Background
The term "multiple births" refers to the delivery of twins and higher-order multiples (ie, triplets, quadruplets, etc). Multiple births occur when multiple fetuses are carried during a pregnancy with the subsequent delivery of multiple neonates. Pregnancies complicated by multiple births are associated with a higher rate of neonatal morbidity and mortality, paralleling the increased risk of preterm delivery, low birth weight, and other associated high-risk morbidities. [1] Maternal morbidity and mortality are also increased in pregnancies complicated by multiple gestations and multiple births.
Physiology/Pathophysiology
Placental physiology has a significant impact on fetal and neonatal outcome. Monochorionic twins have increased neonatal morbidities such as prematurity, intrauterine growth retardation, congenital anomalies, twin-to-twin transfusion syndrome, and increased perinatal mortality. [2] Twin-to-twin transfusion syndrome has been reported in 8-10% of monochorionic pregnancies. Triplet gestations with monochorionic placentation may also experience an increased complication rate. [1, 3]
Determination of placental chorionicity can be evaluated by obstetric ultrasonography during the first and early second trimester. Evaluation of the placenta(s) after birth may also be helpful in the perinatal evaluation process.
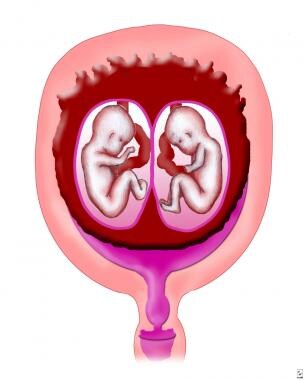
Monozygotic pregnancies involve the fertilization of a single ovum by a single sperm. Monozygotic twins develop when a single fertilized ovum splits after conception. An early splitting of the ovum (ie, within 2 days of fertilization) produces separate chorions and amnions. These dichorionic twins have different placentas, which can be separate or fused. Approximately 30% of monozygotic twins have dichorionic/diamniotic placentas.
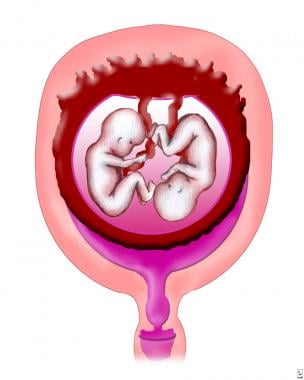
Later splitting (ie, 3-8 days after fertilization) results in monochorionic/diamniotic placentation (see the image below).
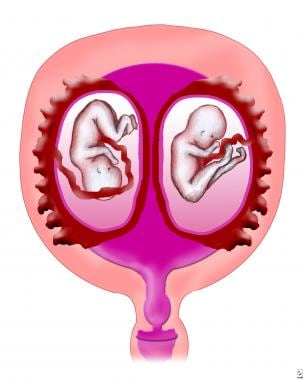
Approximately 70% of monozygotic twins are monochorionic/diamniotic. If splitting occurs later (ie, 9-12 days after fertilization), monochorionic/monoamniotic placentation occurs (see the image below).
Monochorionic/monoamniotic twins are rare; only 1% of monozygotic twins have this form of placentation. Monochorionic/monoamniotic twins have a common placenta, with the possibility of significant vascular communication between the 2 fetal circulations. These twins can develop twin-to-twin transfusion syndrome. If twinning occurs more than 12 days after fertilization, then the monozygotic fertilized ovum only partially splits, resulting in conjoined twins.
Dizygotic, trizygotic, and other higher-order pregnancies involve the fertilization of multiple ova. Dizygotic twins, for example, develop when two ova are fertilized. Dizygotic twins have separate amnions, chorions, and placentas (see the image below).
The placentas in dizygotic twins may fuse if the implantation sites are proximate. The fused placentas can be easily separated after birth.
