Overview
Approximately 1.96 million new cases of invasive cancers are diagnosed annually in the United States. Cancer is the second leading cause of death in the United States among children aged 1 to 14 years, and there are an estimated 9910 cases annually in this age group. [1] The heterogeneity of pediatric cancer is substantial, and even the most common pediatric cancer (ie, acute lymphoblastic leukemia [ALL]) is characterized by biological and clinical diversity. As a result of this heterogeneity and low incidence, the ability of epidemiologists to ascribe causes to specific childhood cancers is extremely limited.
Epidemiological studies have noted the effects of cancer genetics, defined family pedigrees and penetrance, and identified subsets of certain cancers and their implications for treatment and prognosis. In addition, the study of rare genetic diseases that increase the risk of malignancy in childhood has led to an understanding of important cancer genes, which has wide applicability to oncology in both children and adults.
Tools of Study
Measures The understanding of the epidemiology of any medical problem demands the use of basic terminology from the language of statistics. Important terms are defined as follows:
Ratio - Relationship between 2 quantities (ie, x/y)
Proportion - Ratio in which the denominator also includes the numerator (ie, x/[y + x])
Rate - Proportion occurring per time period (ie, x/[x + y]/time)
Incidence - Proportion of new cases within a population over time (ie, x/[y + x]/time)
Prevalence - Number of existing cases in a population at a set time
Crude rate - Measure of actual events in a population
Standardized rate - Crude rate adjusted for a factor in the population (eg, age, sex, economic status)
Standardized mortality-incidence ratios - Observed rates adjusted by comparison with the expected rate derived from a large population
Relative risk - Incidence in a population with a specific characteristic compared to that in a population without the characteristic
Study Designs
Study designs useful to epidemiology include the following:
Descriptive design - Used to define the characteristics of a particular disease entity
Ecological design - Used to compare large populations (eg, populations of nations)
Prospective design - Used to identify 2 similar populations to be treated in different ways in the future for subsequent analysis
Retrospective design - Used to identify and analyze 2 similar populations that were treated in clinical trials; administered by individual institutions, by consortia, and by national and international clinical trial groups, often with oversight by the National Cancer Institute (NCI) of the National Institutes of Health (NIH) and the US Food and Drug Administration (FDA); drug development monitored by The Cancer Therapy Evaluation Program (CTEP) of the NIH
Clinical Drug Trials
New cancer drugs were historically adapted for pediatric use after they were first used in adult patients. New drug development has recently incorporated pediatric trials performed after adult trials, which follow research and development in private industry and academia.
A typical protocol for a clinical trial includes the following information: objectives of the trial, background, patient eligibility criteria, study design, treatment plan, drug information, treatment evaluation criteria, data collection methods, plan for statistical analysis, consent form to be signed by the patient (or parent or guardian) and the investigator, assent by a minor patient, supporting references, and relevant appendices.
Phase 1 trials
Phase I trials are specifically designed to assess toxicity and thus appropriate dosing. Pediatric patients are treated in cohorts of 3 starting at a dose that is either 75% the adult dose or 10% the lethal dose in mouse studies. The dose is increased in predetermined steps for each new cohort of patients. Toxicity is assessed in several body systems, and a level of dose-limiting toxicity (DLT) is defined. If DLT occurs in at least 1 of the 3 patients, the protocol drops back to the previous dose level, unless the DLT involves only hematologic toxicity in a patient with a hematologic malignancy. Alternative means of identifying dosage can come from studies of toxicity in animals, using a modified Fibonacci scheme. Another method uses continual reassessment in order to escalate to potentially efficacious dosage, risking the encounter of toxicity. Reliance on adult experience is helpful, but obviously not a given, in pediatric-only disease. [2, 3, 4]
Phase 2 trials
Phase 2 trials are typically designed to directly assess the efficacy of a drug in different tumor types. A dose presumed to be safe from the results of phase 1 trials is used. An objective measure of response, such as percentage decrease in tumor size on radiographic imaging or remission assessment within a given period of time during induction, is used to evaluate efficacy. Phase 2 trials typically involve a 2-stage process to establish a firm likelihood and then to measure small differences using statistically significant sample sizes. [5, 6]
Phase 3 trials
Phase 3 studies are intended to test the efficacy of novel ways of using drugs (eg, combination chemotherapy, neoadjuvant therapy, timing variations, dose intensification) compared with standard therapy or the natural history of the disease. In addition, this may include a novel drug in combination with accepted therapy as a therapeutic window to assess efficacy in a combined phase 2/3 approach. The design must allow investigators to measure and account for potential false-positive and false-negative data. The potential for error can be calculated and used to decide on the number of patients who need to be enrolled to ensure a certain level of confidence in the results.
A type I error occurs when the P value suggests that a proposed treatment is better than the standard treatment when it is not. [7] The P value is the probability of obtaining the observed data (or data that are more extreme) if the null hypotheses were exactly true. Phase 3 trial design can be sequential to allow data to be continuously evaluated to find effective treatments as quickly as possible. However, type I errors can be magnified in this type of trial. This phenomenon can be ameliorated by requiring increased significance for the study. Factorial designs can examine several factors using a randomization method. Equivalence trials can be designed to determine if a treatment strategy of reduced duration and dosage is as effective as standard therapy.
