Background
Anomalous congenital connections of the pulmonary venous system represent a spectrum of conditions in which the pulmonary veins are partially or entirely connected to the right atrium, either directly or via the systemic venous return. Anomalous connection rather than “drainage” or “return” better describes the anatomical situation.
Total anomalous pulmonary venous connection (TAPVC) and partial anomalous pulmonary venous connection (PAPVC) account for 1-2% of congenital heart defects.
History of the Procedure
Wilson first described the analogy in 1798, which Brody reviewed in 1942 (37 cases in the literature). Muller performed the first surgical intervention in 1951, and the condition was first completely corrected with the use of cardiopulmonary bypass in 1956-1957.
Since then, various modifications of the technique have been proposed. For instance, free and in situ autologous tissue have been used to create a wide, unobstructed connection between the pulmonary venous confluence and the left atrium (LA). Despite this technique, 10-15% of patients represent with stenosis after initial successful correction. Recurrent stenosis is often a progressive process, resulting in multiple representations requiring further procedures for correction, with an increasingly poor outcome at each representation.
Most recently, a technique to minimize the surgical trauma to the pulmonary vein intima was proposed to improve outcomes in patients with postrepair stenosis. At present, indications for using this technique are being extended to the correction of primary venous anomalies.
Problem
In the absence of a normal connection, an alternative pathway is formed to allow the egress of blood from the developing lung. This connection is usually to the right atrium (RA), or a systemic vein draining into the RA, thus creating a left-to-right shunt.
Patients with partial anomalous pulmonary venous connection (PAPVC) most commonly have an associated sinus venosus type atrial septal defect (ASD); PAPVC with intact atrial septum is a rare finding. Pisola et al describe a case of PAPVC with connection between the left upper pulmonary vein and the left internal thoracic vein with an intact atrial septum. [1]
Patients with total anomalous pulmonary venous connection (TAPVC) most commonly present a confluence draining into a connecting vein to the systemic venous system. Less commonly, the pulmonary veins may drain to multiple sites (mixed pulmonary venous connection). Supply of oxygenated blood to the systemic circulation relies on an intracardiac right to left shunt in these patients.
Etiology
The primitive lungs buds out-pouch from the foregut at 26-27 days' gestation. Shortly after a venous splanchnic plexus develops around them and allows the drainage of blood into the anterior cardinal (the later vena cava, coronary sinus, and azygous vein) and into the umbilicovitelline (ie, portal system) systems. Around day 27, the primordial pulmonary vein arises behind the developing atrium and fuses with the splanchnic plexus, around day 30. The portion of the atrium to the left of the developing septum primum then fuses with the pulmonary venous confluence positioned behind it as a result of the reabsorption of the primordial vein. By day 38-40, the reabsorption is complete and 4 distinct pulmonary vein ostia are found on the posterior wall of the fully formed left atrium. At the same time, the connections between the lung buds and the systemic venous system regress.
Total anomalous pulmonary venous connection (TAPVC) is thought to result from failure of fusion between the LA evagination and the pulmonary venous plexus or from a position mismatch between the atrial evagination and the forming atrial septum. Partial anomalous pulmonary venous connection (PAPVC) occurs at the same stage but does not involve all four veins.
Anomalies occurring at a later stage and in particular during the reabsorption of the primordial vein are at the origin of related lesions like cor triatriatum and atresia of pulmonary vein. Anomalies in the modality of formation and involution of the primordial pulmonary vein are responsible for rarer conditions like congenital pulmonary vein stenosis and an abnormal number of pulmonary veins. [2, 3]
Pathophysiology
Partial anomalous pulmonary venous connection
The main hemodynamic abnormality is represented by the left-to-right shunt imposed by pulmonary venous drainage into the RA. The presence of an interatrial communication further increases the left to right shunt because as much as 50% of the total venous return to the left atrium can shunt to the right side. The resulting volume overload leads to chronic dilatation of the right ventricle, hypertrophy, and, eventually, supraventricular arrhythmias and systolic dysfunction.
Although an atrial septal defect (ASD) usually produces a left-to-right shunt, it adds the potential for right-to-left shunting at a later stage when pulmonary hypertension and right ventricular diastolic dysfunction ensue.