Triplet pregnancies result from various fertilization, splitting, and development scenarios that involve ova and sperm. For example, triplets can be monozygotic, dizygotic, or trizygotic. Trizygotic triplets occur when three sperm fertilize three ova. Dizygotic triplets develop from one set of monozygotic cotriplets and a third cotriplet derived from a different zygote. Finally, two consecutive zygotic splittings with a vanished fetus can also result in monozygotic triplets. Zygosity in quadruplets and higher order multiples also varies.
Although the evaluation of the placenta(s) following birth is important in all multifetal pregnancies, the examination may not always help to determine zygosity. [4]
Epidemiology
The incidence of monozygotic twins is constant worldwide, approximately 4 per 1000 births. Approximately two thirds of twins are dizygotic. Birthrates of dizygotic twins vary by race (10-40 per 1000 births in blacks, 7-10 per 1000 births in whites, and approximately 3 per 1000 births in Asians) and maternal age (ie, the frequency has risen with increasing maternal age ≤40 years). Dizygotic-twin birthrates are also influenced by other factors, such as parity and mode of fertilization (ie, most artificially conceived twins are dizygotic; however, 6-10% are monozygotic). The highest birthrate of dizygotic twins occurs in African nations, and the lowest occurs in Asia. [5, 6] The incidence of multiple zygotic pregnancies varies in relation to maternal age, the use of assisted reproductive technology (ART), and ethnicity. Naturally occurring triplet births occur in approximately 1 per 7000-10,000 births; naturally occurring quadruplet births occur in approximately 1 per 600,000 births.
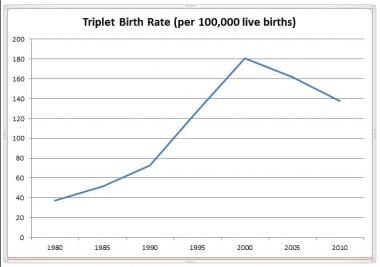
The incidence of multiple births increased significantly in the late 20th century in the United States and worldwide. [2, 7] A combination of factors contributed to this, the two most prominent of these being the use of ART and advanced maternal age at the time of conception. [2, 8, 9, 10]
In the United States, a plateau in the prevalence of multiple births was observed from 2004-2010. Statistics showed that the prevalence of twin deliveries in the United States remained stable at approximately 33 per 1000 live births, compared with a decreasing prevalence of higher-order multiple deliveries (see the graphs below). [2, 10] This trend continued until 2014, when the twin birth rate began to decline by an average of 1% a year from 33.9 in 2014 to 32.6 in 2018, for a total decrease of 4%. [11, 12, 13]
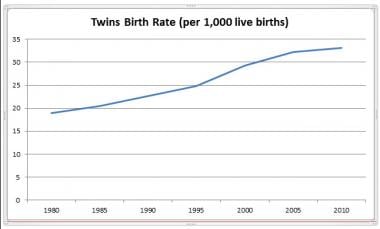 National Vital Statistics Reports, August 2012. Courtesy of the US Department of Health and Human Services (HHS).
National Vital Statistics Reports, August 2012. Courtesy of the US Department of Health and Human Services (HHS).
Prognosis
Even with advancements in perinatal/neonatal medicine, multifetus pregnancies present challenges in prenatal and postnatal care. Neonatal morbidity and mortality parallel the increased risk of preterm birth and low birth weight in these pregnancies. [14]
Improving the outcome of multifetal pregnancies involves decreasing the rate of preterm births, providing an optimal intrauterine environment for fetal growth, optimizing neonatal care in the delivery room, and neonatal ICU if required. [15]
Maternal morbidity
Multiple-gestation pregnancies are associated with a significantly higher maternal complication rate than are singleton gestations. [16] Multiple-gestation pregnancies carry an increased risk of hypertensive disorders of pregnancy; gestational diabetes mellitus; hyperemesis; preterm labor; premature rupture of membranes; anemia; placental abruption; postpartum hemorrhage; cardiac complications, such as myocardial infarction and left ventricular heart failure; operative deliveries, both vaginal and cesarean; required hysterectomy; and prolonged hospital stay. [2, 16]
Fetal/neonatal morbidity
The increase in fetal and neonatal morbidity and mortality associated with multiple-gestation/birth pregnancies correlates with an increased risk of preterm delivery, low birth weight, and intrauterine growth retardation. The neonatal mortality rate in multiple-fetus pregnancies is similar to singleton rates, increasing with decreasing gestational age.