A key element in phase 3 trials is the inclusion of at least one question that is randomized among alternative possibilities. The randomization mechanism ensures that patients are allocated to respective arms without bias. A method of allocating patients based on random numbers removes predictability from the assignment. Stratification is also desirable to group patients with identifiable prognostic characteristics. [8]
Phase 4 trials
In phase 4 trials, investigators apply positive findings from research centers to generic use in the community. Phase 4 studies can include large-scale population analyses for marketing and drug promotion by a company or for surveillance as mandated by the FDA. Phase 4 trials can also be conducted for safety and efficacy analysis of already approved drugs. These trials can include the use of controlled randomized studies to study different preparations of already approved agents.
Cancer Incidence
Incidence and mortality rates of childhood cancers vary worldwide. Some of this variation may be attributable to differences in reporting. In children aged 0-14 years incidence rates range from less than 100 per million in areas of sub-Saharan Africa and India to more than 150 per million in some populations of North America and Europe. [9]
In the United States, the estimated incidence of pediatric cancers is 178.3 per million children aged birth to 19 years. [10] In the birth to 14-year-old age range leukemias account for approximately 30% of all childhood cancers, followed by tumors of the central nervous system (CNS) (26%), lymphomas (11%), soft tissue sarcoma (6%), neuroblastoma (6%), Wilms tumor (5%), and Hodgkin lymphoma (5%). Numerous rare tumor types account for the remainder. In the 15- to 19-year-old age range, lymphoma is the most common malignancy and accounts for 21% of cancers in this age group, followed by CNS tumors (17%), leukemia (14%), germ cell tumors(12%), thyroid tumors (11%), and melanoma (5%). [11]
The decreased mortality rate of pediatric cancers has been one of the major success stories of medicine in the 20th century, and mortality has continued to improve in the early 21st century. Overall mortality has decreased by more than 50% between 1975 and 2010, and overall survival rates of childhood cancers are now approximately 80%. Improvements in the survival rates of leukemias, Hodgkin lymphoma, gonadal, and renal tumors have been notable successes. [3, 12, 13]
These improvements have led to the new challenge of caring for a growing number of cancer survivors. The risk of a second cancer appearing within 20 years after an initial diagnosis of acute lymphoblastic leukemia (ALL) is approximately 10%. [14] The existence of this group also suggests that risk factors (eg, treatment, heredity, other environmental factors) might be identifiable. For instance, the risk of acute myelogenous leukemia (AML) with the 9:11 translocation is approximately 3-6% within 5 years of therapy that includes high-dose etoposide or alkylating agent therapy, depending on dosage and tumor type. Additionally, in utero exposure to diagnostic radiation has been associated with an increased risk of childhood cancer. [15]
A decade-long survey has determined that the incidence of renal carcinoma rates are increasing among children and adolescents. This study also confirmed that thyroid cancer rates are increasing and that there has been an increase in overall cancer rates among African American children and adolescents. [13, 16]
Tumors
Leukemias
Leukemias are the most common type of childhood cancer, accounting for approximately 30% of new diagnoses. The greatest advances in treatment and outcomes have occurred in leukemias, in no small part because of the ability to treat relatively large numbers of patients with uniform treatment protocols. [17]
Acute lymphoblastic leukemia
Nearly 80% of childhood leukemias are ALL. The advent of modern molecular techniques has resulted in the further dissection of ALL into several subtypes with important prognostic and therapeutic implications. For example, the TEL-AML1 translocation is present in approximately 20% of pediatric cases of ALL and is considered to be a favorable prognostic indicator. Conversely, the presence of the Philadelphia chromosome, a 9:22 translocation involving the BCR and ABL oncogenes, is a poor prognostic indicator in ALL. Recently, Philadelphia-like mutations have been identified with a similar genetic expression signature to Philadelphia chromosome positive ALL. These mutations include more than 30 rearrangements in kinase, cytokine and receptor genes and confer a similar poor prognosis as the BCR-ABL translocation. Other poor prognostic indicators include MLL gene rearrangement at 11q23, which is associated with infant ALL, and hypodiploid ALL(Table 1). [18, 19, 20, 21]
Although ALL incidence peaks at 2-3 years of life, it represents an even greater proportion of leukemia cases in older children because the number of acute myelogenous leukemia (AML) cases further decline with age. Rates of ALL in the United States are highest in Hispanic children, and lowest in black children. [18]
Predisposing genetic conditions are associated with ALL, including Down syndrome, Bloom syndrome, Wiskott-Aldrich syndrome, ataxia telangiectasia, and other immunodeficiency syndromes. Environmental factors have also been implicated. Radiation exposure has been most tightly linked to ALL in children. Although the effect of radiation has been difficult to quantify, the risk of in utero exposure has been reported to be significant. [22, 23, 24, 25, 26]