Total anomalous pulmonary venous connection
The hemodynamic abnormality in patients with TAPVC is related to the complete diversion of pulmonary venous blood away from the left atrium to a systemic vein. As a consequence, two anatomic factors determine the patient's clinical status.
An obstruction may occur in the path of the pulmonary venous drainage from the lungs to the systemic venous system. If obstruction occurs, egress of blood from the lungs is limited. The consequences of obstruction are pulmonary venous congestion, pulmonary hypertension with consequent limitation of pulmonary blood flow, increased right atrial pressures, hypoxia, and low cardiac output. These events lead to life-threatening cyanosis and shock immediately after birth. [4]
Desaturated blood cannot reach the left ventricle unless a right-to-left shunt is present. In most cases, this is a patent foramen ovale (PFO), ASD, or, more uncommonly, a patent ductus arteriosus (PDA) or ventricular septal defect (VSD). The obligated right-to-left shunt determines systemic cardiac output and oxygenation.
Presentation
Partial anomalous pulmonary venous connection
Patients are often asymptomatic and present with a murmur as an incidental finding upon routine examination. Older patients may present with primary arrhythmia, most commonly atrial fibrillation.
Subsequent workup demonstrates PAPVC and an associated sinus venosus atrial septal defect (ASD). Symptomatic patients present with the sequelae of a large left-to-right shunt: decreased exercise tolerance and/or poor growth. Upon examination, cyanosis is rarely seen unless pulmonary hypertension has developed. A fixed-split and prominent second heart sound and a functional systolic murmur at the left parasternal upper auscultation point are often present. [5]
Total anomalous pulmonary venous connection
The degree of pulmonary venous obstruction largely determines the clinical presentation. Patients with high-grade obstruction present perinatally with profound cyanosis and shock, or with cyanosis, respiratory distress, and poor growth in mildly stenosed circulation. Upon examination, tachypnea, cyanosis, and poor peripheral perfusion are invariably seen. The second heart sound is prominent and split as a result of pulmonary arterial hypertension. Unless rapid resuscitation measures including intubation and early surgical repair are put in place, death is the likely outcome in these cases.
In contrast, patients without clinically significant pulmonary venous obstruction present in infancy or early childhood with signs and symptoms related to a large left-to-right shunt and resulting right-heart volume overload. They still can present with dyspnea, poor feeding, and poor growth. They may have cyanosis on examination, but this is usually mild.
Indications
Obstruction in the pulmonary venous pathway constitutes a surgical emergency in patients with total anomalous pulmonary venous connection (TAPVC). Medical measures aim at resuscitating and optimizing the patient's clinical status until definitive repair and include intubation, hyperventilation with 100% oxygen, prostaglandin infusion, aggressive correction of pH, correction of all metabolic dysfunction, and inotropic support. The definitive therapeutic goal is complete relief of pulmonary venous obstruction and correction of the anomalous correction, which can be accomplished with only surgical repair.
In the absence of obstruction, surgery can be performed on an elective basis after diagnosis. Excellent clinical results are reported in infants, suggesting that little is gained by delaying surgical repair beyond age 4-6 months.
Relevant Anatomy
Partial anomalous pulmonary venous connection (PAPVC) is characterized by the failure of 1-3 pulmonary veins to incorporate within the developing left atrium (LA). Typically, the right upper pulmonary vein (RUPV) is affected and connects to the superior vena cava (SVC), most commonly at the SVC–right arterial (RA) junction (see the image below).
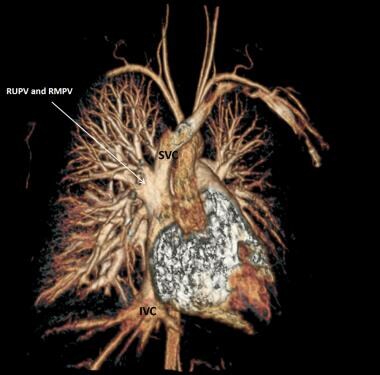 Partial anomalous pulmonary venous connection (PAPVC) of right-sided pulmonary veins to the right superior venoatrial junction. Note the enlarged confluence and superior vena cava. SVC = Superior vena cava; IVC = Inferior vena cava; RUPV = Right upper pulmonary vein; RMPV = Right middle pulmonary vein.
