about possible abuse are based only on a physical sign or symptom, the child must be examined by a healthcare provider who is familiar with the nonabusive causes of the symptoms or signs. Understanding the wide variations in the appearance of the hymen and other genital tissues in prepubertal girls is also necessary.
In 2013, the American Academy of Pediatrics (AAP) published an updated clinical report on the subject of suspected child sexual abuse with guidance for the clinician in deciding when a report to protective services is necessary. [4] In 2016, Adams et al published updated guidelines for medical care of children with suspected sexual abuse, [5] and in 2018, these guidelines were updated further. [6] In 2022, the AAP released a policy statement on protection of children from sexual abuse by healthcare professionals and within the healthcare setting. [7]
Clinicians who wish to learn more about the specific examination for child sexual abuse can review the article Child Sexual Abuse in Emergency Medicine or the articles on the medical evaluation of sexual abuse listed in the references. [4, 5, 6, 7, 8]
For patient education resources, see the Women's Health Center, as well as Foreign Body, Vagina.
Presentation
History
The following questions are helpful in determining the possible causes of genital redness, itching, discharge, or irritation:
-
Is the child completely toilet-trained? If not, how often does she wear diapers, and what kind of diapers are worn? Ultra-absorbent disposable diapers can hold urine and feces close to the skin for hours without the parent realizing that the diaper should be changed
-
If the child is out of diapers, how is she bathed? Does she take showers or baths? Does she play in a tub with bubble bath or shampoo suds? What kind of soap is used? Does the mother or caregiver scrub the genital area with soap or a washcloth? Bubble bath, shampoo, perfumed soaps, and vigorous scrubbing can cause irritant vulvitis
-
Does the child wear cotton or nylon panties? Does she often wear Lycra clothing or other types of clothing that restrict air circulation to the genital area? Does she like to wear her wet bathing suit all day? Nylon, Lycra, and other occlusive materials can cause genital irritation after prolonged wear
-
Is the child recently toilet-trained? If so, does her mother or other caregiver still help her with hygiene after a bowel movement? If the child cares for her own toilet needs, does her mother or caregiver frequently find streaks of stool on the child's underwear? Fecal soiling can cause irritant vulvitis. Does she wipe front to back?
-
Has the caregiver noticed a bad odor from the genital area or seen dark discharge on the panties? (See Vaginal Discharge)
-
Does the child frequently complain of itching in the genital and anal area, or does the caregiver observe her to be constantly scratching or rubbing herself in that area? (See Vaginal Itching)
-
Does the child have eczema, allergic rhinitis, or diarrhea, or has she had recent upper respiratory infections? These could explain itching, irritation, or discharge
-
Has the caregiver ever noticed the child trying to insert objects into her own vagina? (See Vaginal Discharge)
-
Has the caregiver ever noticed blood on the child's underwear or after wiping? (See Vaginal Bleeding)
-
Does the caregiver have any concerns about possible sexual abuse on the basis of the child's statements or sexualized behaviors? (See Child Sexual Abuse)
Physical examination
To perform a careful genital inspection, the following are necessary:
-
A clinician who has time, knowledge, and skill with children
-
A relaxed or distracted child (books read by the mother or caregiver are great sources of distraction)
-
A good light source
If vaginal discharge is evident upon examination, and the clinician is skilled at sample collection, samples can be obtained by using a small urethral swab (calcium alginate, Dacron, or cotton) moistened with sterile saline. One swab should be sent for routine vaginal culture, and a separate swab for gonorrhea culture can be obtained. A nucleic acid amplification test (NAAT) for both Neisseria gonorrhoeae and Chlamydia trachomatis has been shown to be a much more sensitive method of detecting both gonorrhea and chlamydial infection, using either a urine sample or a sample from a vaginal swab. [9]
NAATs are very sensitive and generally yield a low false-positive rate; however, if the urine NAAT findings are positive for either gonorrhea or chlamydia, the child should be asked to return for a repeat test with a different type of nuclear acid amplification. See the recommendations from the Centers for Disease Control and Prevention. [10]
One position for the patient while the physician is conducting the examination is lying on her back on the examination table in the supine frog-leg position with her knees bent and the soles of her feet touching. The labia majora are then gently spread laterally with separation or grasped and pulled forward toward the examiner with labial traction. In this way, the hymen and vestibular tissues are clearly identified.