Table 1. Genetic markers in ALL and prognostic implications (Open Table in a new window)
Name |
Location |
Prognosis |
TEL-AML1 |
t12:21 |
favorable |
MLL |
11q23 |
Poor, worse in infants |
Hypodiploid |
poor, worse < 44 chromosomes |
|
Philadelphia chromosome |
t9:22 |
poor prognosis |
Ph-like mutation |
>30 rearrangements, include ABL1, ABL2, CSF1R, PDGFRB, EPOR, JAK2, CRLF2 |
poor prognosis |
Acute myelogenous leukemia (AML)
Approximately 18% of childhood leukemia cases involve AML. This ratio of ALL-to-AML remains constant throughout childhood, except for a predilection for AML in the neonatal period. AML comprises a heterogeneous array of subtypes. Molecular diagnostic methods have advanced the ability to subtype myeloid leukemias; the analysis of translocations helps to define and confirm the histologic designations. [27, 28]
For example, the t(8:21) translocation is found in 15% of patients with AML, and this translocation is a favorable predictor of long-term survival. The acute promyelocytic subtype, which is associated with a 15:17 translocation, is similarly correlated with a favorable outcome by virtue of its response to therapy with all–trans-retinoic acid. In contrast, the chromosome 9:11 translocation associated with the monocytic subtypes indicates a poor prognosis. Abnormalities of chromosome 11 at the malignant lymphoma, lymphoblastic (MLL) locus are often observed in individuals with secondary AML after treatment with etoposide. [29, 30] Abnormalities in the oncogene, FLT-3, such as internal tandem duplications and loss of whole or parts of chromosomes 7 and 5, are associated with poorer outcomes. [31, 32]
Several environmental exposures are known to be associated with development of AML. Exposure to ionizing radiation in Japan resulted in increased AML risk. Organic solvent exposure has also been associated with AML. Exposure to chemotherapeutic agents such as topoisomerase II drugs and alkylators also predispose to secondary AML. A long list of genetic diseases are also associated with AML. [33, 34, 35]
Chronic leukemias
Chronic leukemias account for less than 5% of all pediatric leukemias. Chronic myelogenous leukemia (CML) is the most common chronic leukemia of childhood. Incidence increases with age, with rate of 0.7 per million per year in infancy and increasing to 1.2 per million per year in adolescence. [36] Similar to adult CML, imatinib is now the frontline treatment and has resulted in improved survival. [36] Juvenile myelomonocytic leukemia (JMML), a chronic leukemia that lacks the BCR-ABL fusion, is a disease found in younger children, with most cases diagnosed in children younger than 2 years. Other rare forms of chronic childhood leukemia include chronic myelomonocytic, monocytic, and lymphocytic leukemias. [37]
Brain Tumors
Tumors of the CNS are the second most common type of childhood cancer and comprise roughly 20% of childhood cancers. They are also the leading cause of childhood cancer related mortality. [38] Incidence of brain tumors increased in the 1990s, likely related to increased detection with better access to MRIs, and since the 1990s has remained stable. [39, 40] Most pediatric brain tumors occur in the first decade of life. Unlike adult brain tumors, most childhood brain tumors occur in the posterior fossa. [41]
Gliomas are the most common pediatric brain tumors. Low grade gliomas comprise 24% of pediatric brain tumors. Pilocytic astrocytomas are the most common type of low grade glioma in children and are rarely associated with transformation to high grade gliomas. [39, 42]
High grade gliomas comprise approximately 10% of pediatric brain tumors. Molecular markers can predict prognosis, and histone 3 (H3) K27 mutations in particular have poor prognosis. Other poor prognostic markers include EGFR or MYCN mutations. IDH1 mutations are rare in pediatric patients but have better prognosis when present. Diffuse Intrinsic Pontine Gliomas (DIPG), a subset of high grade gliomas, are often associated with mutations of histone H3.3 or H3.1 that are not found in adults. Histone H3-K27 mutations in DIPG are associated with worse prognosis. [39, 42]
Ependymomas originate from radial glial cells and can be found in the brain and spinal cord. Spinal ependymomas are found more commonly in patients with neurofibromatosis type 2. They are classified into Group A and B; Group A is more common in infants and has a poor prognosis. Group B ependymomas occur in adolescents and have a better prognosis. [42]