Partial anomalous pulmonary venous connection (PAPVC) of right-sided pulmonary veins to the right superior venoatrial junction. Note the enlarged confluence and superior vena cava. SVC = Superior vena cava; IVC = Inferior vena cava; RUPV = Right upper pulmonary vein; RMPV = Right middle pulmonary vein.
More infrequently, the junction is at higher levels above the inlet of the azygos vein. Occasionally, the connection is found at the SVC-innominate vein junction. Less frequently, the lower pulmonary vein connects to the inferior vena cava (IVC)–RA junction. In some rare instances, both veins connect to the right atrial wall. [6, 7]
This lesion commonly occurs in association with sinus venosus atrial septal defect (ASD), which can be found above the superior limbus or below the fossa ovalis (beneath the Valsalva valve). Intact atrial septum is rare. [1, 8]
A more serious condition albeit rare is the scimitar syndrome, where the whole of the right lung veins drain into the IVC via a long vein descending parallel to the right-heart border (see the image below).
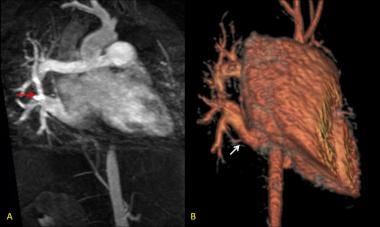 (A): Patient with obstructed scimitar syndrome (magnetic resonance angiography). The right upper pulmonary vein (RUPV) is diffusely narrow and presents a discrete stenosis at the confluence with the right lower pulmonary vein (red arrow). (B): The confluence at the atrial level appears unobstructed (white arrow) in the 3D reconstruction.
(A): Patient with obstructed scimitar syndrome (magnetic resonance angiography). The right upper pulmonary vein (RUPV) is diffusely narrow and presents a discrete stenosis at the confluence with the right lower pulmonary vein (red arrow). (B): The confluence at the atrial level appears unobstructed (white arrow) in the 3D reconstruction.
The radiographic appearance of an enhanced vertical profile, resembling the blade of a scimitar sword is the diagnostic finding in these cases. This condition is commonly associated with right lung hypoplasia, aortopulmonary collaterals to the right lung, pulmonary venous obstruction, and pulmonary hypertension. [9]
In patients with total anomalous pulmonary venous connection (TAPVC) lungs drain to the systemic venous system, creating a large left-to-right shunt. Supply of oxygenated blood to the systemic circulation requires an intracardiac communication. This communication is usually an ASD, less commonly a patent ductus arteriosus (PDA), or ventricular septal defect (VSD). Any obstruction at the level of the confluence, communicating vein, or the intracardiac shunt results in decreased left side blood inflow, pulmonary venous congestion, and consequent pulmonary hypertension. [10]
TAPVC represent a wide array of venous configurations. A unified nomenclature system has been presented at the International Nomenclature and Database Conferences for Pediatric Cardiac Surgery. [11] In this system, the original Darling's classification has been adopted because of its simplicity and wide acceptance, but the presence or absence of obstruction has been added, as well as the nature and level of obstruction. Four types are therefore identified, all of which can present with or without obstruction (see the image below).
The supracardiac type accounts for 45-55% of cases (see the image below).
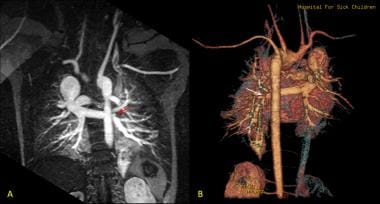 (A): Total anomalous pulmonary venous connection (TAPVC) of supracardiac type. All pulmonary veins drain into a long confluence and a short communicating vein is attached to the right superior vena cava (SVC). The left lower pulmonary vein appears stenosed (red arrow). (B): These findings are confirmed by the 3D reconstruction (white arrow).
(A): Total anomalous pulmonary venous connection (TAPVC) of supracardiac type. All pulmonary veins drain into a long confluence and a short communicating vein is attached to the right superior vena cava (SVC). The left lower pulmonary vein appears stenosed (red arrow). (B): These findings are confirmed by the 3D reconstruction (white arrow).