If the hymen does not open up with labial traction to reveal the hymenal opening or if vaginal cultures must be taken, the child can be turned over and placed in the prone knee-chest position. In this position, the examiner can take cultures with a urethral swab from the vagina without touching the hymen and causing pain and without the child being alarmed by the sight of the swab.
Normal Variations and Congenital Anomalies
In infants, the hymen is thickened, pale in color, folded upon itself, or redundant. This is due to the effects of maternal estrogen (see the first image below). As the child begins to enter puberty, sometimes before the onset of breast development, estrogen again causes the hymen to become thicker, paler, and folded (see the second image below). In the intervening years, the hymen is usually thinner, more translucent, and pink-red.
 In infants and toddlers, effect of maternal estrogen causes hymen to be thicker and more redundant than in older children. Folds of hymen are often closed, making visualization of hymenal edge difficult.
In infants and toddlers, effect of maternal estrogen causes hymen to be thicker and more redundant than in older children. Folds of hymen are often closed, making visualization of hymenal edge difficult.
 As child begins to enter puberty, her own body produces estrogen, which again causes hymen to become thicker, paler, and more redundant.
As child begins to enter puberty, her own body produces estrogen, which again causes hymen to become thicker, paler, and more redundant.
The 5-year-old girl in the image below has an anular hymen, which means that there is hymenal tissue all the way around the opening into the vagina. Labial traction is being used to expose the structures of the vestibule: the urethral opening, the hymen, and the fossa (the space below the hymen edge). The bright-red color of the vestibular tissues adjacent to the hymen on both sides is readily visible. This is normal vascularity, which should not be mistaken for signs of injury or trauma.
 Red color of vestibular tissues is apparent bilaterally in 5-year-old girl with anular hymen. This is normal vascularity, not to be mistaken for injury or trauma.
Red color of vestibular tissues is apparent bilaterally in 5-year-old girl with anular hymen. This is normal vascularity, not to be mistaken for injury or trauma.
The most common hymenal configuration is the crescentic hymen (see the image below), in which the anterior attachments of the hymen are at the 9- to 11-o'clock or the 1- to 3-o'clock position, with no hymenal tissue anteriorly. The posterior rim of the hymen may appear very narrow in some children, but if no tears or breaks appear in the tissue in the posterior half of the hymen, it is probably normal.
Hymens can also be septate (see the image below). This is an anomaly that may require resection. Adolescents with a septate hymen may find it difficult to remove a tampon, because it pulls on the septation. If the hymenal septum appears very thick, referring the child to a gynecologist to determine whether a septate vagina is also present may be necessary. Alternatively, it can be resected in adolescence.
 Hymenal septum (band of tissue that can stretch either vertically or horizontally across hymenal opening). These septa usually involve only hymen but also can be associated with vaginal septum and other higher-tract congenital abnormalities.
Hymenal septum (band of tissue that can stretch either vertically or horizontally across hymenal opening). These septa usually involve only hymen but also can be associated with vaginal septum and other higher-tract congenital abnormalities.
Two other common variants are the fossa groove in a child who is nearing puberty (see the image below) and the perineal groove, which appears as a mucosal defect extending from the fossa to the anus, usually observed in infants or toddlers. This defect spontaneously heals without treatment, but healing may take several years.
Erythema of Genital Tissues
The skin of the labia majora and labia minora is subject to the same conditions as skin elsewhere on the body. Therefore, childhood eczema, seborrhea, and psoriasis can cause redness, irritation, scaling, and itching in the genital area.
Most often, however, genital redness (with or without vaginal discharge) is caused by local irritants. The most common of these include bubble bath, shampoo, and scented soaps. Bleach used to clean underclothing can also cause irritation, as can strong detergents. Occlusive clothing (eg, nylon panties, leotards and tights, pantyhose, swimsuits, and Lycra shorts or exercise pants) can cause irritant vulvitis in some children.