Medulloblastomas are the most common posterior fossa tumor. These tumors are embryonal in origin. Traditionally they have been classified by histologic subtype (classic, desmoplastic, and large/anaplastic), however recently they have been further classified into molecular subtypes based on transcriptional patterns. There are four molecular subtypes: Wnt, Sonic Hedge Hog (Shh), Group 3, and Group 4. Wnt tumors (named for mutations in inhibitors of the Wnt signaling pathway) make up 10% of medulloblastomas, are more common in children over 10 years old and have the best prognosis with over 90% five year survival after treatment. Shh tumors are named for mutations in the sonic hedgehog signaling pathway and are found in 25% of medulloblastomas. This subgroup has a bimodal distribution in infants and older adolescents, and it has an intermediate prognosis that is negatively influenced by the presence of a p53 mutation. Group 3 tumors are categorized based on their transcriptional profile, often have MYC amplification, and are also associated with SMARCA4 mutation and isochromosome 17q amount other mutations. They account for 25% of medulloblastomas. This group is more common in males, has the poorest prognosis, and is often metastatic at presentation. Group 4 medulloblastomas are also characterized by their similar transcriptional profiles but less is known about their pathogenesis. They account for 35% of medulloblastomas and are associated with and intermediate prognosis (Table 2). [42, 43, 44, 45]
Other rare embryonal tumors include atypical teratoid/rhabdoid tumors (ATRT) and primitive neuroectoderm tumors (PNET). ATRT was recently added in 2000 to the WHO classification. It is most often a supratentorial tumor, and more commonly found in children < 3 years old. PNET can occur in the posterior fossa or supratentorial, and both are associated with poor prognosis. [46]
Various genetic syndromes cause predisposition to development of CNS tumors. Neurofibromatosis type 1, associated with mutation in NF1 gene, is the most common predisposition syndrome and causes an increased risk of gliomas. Other predisposition syndromes and their associated genetic mutations include neurofibromatosis type 2 (NF2 gene), Li-Fraumeni (TP53 gene and CHEK2), tuberous sclerosis (TSC2 genes), von Hippel-Lindau disease (VHL gene), and Gorlin syndrome (PTCH1 and SUFU genes). [39, 47, 48] Environmental exposures are also associated with increased risk of CNS tumors. Radiation in the treatment ALL is associated with increased risk of CNS tumors. [49] Additionally, radiation therapy in medulloblastoma is associated with an increased incidence of secondary malignant brain tumors, with some studies citing incidence as high as 4%. [50]
Table 2. Medulloblastoma characteristics by subtype (Open Table in a new window)
Subtype |
Demographics |
Prognosis |
Wnt |
More common in children > 10 |
Best, >90% EFS |
Shh |
Bimodal age distribution |
Intermediate, worse with P53 mutation |
Group 3 |
More common in males |
Poor |
Group 4 |
Peak in late childhood |
Intermediate, worse in infant |
Hodgkin lymphoma
Rates of Hodgkin lymphoma, which accounts for 5% of childhood cancers, has a multimodal distribution with peaks in children younger than 14 years, in young adults, and in adults older than 55 years. Most statistical reports comment on childhood cancers in individuals aged 14 years or younger. Like non-Hodgkin lymphoma (NHL), Hodgkin lymphoma is reported to be associated with immunodeficiency and infection with the Epstein-Barr virus (EBV) as well as cytomegalovirus (CMV). [51]
Classification of Hodgkin lymphoma includes specific subtypes, including nodular sclerosing, lymphocyte predominant, mixed cellularity, and lymphocyte depleted. Nodular sclerosing is the most common subtype. Lymphocyte depleted is the least common subtype is associated with severe disease and worse outcomes. Overall Hodgkin Lymphoma has an excellent prognosis, but is associated with risk of secondary malignancy and late effects of chemotherapy. Breast cancer in young patients with a history of Hodgkin lymphoma is mostly associated with irradiation as a treatment modality and the risk is increased in those less than 30 at the time of radiation therapy, as well as in those with a cumulative dose of radiation greater than 25 Gy. Treatment for Hodgkin lymphoma in the last decades has moved towards reducing therapy to minimizing late effects given the high cure rate. [52, 53, 54]
Neuroblastoma
Neuroblastoma is the most common non-CNS solid tumor. Both long-term survival and short-term treatment remain challenges in the care of patients with neuroblastoma. Neuroblastoma has a wide range of clinical presentations and prognoses, and treatment is based on risk classification. Of interest, patients under age 18 months at presentation have a generally good prognosis. The type of neuroblastoma that emerges in infancy greatly improves the likelihood of long-term survival and is marked by a lack of N-myc amplification, by hyperdiploidy, by low-stage, limited distant sites in stage I or II disease (marrow, liver, or skin involvement in < 10% of patients), by the absence of 1p chromosomal abnormalities, by a lack of changes on chromosome 17, and by evidence of neuronal differentiation. However, the form that emerges in later years has a worse prognosis, especially in setting of n-myc amplification. Associations with genetic alterations have been characterized, including germline mutations in the ALK gene and chromosome 1p deletions. [55, 56]
Non-Hodgkin lymphoma (NHL)
Lymphomas make up a large, if heterogeneous, category of childhood cancers. Chief among these cancers are the NHLs, which are responsible for 6% of all pediatric cancers. Overall incidence of NHL increases with age; however, NHL is more prevalent than Hodgkin lymphoma in the first decade of life. It has an overall predilection for boys, likely because of the male predominance of T-cell lymphoma. A major factor in NHL is its association with immunodeficiency secondary to underlying genetic diseases, viral infection, or drugs. [57, 58, 59, 60]