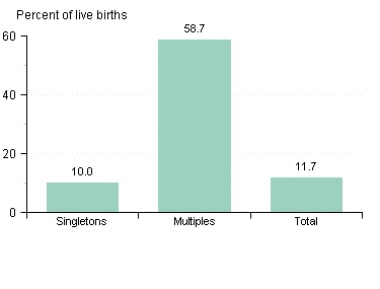
The average gestational age for twin deliveries is 35.3 weeks; for triplet deliveries, 32.2 weeks; and for quadruplet deliveries, 29.9 weeks. Although the percentage of preterm multiple-birth deliveries in the United States declined between 2006 and 2010 (as did the incidence of preterm births in general), [10] the rate still remained significantly high; in 2011, approximately 60% of multiples delivered at less than 37 weeks' gestation (see the graph below). [2, 17]
Birth weight is closely associated with gestational age, so the increased incidence of preterm delivery influences the rate of reduced birth weights in multiple-birth neonates. These neonates also have an increased incidence of intrauterine growth retardation. Divergence from singleton growth curves occurs at approximately 32-33 weeks in twin gestations, at 29-30 weeks in triplet gestations, and at 27-28 weeks in quadruplet gestations.
Comparing specific morbidities and mortality in multiple-gestation pregnancies is difficult due to the complexity of contributing factors. For example, some evidence suggests a link between ART and perinatal morbidity unrelated to the risks associated with multiple births. [18] Chorionic-amniotic placentation also affects multiple-gestation outcomes.
Neonatal outcomes at specific gestational ages and birth weights are similar in multiple-birth neonates to those in singleton pregnancies. Neonates from multiple-gestation pregnancies may have a higher risk of acute respiratory morbidity, such as respiratory distress syndrome, [19] but do not have a higher incidence of chronic lung disease. Other major morbidities, including intraventricular hemorrhage, periventricular leukomalacia, retinopathy of prematurity, necrotizing enterocolitis, patent ductus arteriosus, and nosocomial infection, as well as length of hospital stay, demonstrate no statistical difference between singletons and multiples. [8, 20]
The risk of cerebral palsy in multiple-fetus pregnancies parallels decreasing gestational age. A second association during the late preterm period (34-37 weeks' gestation) may correlate with the increasing maternal morbidities of multiple-fetus pregnancies during this time frame (ie, fetal growth restriction, hypertensive disorders, placental insufficiency). [9]
In a prospective cohort study of monochorionic twins followed from the first trimester to a mean age of 24 months, Ortibus et al found that twin-to-twin transfusion syndrome (a specific morbidity in multiple-gestation pregnancies) and assisted conception increased the risk of both death and neurodevelopmental impairment, whereas early onset discordant growth increased only the risk of death. Of the 136 pregnancies studied, 90% resulted in both twins surviving, 4% resulted in one survivor, and 6% resulted in no survivors. Overall mortality was 8%, and neurodevelopmental impairment occurred in 10% of infants. [21]
Patient Education
When multifetal pregnancy is diagnosed, parental education on specific issues of a multifetal pregnancy should take place.
Most outcomes from multifetal pregnancies require only routine pediatric care; however, some patients may require specialized follow-up coordinated through a neonatal ICU (NICU) follow-up clinic.
-
Monochorionic/diamniotic placentation.
-
Dichorionic/diamniotic placentation.
-
Monochorionic/monoamniotic placentation.
-
National Vital Statistics Reports, August 2012. Courtesy of the US Department of Health and Human Services (HHS).
-
National Vital Statistics Reports, August 2012. Courtesy of the US Department of Health and Human Services (HHS).
-
Preterm by plurality, United States, 2011. Courtesy of March of Dimes (www.marchofdimes.org).