The standard recommendations for treatment of presumed irritant vulvitis are as follows:
-
Have the child take a sitz bath in plain warm water with no soap of any kind for 20 minutes daily
-
Use only white cotton underwear and white unscented toilet tissue
-
Stop all bubble baths, do not allow the child to play in the tub after shampooing her hair, and do not use shampoo or dishwashing detergent as a bubble bath substitute
-
Use hypoallergenic laundry detergent
-
If proper hygiene is a problem after the child has a bowel movement, have her use a squirt bottle of warm water to rinse afterwards and pat dry with toilet tissue; if marked redness of the genital tissues is present, also involving the perianal area, consider streptococcal cellulitis; a culture can be taken from the affected area, and if test results are positive for group A beta-hemolytic Streptococcus, infection can be treated with penicillin or amoxicillin
-
Consider instructing the child not to sleep in underwear, in that this can decrease vulvar moisture
In a child who is toilet-trained, vulvitis or vaginitis caused by Candida albicans is quite unusual. If the child has the typical thick white vaginal discharge, obtain a culture for fungus. However, most girls in whom a yeast infection is diagnosed probably have irritant vulvitis (see the image below). In patients with vulvar irritation, treatment with an emollient such as Aquaphor or petroleum jelly may also help relieve symptoms.
 Increased genital erythema can be caused by local irritants, infection, or rubbing of tissues. This child had nonspecific vulvovaginitis caused by sensitivity to bubble baths.
Increased genital erythema can be caused by local irritants, infection, or rubbing of tissues. This child had nonspecific vulvovaginitis caused by sensitivity to bubble baths.
Another cause to consider is voiding dysfunction. A report from Chile described 20 girls who were referred for recurrent vulvovaginitis and had urodynamic studies performed. [11] The authors report that 19 of the 20 girls had urodynamia, including 10 with overactive bladder, eight with external bladder sphincter dyssynergia, and one with a hypotonic bladder. Treatment of the dysfunction in 13 of the 20 girls resulted in clinical improvement in symptoms.
In infants and girls who have had repeated episodes of vulvitis, labial adhesions may result from the lack of estrogen effect on the skin of the labia majora; this irritation then leads to a stickiness of the skin, which fuses or adheres. Labial adhesions can be either extensive (see the image below), causing urinary retention, or minor. If the child has no complaints and is able to urinate normally, no treatment is needed. If irritation or recurrent urinary or vaginal infections occur, the adhesions can be treated with topical estrogen cream.
 Labial adhesions can be extensive or minimal. This child was having difficulty urinating because of almost complete adhesion of her labia and needed treatment with topical estrogen cream for 4 weeks.
Labial adhesions can be extensive or minimal. This child was having difficulty urinating because of almost complete adhesion of her labia and needed treatment with topical estrogen cream for 4 weeks.
The cream must be applied directly to the adhesion several times daily for 3-4 weeks. Once the adhesions resolve, daily use of a lubricant, such as petroleum jelly, is necessary to prevent their recurrence (see Labial Adhesions). [12] Surgical separation of the labial adhesions is occasionally necessary for particularly thick and extensive adhesions if they do not respond to estrogen cream.
A retrospective study of 131 girls with labial adhesions compared the success of topical estrogen, topical betamethasone, or combination treatment using both types of topical ointment. [13] The success rates for each of the medications used alone were similar (15%). Combination treatment was slightly more successful at resolving the adhesions (28.5%), but this difference was not statistically significant.
Vaginal Itching
Pinworms can hatch in the anus, travel to the vagina, and cause genital itching. The child may be observed scratching at either the genital or the anal area, especially at night. Occasionally, the parent may be able to see pinworms in the anal area if the child is checked when asleep (see the image below). If genital or perianal itching is particularly intense, a trial of oral medication to eliminate pinworms may be warranted. Parents can also be instructed on how to obtain a sample from the anal area of the child while sleeping, using "pinworm paddles" to try to diagnose the pinworm infestation. When an infestation is confirmed, all family members need to be treated and the bedding cleaned with hot water and bleach.
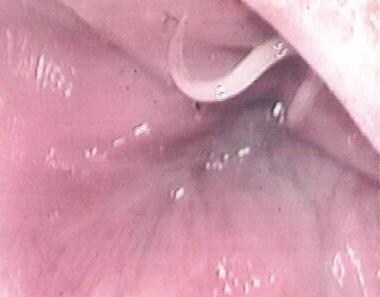 Patient was examined for possible sexual abuse because of constant complaints of pain and itching in genital area. This print from videotaped examination shows pinworm coming out of anus. Image courtesy of Jeanie Ming, CPNP.