Burkitt lymphoma, which accounts for roughly 50% of all NHLs, and 2-3 among childhood cancers, is associated with EBV infection and is endemic on the African continent. In its endemic form, the incidence of Burkitt lymphoma can increase as much as 50-fold. Endemic Burkitt lymphoma is associated with EBV and appears to occur in equatorial Africa. Additional environmental factors appear to be at work in the pathogenesis of Burkitt lymphoma, because the endemic form differs from the sporadic form, which can also be found along with EBV in North America, as the breakpoints of the 8:14 translocation differ. [60, 61, 62]
Lymphoblastic lymphomas comprise approximately 25% of NHL. [60] Most lymphoblastic lymphomas resemble T-cell ALL in epidemiological incidence and male predominance, with a constant incidence amongst age groups. No virus or chromosomal abnormality has been associated with lymphoblastic lymphomas. [63, 64]
The large cell lymphomas comprise approximately 25% of NHL cases. [60] Different forms including anaplastic (ALCL), diffuse, and mediastinal lymphomas are observed. [65] This variant is associated with EBV in the setting of HIV. ALCL is often associated with anaplastic lymphoma kinase (ALK) gene translocation and is classified as ALK+ or ALK- based on the presence of the translocation. ALK+ disease has better prognosis, and is present in 90% of pediatric ALCL. Poor prognostic factors in pediatric ALCL include liver, lung, or spleen involvement, mediastinal disease, elevated LDH and diffuse skin disease. [66] These tumors are very chemoresponsive leading to to survival rates close to 90%. [60]
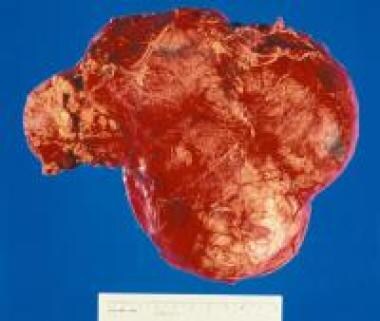
Renal Tumors
Wilms tumor is the most common renal tumor and comprises approximately 5-6% of childhood cancers overall; however, in infancy, related tumors such as mesonephric nephroma are more common. [67, 68]
As in neuroblastoma, patient age affects the prognosis in that patients who present in infancy have the best outcomes. Wilms tumor is strongly associated with a host of genetic syndromes, including Beckwith-Wiedemann syndrome; Denys-Drash syndrome; and Wilms tumor, aniridia, genitourinary abnormalities, and intellectual disability (WAGR) syndrome. Studies of chromosome 11 have led to the description of the products of the WT1 and WT2 genes, which are associated with WAGR and Denys Drash syndrome and Beckwith-Wiedemann syndrome, respectively. WT1 is found on the short arm of chromosome 11 (11p13) and is required for normal nephrogenesis; mutation leads to loss of function of this gene. WT2 is a tumor suppressor gene, and mutation leads to underexpression of the H19 tumor suppressor gene and overexpression of IGF2. [69] Prognostic factors associated with long-term survival in Wilms tumor include low-stage disease, favorable histology, and young age. [70, 71]
Retinoblastoma
With an overall incidence of 2%, retinoblastoma is a relatively rare but classic solid tumor. The study of retinoblastoma led to the development of the 2-hit hypothesis of carcinogenesis. Studies of family trees and analysis of known mutations have demonstrated an incidence of unilateral/sporadic (60%), unilateral/inherited (15%), and bilateral/inherited (25%). Hereditary retinoblastoma occurs early, often at birth and 80% before age 2 years, and is most likely to be bilateral. This implies that the first “hit” was likely inherited in the germline and that a second mutation is necessary for the transformation to malignancy.
Incidents of sporadic retinoblastomas are most likely to be unilateral by virtue of the lower likelihood of two hits occurring in a normal somatic cell. Inherited retinoblastoma cases illustrate the importance of the RB protein in suppressing tumorigenesis in that patient, and those with inherited retinoblastoma remain at risk for other tumors, chiefly osteosarcoma. [72, 73, 74, 75, 76]
Rhabdomyosarcoma
Rhabdomyosarcoma is the most common soft tissue sarcoma of childhood and comprises roughly 3% of childhood cancers. It is the 3rd most common solid tumor of childhood after Wilms Tumor and Neuroblastoma. [77] The incidence peaks in children younger than 6 years and again in early adolescence. [78] It is more common in males than females. [79] The age at diagnosis roughly correlates with the type of tumor. Head and neck tumors are generally diagnosed in young patients (two thirds of cases), and the histology is usually embryonal. Older patients (one third of cases) are most likely to have tumors in the extremities with alveolar histology. Patients with embryonal rhabdomyosarcoma have better outcomes with 5 year survival approximately 75% in this group, compared to approximately 50% in patients with alveolar rhabdomyosarcoma. [79] More recent studies have suggested that presence of the PAX/FOXO1 fusion gene may account for poorer outcomes in the alveolar group, and patients with alveolar histology and negative fusion gene have similar outcomes to patients with embryonal histology. [80] Associations with Li-Fraumeni syndrome, Beckwith-Wiedemann, and neurofibromatosis have all been reported. [81, 82, 83]
Osteosarcoma