All four veins connect to a confluence positioned behind the left atrium, from which a communicating vein (vertical vein) ascends inside or outside the pericardial cavity to connect with the systemic venous system. The innominate vein, the right sided SVC or a persistent left-SVC represent the usual sites of insertion. Obstruction in this type is uncommon. When present, obstruction can result from a so-called anatomical vice where the connecting vein is compressed between the left pulmonary artery and the left bronchus. Given the restriction to the egress of blood from the lungs, pulmonary arterial pressure rises, causing further distension of the pulmonary artery, thus promoting a vicious cycle of distension-obstruction.
In the cardiac group (15-20% of cases), the pulmonary venous confluence connects to the coronary sinus. This can be direct or by interposition of a short connecting vein. The coronary sinus is invariably enlarged, and in some cases is unroofed. Rarely the confluence drains directly to the right atrium. Obstruction in this type is uncommon, but stenosis of the short connecting vein to the coronary sinus has been reported.
Infracardiac types account for 15-20% of cases. Most commonly a vertical vein lying posteriorly to the pericardium connects the pulmonary vein confluence with the portal veins, or the ductus venosus, after traversing the diaphragm through the oesophageal hiatus. Blood then enters the right atrium via the inferior vena cava (IVC). The course of the connecting vein is often long and tortuous, resulting in a high incidence of obstruction which can result from external compression or be of intrinsic nature.
In the mixed type (5-10%), pulmonary venous drainage occurs with a combination of supracardiac, cardiac, and/or infracardiac connections.
Shunts at an atrial level are typically of adequate size and the interatrial gradient is usually low. Restrictive flow across the intracardiac communication is uncommonly the cause of obstruction but when present produces a severe compromise of systemic cardiac output. Moreover, any restriction at the level of the ASD, reducing the volume of blood able to cross to the left heart, causes elevation of the RA pressure and functional obstruction of the pulmonary venous return. [12]
The LA is generally half the size of the expected normal, due to a small posterior component. In most cases the left ventricle has normal size and muscular mass. On the contrary, the right ventricle can be enlarged and hypertrophied, especially in supradiaphragmatic, nonobstructive lesions. [13]
As many as 90% of patients with heterotaxy and asplenia have TAPVC. Tetralogy of Fallot, double outlet right ventricle, and interrupted aortic arch have also been reported as associated lesions [14, 15] .
Contraindications
Total anomalous pulmonary venous connection
No specific contraindications are noted for the repair of total anomalous pulmonary venous connection (TAPVC), although the surgical risk may be high in select groups of patients (eg, single ventricle, or heterotaxy syndromes).
Partial anomalous pulmonary venous drainage
In patients with partial anomalous pulmonary venous drainage (PAPVC) and an atrial septal defect (ASD), closure of the ASD may be inappropriate when pulmonary artery pressures are greater than two thirds the systemic pressure. Although rare, the presence of irreversible pulmonary hypertension is associated with systemic cyanosis. The surgical risk in this group of patients may be prohibitive.
-
Types of total anomalous pulmonary venous connection.
-
Partial anomalous pulmonary venous connection (PAPVC) of right-sided pulmonary veins to the right superior venoatrial junction. Note the enlarged confluence and superior vena cava. SVC = Superior vena cava; IVC = Inferior vena cava; RUPV = Right upper pulmonary vein; RMPV = Right middle pulmonary vein.
-
(A): Patient with obstructed scimitar syndrome (magnetic resonance angiography). The right upper pulmonary vein (RUPV) is diffusely narrow and presents a discrete stenosis at the confluence with the right lower pulmonary vein (red arrow). (B): The confluence at the atrial level appears unobstructed (white arrow) in the 3D reconstruction.
-
(A): Total anomalous pulmonary venous connection (TAPVC) of supracardiac type. All pulmonary veins drain into a long confluence and a short communicating vein is attached to the right superior vena cava (SVC). The left lower pulmonary vein appears stenosed (red arrow). (B): These findings are confirmed by the 3D reconstruction (white arrow).
-
Follow-up CT scan performed after repair of total anomalous pulmonary venous connection (TAPVC). The right upper pulmonary vein (RUPV) appears severely stenosed (red arrow).