Patient was examined for possible sexual abuse because of constant complaints of pain and itching in genital area. This print from videotaped examination shows pinworm coming out of anus. Image courtesy of Jeanie Ming, CPNP.
Irritant vulvitis can also cause itching, and the measures mentioned above usually relieve this symptom.
Another skin condition that can present with intense genital itching is lichen sclerosus. The frequency of this disorder seems to be increasing in prepubertal girls, and it is sometimes difficult to diagnose. The full name of the condition is lichen sclerosus et atrophicus because it eventually causes atrophy of the skin of the affected areas. The skin then becomes easily traumatized and bleeds with normal activities, such as genital wiping, or with rubbing of clothing against the labia.
The characteristic appearance that leads to diagnosis is the sharply demarcated area of hypopigmentation, often in a figure-eight pattern, around the vulva and the perianal area (see the image below). Low-potency topical steroid ointments are often effective in controlling the itching; however, higher-potency formulations used for a shorter time are occasionally necessary (see Lichen Sclerosus et Atrophicus). A study involving both children and adults with lichen sclerosus found that 0.1% tacrolimus ointment was also effective in treating this condition. [14]
Vaginal Discharge
Most cases of vaginal discharge are caused by primary irritants or poor hygiene. Measures recommended above often eliminate the discharge, as well as the genital redness and irritation. Cultures should be obtained if discharge persists, has a foul odor, or is sometimes bloody.
Even in girls with recurrent vaginal discharge, vulvovaginitis is still the most common cause, as was shown in a study of 110 girls referred to a pediatric gynecology clinic for this complaint. [15] In this group, 85% were diagnosed with vulvovaginitis. The other causes included suspected sexual abuse (5%), foreign body (3%), labial adhesions (3%), and vaginal agenesis (2%). In 35% of the cases, the child was admitted for vaginoscopy.
Respiratory pathogens, such as group A beta-hemolytic Streptococcus and Moraxella (Branhamella) catarrhalis, or enteric pathogens, such as Escherichia coli or Shigella organisms, can cause vaginitis with discharge and genital erythema; therefore, it is important to obtain a routine culture from the vagina.
Sexually transmitted organisms can also cause vaginitis in prepubertal girls, even though they cause cervicitis in adolescent and adult women. Cultures should be obtained in a child with a purulent vaginal discharge upon examination to determine the presence of N gonorrhoeae and C trachomatis.
The 2021 guidelines from the Centers for Disease Control and Prevention (CDC) acknowledged that NAATs (eg, ligase chain reaction or polymerase chain reaction [PCR]) can also be done on vaginal swabs or on urine samples from prepubertal girls to detect both organisms. [10] For Chlamydia, NAATs are more sensitive and specific than culture. [16] In many locations, laboratories no longer perform cultures for C trachomatis.
Foreign bodies in the vagina are another relatively common cause of vaginal discharge, especially recurrent discharge with a foul odor or with intermittent bleeding. The most common types of foreign body are small pieces of toilet tissue, which the child usually inserts herself (see the image below).
 Foreign bodies are not unusual in young girls. Most common foreign body is piece of toilet tissue that child inserts herself. Photo shows white piece of tissue, which can usually be removed by gentle irrigation with warm water.
Foreign bodies are not unusual in young girls. Most common foreign body is piece of toilet tissue that child inserts herself. Photo shows white piece of tissue, which can usually be removed by gentle irrigation with warm water.
Small toys, crayons, pen caps, erasers, and other small objects have been removed from young children's vaginas. Most often, these objects are inserted by the child as she explores the vaginal opening in much the same manner as young children who insert objects into their noses or ears. In girls with relatively large hymenal openings, less of a barrier is available to block foreign materials, and bits of tissue may be found inside the vagina from wiping, even if the child has denied inserting anything.
If a child has persistent vaginal discharge, has been treated unsuccessfully with removal of irritants, frequent sitz baths, and mild emollients, and if cultures are negative, an examination by a gynecologist with the patient under anesthesia is indicated. The vagina can be irrigated with saline and explored with the smallest Pedersen speculum or, sometimes, a hysteroscope or cystoscope. Additional cultures can be obtained in this manner, and the vagina can be thoroughly explored for the presence of a small foreign body.