Osteosarcoma is a bone tumor associated with the rapid bone growth characteristic of the adolescent growth spurt. Although more common overall, it is less common than Ewing sarcoma in the first decade of life. [84, 85] Osteosarcoma is most common in patients who are taller than their peers and has a female predominance when diagnosed at an early age. Tumors are localized to the metaphyseal part of long bones, with most common sites including distal femur (30%), proximal tibia (15%), and proximal humerus (10%). Prior exposure to radiation and alkylating agents has been implicated in the etiology of osteosarcoma, along with retinoblastoma and Li-Fraumeni syndrome. [86, 87]
Ewing sarcoma
Ewing sarcoma represents a group of tumors that includes peripheral primitive neuroectodermal tumors and primary bony tumors. The diagnostic standard involves detection of either the chromosome 11;22 or the 21;22 translocation (EWS-FLI-1 and EWS-ERG respectively), [88] at least one of which is found in as many as 95% of individuals with Ewing sarcoma. An interesting feature of Ewing sarcoma is its extreme rarity among blacks and significant occurrence in whites. [84] Although the greatest incidence is observed in the second decade of life, Ewing sarcoma occurs more throughout the age spectrum than does osteosarcoma. Ewing sarcoma is not associated with rapid bone growth and may be found anywhere along the bone or adjacent soft tissue or may even occur as an isolated soft-tissue mass. The most common sites of Ewing sarcomas are the pelvis (26%), femur (20%), tibia (10%), and chest wall (16%). [89]
Cancer Predisposition Factors
Relatively few causative factors have been identified for childhood cancer. The increased numbers of adults with cancer have enabled the ascertainment of causative factors, such as alcohol and smoking, whereas the small numbers of children with cancer have made environmental factors difficult to evaluate. However, analysis for inherited factors is increasingly fruitful, given the explosion in availability of molecular biologic technology and DNA sequencing. [90]
Inherited Predisposition
At its most basic level, cancer is a genetic disease. Production of genetic instability that confers some kind of mutator phenotype is most likely the chief characteristic of any inherited predisposition for cancer. These instabilities take several forms: (1) Mutations causing increasing chromosomal breakage and interfering with DNA repair (Fanconi anemia, ataxia telangiectasia), (2) mutations in signaling pathways leading to cell differentiation (eg Neurofibromatosis type 1), (3) mutations causing shortened telomere length (eg, Shwachman diamond syndrome) (4) complex chromosomal syndromes that increase the person's susceptibility to develop cancer (eg, Down syndrome). [90, 91, 92, 93]
Down syndrome
Children with Down syndrome have a 1% risk of developing leukemia before age 10. The ratio of types is different in these children than in children overall in that 60% of children with Down syndrome develop acute lymphoblastic leukemia (ALL), and 40% develop acute myelogenous leukemia (AML). More recent studies have shown that patients with Down syndrome and ALL have decreased overall survival compared to patients without Down syndrome. [94] In contrast, outcomes tend to be better in AML in children with Down syndrome than in children without Down syndrome. Interestingly, AML in Down syndrome is skewed toward the megakaryoblastic form. AML in Down syndrome is associated with a mutation in the key hematopoietic transcription factor GATA1 and results in upregulation of megakaryocytic precursors. [95] Roughly 10% of patients with Down syndrome may have associated transient myeloproliferative disease (TMD) of infancy. TMD is a self limited process that resembles congenital leukemia but also confers a 20-30% risk of subsequent AML. [96] Poor prognostic factors in AML in the Down syndrome population include age >4 years and relapsed or refractory disease. [95]
Turner syndrome
Retention of the Y chromosome in female individuals with Turner syndrome mosaicism or androgen insensitivity syndrome increases the lifetime risk of gonadoblastoma. This risk is as high as 25% by adulthood. [97]
Wilms tumor
Association of gross deletions at the 11p13 locus with Wilms tumor led to isolation of the WT1 gene. Clinical abnormalities associated with WT1 mutations include aniridia, genital abnormalities, and intellectual disability. As many as 40% of individuals with Wilms tumor have some familial component.
Syndromes associated with increased growth have also been associated with Wilms tumor. Examples include the Beckwith-Wiedemann syndrome and hemihypertrophy. Beckwith-Wiedemann syndrome is linked to chromosomal band 11p15, where the WT2 gene resides. WT2 is linked to expression of IGF2 and H19. [69, 71]
Mendelian Inheritance of Genetic Cancer Predisposition
Autosomal dominant disorders
In his study of retinoblastoma, Knudson first described the 2-hit hypothesis of carcinogenesis. [75] This hypothesis describes the process whereby, given the genetic transmission of these disorders through the germline, the loss of a second allele of the same gene in a predisposed patient leads to the onset of cancer at an early age. Germline defects in one allele may predispose the person to or may promote the loss of the other corresponding allele. These disorders are more likely than other cancers to be associated with bilateral and multiple tumors. Concomitant with this risk is the person's risk of developing several tumors at various times during his or her lifetime, depending on the tissue at risk.
With regard to retinoblastoma, the deleted RB gene not only increases the risk of the patient born with the mutation but also entails unknown risk for 2 other groups: patients with newly diagnosed sporadic cases and familial carriers who do not develop retinoblastoma as children. Mutation in the RB gene also confers a lifetime risk of osteosarcoma and melanoma. [75, 98]
The p53 gene represents the gene most commonly mutated in human cancers and is the dysfunctional gene responsible for the rare familial Li-Fraumeni cancer syndrome. Numerous cancers cluster in Li-Fraumeni cancer syndrome, including sarcomas, breast cancer, leukemia, brain tumors, and adrenocortical carcinoma. The study of Li-Fraumeni syndrome has improved our understanding of cancer in general because p53 appears to be a convergence point for many cancers in the long, multistep process of carcinogenesis. [99]
The development of several colonic polyps is associated with the early development of familial colon cancer and hepatoblastoma. The APC gene was found by positional cloning. This gene affects cellular signaling pathways by means of the beta-catenin pathway. [100]
Hereditary nonpolyposis colon cancer (HNPCC) was first defined as a genomic instability disorder in which the underlying genetic defect promotes the loss of the other allele, giving rise to the tumor. The HNPCC group involves at least the mismatch repair proteins that are implicated in an array of adult cancers. The mismatch repair genes are analyzed at the protein level and as an in vitro test to determine a person's carrier status for HNPCC. [101]
The gene complex for multiple endocrine neoplasia (MEN) is marked by an association of cancers of the thyroid, parathyroid, pancreas, pituitary, and adrenal medulla. MEN type 2 syndrome appears to be due to activating mutations of the ret oncogene rather than to a 2-hit mechanism. [102]
Neurofibromatosis type 1 is one of the most common genetic syndromes and is marked by a propensity to cause brain tumors and peripheral nerve sheath tumors. Mutations in the RAS guanosine triphosphatase (GTPase) gene, termed neurofibromin, are sporadic in at least one half of the cases of neurofibromatosis detectable in the general population. The frequency is 1 case per 3000 persons. Patients with neurofibromatosis type 1 are prone to develop optic gliomas, most commonly in early childhood, along with gliomas in other locations. A link to the development of myeloid leukemias is also described; this link is consistent with the connection between RAS mutations and myeloid disease. Associations with many other diseases are reported but not proven. [103]
Tuberous sclerosis is a syndrome of seizures, intellectual disability, and angiofibromas. Tuberous sclerosis is associated with a range of benign growths. Cardiac rhabdomyomas are a problem of infancy, whereas retinal hamartomas and giant cell astrocytomas develop later in childhood. [104]
Von Hippel-Lindau syndrome involves an association of renal cell carcinoma, retinal and cerebellar angiomata, and pheochromocytoma. The VHL gene product is an elongin that is responsible for normal transcription completion. [105]
Autosomal recessive disorders
Xeroderma pigmentosum results from several genetic complementation groups that are part of the nucleotide excision repair system and transcriptional apparatus. Patients with xeroderma pigmentosum are at increased risk for basal cell carcinoma, squamous cell carcinoma, and melanoma. Neurologic and other skin findings are also part of the related disorders trichothiodystrophy and Cockayne syndrome. [106]
Ataxia telangiectasia is a radiation hypersensitivity syndrome that comprises a constellation of ataxia, oculocutaneous telangiectasia, and increased incidence of lymphoid malignancies. The gene product responsible for this disease is the ATM (ataxia-telangiectasia mutated) phosphoinositide (PI) 3-kinase. The protein participates in the Rad50-BRCA1 epistasis group; it is also probably involved in double-strand break repair by means of homologous recombination. [107]
Bone marrow failure disorders
Fanconi anemia, a disorder of hypersensitivity to bifunctional alkylating agents, is marked by congenital defects, bone marrow failure, and susceptibility to several cancers (most commonly AML). At least 22 genes are defective among the known complementation groups for Fanconi anemia. [108] Although many genes have been cloned, the molecular mechanism of the Fanconi anemia pathway remains complex but appears to converge upon the homologous recombination pathway by virtue of the involvement of BRCA genes and RAD51 as bona fide FA genes. [109, 110]
Other marrow failure syndromes include Kostmann disease, Shwachman-Diamond syndrome (SDS), dyskeratosis congenita (DC), and Diamond-Blackfan anemia (DBA). These syndromes display marrow failure to one extent or another. Even Diamond-Blackfan anemia, although typically resulting in isolated red cell failure, can affect all blood cell lines. Although rare, all bone marrow failure syndromes result in the increased risk of leukemia, probably as a combination of a bone marrow under stress coupled with the underlying molecular defect. [111] SDS, DC, and DBA in particular all share defects in RNA processing, among others. [112]
Immunodeficiency States
Severe combined immunodeficiency