Malignancies such as rhabdomyosarcoma and endodermal sinus tumors can also cause discharge or bleeding and require an intravaginal examination under anesthesia, with biopsy of suspicious lesions. A study of 24 girls younger than 6 years who underwent such an examination for bleeding or discharge identified six patients with malignancies. [17]
Vaginal Bleeding
In addition to foreign bodies, bacterial vaginitis, and lichen sclerosus, other conditions must be considered in the child who presents with blood on the diaper or panties that seems to originate from the vaginal area. [18] (See the image below.)
 This child was brought for urgent care because of blood on her diaper. Appearance of clustered condyloma lesions in vaginal vestibule differs from that of condyloma lesions that develop on skin.
This child was brought for urgent care because of blood on her diaper. Appearance of clustered condyloma lesions in vaginal vestibule differs from that of condyloma lesions that develop on skin.
Condylomata acuminata, or genital warts, often present with bleeding because they are friable and easily abraded. These lesions, caused by human papillomavirus (HPV), can be present in infants as a result of perinatal transmission from the mother's birth canal, even if the mother has no active lesions at the time of delivery. The appearance of the condylomata varies. They can present as large pedunculated lesions (see the image below) or as fleshy hypervascular lesions in mucosal areas such as the vaginal vestibule.
 Presentation of condyloma acuminatum, usually caused by human papillomavirus type 6 or 11, varies. In this case, both mother and father had warts when infant was delivered; thus, virus was likely transmitted at birth.
Presentation of condyloma acuminatum, usually caused by human papillomavirus type 6 or 11, varies. In this case, both mother and father had warts when infant was delivered; thus, virus was likely transmitted at birth.
Another cause of vaginal bleeding is urethral prolapse. The cause of this condition is unknown, and it can occur with no known precipitating factor. It is said to occur sometimes with excessive straining and, for unknown reasons, is much more common in Black girls than in White girls. When the urethra prolapses, it causes discomfort and bleeding. In a case series of 21 Black girls referred for treatment of urethral prolapse, 13 had mild symptoms and were managed conservatively with frequent sitz baths. Seven patients with more severe symptoms underwent prolapse reduction under general anesthesia. None of the patients required surgery. [19]
The first image below shows the appearance of the genital and urethral tissues in a 3-year-old girl who presented with blood in her underwear 1 day after being discharged from the pediatric intensive care unit (ICU) following minor head trauma. She had had a Foley catheter placed and pulled it out (without the balloon being deflated) as she was regaining consciousness. The urethra was prolapsed and showed signs of early necrosis. Surgery was not needed because sitz baths, oral antibiotic therapy, and application of topical estrogen cream led to the resolution of the problem within 7 days (see the second image below).
 3-year-old girl presented with blood in panties 2 days after being discharged from intensive care unit after treatment for injuries resulting from fall from playground slide. When she awoke from sedation, she had pulled out her Foley catheter. No bleeding was noted at that time, but bleeding started after she went home. Urethra is prolapsed and engorged and shows evidence of early necrosis.
3-year-old girl presented with blood in panties 2 days after being discharged from intensive care unit after treatment for injuries resulting from fall from playground slide. When she awoke from sedation, she had pulled out her Foley catheter. No bleeding was noted at that time, but bleeding started after she went home. Urethra is prolapsed and engorged and shows evidence of early necrosis.
 Photo shows resolution of prolapse experienced by child in preceding image. Child was treated with local hygiene measures, oral antibiotics, and topical estrogen cream to promote healing. Hymen can be seen inferiorly and is normal in appearance.
Photo shows resolution of prolapse experienced by child in preceding image. Child was treated with local hygiene measures, oral antibiotics, and topical estrogen cream to promote healing. Hymen can be seen inferiorly and is normal in appearance.
When a child presents with a history of blood in the diaper or on the panties, the examination should be performed on an urgent basis. If trauma to the genital or anal tissues has occurred, the possibility of sexual abuse must always be considered. Acute lacerations of the posterior fourchette, hymen, or anus are readily seen by even an inexperienced examiner. The image below shows a laceration of the posterior fourchette and a complete tear through the hymen in a 9-year-old girl who was raped by her stepfather and bled for 5 days.
 Photo shows injuries to 9-year-old girl who was raped. She has tear through hymen, posterior fourchette, and vagina, with bruising of tissues as well.
Photo shows injuries to 9-year-old girl who was raped. She has tear through hymen, posterior fourchette, and vagina, with bruising of tissues as well.
When children have injuries such as these, even if the history of sexual assault is not forthcoming, the child must be referred to the closest center where forensic medical examinations of children are conducted. Trace evidence must be collected and preserved for law enforcement, and injuries must be carefully documented, preferably with photographs.
Accidental injuries to the genital and anal tissues also occur in children. In these cases, the child is usually brought for care immediately when the parent notices blood on the underclothes or the child complains of pain and is able to describe what caused her injury. Bruising of the external genital tissues may be present or absent, depending on the type of accident.
One case report described injury to the hymen resulting from accidental impalement by a "Barbie's horse's foot" in a 7-year-old girl who was sliding bottom-first in the wet tub trying to knock down her toy horses after her bath. Another case report described two girls with injuries to the hymen after being run over by slow-moving automobiles. Another report from 1999 described two girls who sustained midline splitting injuries of the fossa navicularis and posterior fourchette from "doing the splits" while skating on inline skates. [20]
The image below depicts a bruise near the hymen of an 8-year-old girl that was caused by falling on a rock while climbing up a steep hill. Her older brother was above her and also slid down, landing on her. She and her brother confirmed the history.
The images below show a 5-year-old girl who was brought to the emergency department after her mother noticed she was still bleeding 3 days after falling on the edge of a cabinet door in the bathroom. The child told her mother she was standing on the shelf of the cabinet under the bathroom sink when she slipped and landed on the top of the open cabinet door. The first image below shows the bruise on her labia majora. The second image is a close-up view, taken with a camera attached to a colposcope, of the laceration of the fossa navicularis and bruising on the lower portion of her hymen.
 Magnified view of fossa navicularis and lower hymen edge of child shown in preceding image. Laceration of fossa is visible, along with bruising on hymen.
Magnified view of fossa navicularis and lower hymen edge of child shown in preceding image. Laceration of fossa is visible, along with bruising on hymen.
In another case, a 3-year-old girl was brought in after she fell off a trampoline and landed on the hard edge of an upside-down plastic crate that was being used as a step. She had a laceration between the right labium minus and the right labium majus (see the image below). Her older brother confirmed the history. Although he did not see the fall, he heard her cry and found her lying next to the crate.
 Laceration between labium minus and labium majus on right side. Child fell while jumping on trampoline, landing on hard plastic crate.
Laceration between labium minus and labium majus on right side. Child fell while jumping on trampoline, landing on hard plastic crate.
Rarely, girls with no signs of puberty may develop a condition known as isolated prepubertal menarche. In such cases, the child has no signs of sexual development but experiences monthly episodes of vaginal bleeding or spotting. If physical examination, ultrasonography, examination under anesthesia, and laboratory studies all yield normal results, the child can be monitored carefully for other signs of premature puberty, and the parents can be reassured. [21]
Genital Pain
Young girls with urinary tract infections, vaginal infections, vaginal irritation, vulvar skin conditions, or other skin lesions may complain of pain in the genital area. [22] If inspection reveals the presence of genital ulcers, the following conditions should be considered in the differential diagnosis:
-
Primary varicella or varicella zoster lesions
-
Ulcerative vulvitis of bacterial origin
-
Bacterial infection (especially Streptococcus) [23]
Because only herpes simplex and syphilis raise the suspicion of sexual abuse, the vesicular lesions should be cultured for virus and serum obtained for syphilis serology if the child gives no history of sexual contact before any report is made to protective services. A routine bacterial culture should be obtained, and the oral mucosa, eyes, and perianal area should be carefully examined for other signs of systemic illness.
The image below shows vesicular lesions on the labia of a 6-year-old girl who described being sexually abused. One lesion was swabbed and sent for viral culture, and herpes simplex type 2 was identified.
 These vesicular lesions on labia majora were cultured and found to be caused by herpes simplex type 2. Child also gave history of being sexually abused.
These vesicular lesions on labia majora were cultured and found to be caused by herpes simplex type 2. Child also gave history of being sexually abused.
The adolescent girl in the image below presented with a painful genital ulcer, which was cultured for herpes. Her case was reported to child protective services as probable abuse, even though she denied any type of sexual contact. The culture of the lesion subsequently was negative for herpes. A bacterial culture revealed E coli, and the lesion resolved with improved hygiene and oral antibiotics. This child had no oral lesions at the time but several months later developed another genital ulcer along with an oral ulcer; she was thought to have Behçet disease.
-
In infants and toddlers, effect of maternal estrogen causes hymen to be thicker and more redundant than in older children. Folds of hymen are often closed, making visualization of hymenal edge difficult.
-
Red color of vestibular tissues is apparent bilaterally in 5-year-old girl with anular hymen. This is normal vascularity, not to be mistaken for injury or trauma.
-
As child begins to enter puberty, her own body produces estrogen, which again causes hymen to become thicker, paler, and more redundant.
-
Crescentic hymen, which is smooth and without interruption, in 7-year-old girl.
-
Hymenal septum (band of tissue that can stretch either vertically or horizontally across hymenal opening). These septa usually involve only hymen but also can be associated with vaginal septum and other higher-tract congenital abnormalities.
-
In adolescent girls or in those just entering puberty, hymen becomes thicker and more redundant. Concurrently, groove may appear in fossa navicularis. This is normal developmental feature. Image courtesy of Nancy Kellogg, MD.
-
Increased genital erythema can be caused by local irritants, infection, or rubbing of tissues. This child had nonspecific vulvovaginitis caused by sensitivity to bubble baths.
-
Labial adhesions can be extensive or minimal. This child was having difficulty urinating because of almost complete adhesion of her labia and needed treatment with topical estrogen cream for 4 weeks.
-
Patient was examined for possible sexual abuse because of constant complaints of pain and itching in genital area. This print from videotaped examination shows pinworm coming out of anus. Image courtesy of Jeanie Ming, CPNP.
-
This 8-year-old girl complained of genital itching and had spots of blood on her underpants. Pattern of hypopigmentation, with clear demarcation of normal and affected skin, is typical of lichen sclerosus. Atrophic skin bleeds easily, even with gentle wiping with tissue.
-
Foreign bodies are not unusual in young girls. Most common foreign body is piece of toilet tissue that child inserts herself. Photo shows white piece of tissue, which can usually be removed by gentle irrigation with warm water.
-
Presentation of condyloma acuminatum, usually caused by human papillomavirus type 6 or 11, varies. In this case, both mother and father had warts when infant was delivered; thus, virus was likely transmitted at birth.
-
3-year-old girl presented with blood in panties 2 days after being discharged from intensive care unit after treatment for injuries resulting from fall from playground slide. When she awoke from sedation, she had pulled out her Foley catheter. No bleeding was noted at that time, but bleeding started after she went home. Urethra is prolapsed and engorged and shows evidence of early necrosis.
-
Photo shows resolution of prolapse experienced by child in preceding image. Child was treated with local hygiene measures, oral antibiotics, and topical estrogen cream to promote healing. Hymen can be seen inferiorly and is normal in appearance.
-
Photo shows injuries to 9-year-old girl who was raped. She has tear through hymen, posterior fourchette, and vagina, with bruising of tissues as well.
-
Bruise in vaginal vestibule caused by landing on rock while climbing steep hill.
-
Labial bruise in 5-year-old girl who fell on edge of cabinet door.
-
Magnified view of fossa navicularis and lower hymen edge of child shown in preceding image. Laceration of fossa is visible, along with bruising on hymen.
-
Laceration between labium minus and labium majus on right side. Child fell while jumping on trampoline, landing on hard plastic crate.
-
These vesicular lesions on labia majora were cultured and found to be caused by herpes simplex type 2. Child also gave history of being sexually abused.
-
13-year-old girl presented with complaint of painful ulcer. Cultures for herpes virus were negative, as was serologic testing for syphilis. Lesion resolved with improved hygiene and oral antibiotics and was presumed to be caused by bacterial infection of scratch on labia.
-
This child was brought for urgent care because of blood on her diaper. Appearance of clustered condyloma lesions in vaginal vestibule differs from that of condyloma lesions that develop on skin.