Severe Combined Immunodeficiency (SCID) is caused by genetic mutations that result in dysfunctional B and T cells. It is a rare disorder, seen in approximately 1: 50,000 births, and is more common in males than females. [113] The biology of patients with SCID is difficult to examine because of the heterogeneity of these disorders and the severity of their underlying defect. However, their inherent propensity toward lymphoid malignancy is clear. Mutations associated with SCID include defects in recombination activating genes 1&2 (RAG1, RAG2). Reticular dysgenesis is a rare form of SCID characterized by mutation in adenylate kinase 2 gene (AK2), that is associated with lymphopenia as well as neutropenia. [114]
Other T cell disorders can present with a similar phenotype to SCID. Immune dysregulation, polyendocrinopathy, enteropathy, X-linked (IPEX) is characterized by a mutation in the FOXP3 gene, which is responsible for T-cell regulation, and is associated with lymphadenopathy and hepatosplenomegaly. [114] DiGeorge syndrome is part of the family of 22q11.2 deletion syndromes, and is characterized by immunodeficiency, hypoparathyroidism and congenital heart disease. The immunodeficiency is caused by thymic aplasia and absence of T cells and is associated with lymphoproliferative disorders. [115, 116, 117, 118] CHARGE syndrome is characterized by coloboma, heart defects and choanal atresia, growth retardation, genital abnormalities and ear abnormalities, but is also associated with immunodeficiency that include T cell lymphopenia and hypogammaglobulinemia. It is characterized by a mutation in the chromodomain helicase DNA binding protein-7 (CHD7). [114]
Wiskott-Aldrich syndrome
Wiskott-Aldrich syndrome (WAS) is an immunodeficiency disorder characterized by thrombocytopenia, eczema, and T-cell dysfunction. It is found in approximately 1 to 10 of every 1 million births and it is caused by a mutation in the WAS gene. Malignancies are reported in as many as 13-22% of patients with WAS. The most common associated malignancies are lymphoma, leukemia, and myelodysplasia. [119, 120]
Lymphoproliferative syndromes
Lymphoproliferative syndromes increase the risk of lymphoid proliferation triggered by Epstein-Barr virus (EBV) infection. The genetic syndromes are associated with mutations in genes regulating apoptosis. The X-linked form is associated with mutations in the SAP and XIAP genes, in type 1 and 2 disease respectively. EBV infection accounts for 70% of deaths in these patients. After prolonged immunosuppression (eg, chronic graft versus host disease after bone marrow transplantation), the patient's susceptibility to lymphoproliferative disease increases. [121]
Autoimmune lymphoproliferative syndrome (ALPS) is marked by chronic lymphadenopathy and associated autoimmune cytopenias. Laboratory findings in these patients are notable for a T cell population that is CD4 and CD8 negative, referred to as double negative T cells. ALPS is associated with mutations in FAS, FASL, and CASP10. [122]
HIV infection
HIV has not left the pediatric population unaffected, despite advances in preventing vertical transmission and promotion of safe sex practices. There has been a shift in the pattern of HIV associated malignancies in the last 2 decades as highly active anti-retroviral therapy (HAART) has become common practice. Prior to HAART therapy, the rate of malignancy was 2.5% in HIV patients in the US, with NHL accounting for the most common HIV associated neoplasm in children, followed by Kaposi sarcoma and leiomyosarcoma. [123] Since the incorporation of HAART therapy incidence of kaposi sarcoma and NHL have both decreased, while leiomyosarcoma has become more common. [124]
Environmental Factors
Ionizing radiation
Although increased cancer rates in children have been associated with radiation exposure, no threshold effect has been noted. Data derived from the atomic bomb exposures at Hiroshima and Nagasaki represent the most convincing body of evidence. [125] A link also has been established between prenatal radiologic examinations in mothers and leukemia, with studies showing odds ratios of developing leukemias ranging from 1.2-1.9. [126] One study showed an effect on cancer incidence from paternal exposure; however, these data have not been reproduced. [127] The use of CT scanning is also a common source of radiation exposure and it’s use has increased in the early twenty first century. Studies show an association between cumulative dose of radiation from CT scans and risk of leukemia and CNS tumors. [128, 129]
Electromagnetic fields
Research has produced great controversy but little solid evidence of a relationship between cancer and electromagnetic fields. Published reports have suggested that electromagnetic fields have some potential effect on the promotion of leukemia. However, when the available data are combined, the relative risk is probably no more than 1.3, and in many cases no correlation has been seen. [130]
Chemicals
Most data about chemical exposure and its relationship to adult cancers imply that a lifetime of exposure is required to cause cancer. This supposition is exemplified by tobacco exposure. However, exceptions have been reported. Dioxin has been associated with many malignancies, including NHL, lung cancer and soft tissue sarcomas. [41] Trichloroethylene has been implicated in cases in Woburn, Massachusetts, suggesting a link between maternal exposure and leukemia. [131] A strong relationship has been suggested between parental exposure to chemicals and subsequent childhood cancer. Agents and their associated cancers include pesticides (CNS tumors), solvents (eg, leukemia, NHL), metals (hepatoblastoma), petroleum products (leukemia) and boron (Wilms tumor). [131, 132, 133, 134, 135]
Viral
Associations with viruses have been difficult to ascertain in childhood cancer. Perhaps the strongest link has been to Epstein-Barr virus (EBV), with a clear connection in African Burkitt lymphoma. On the other hand, a causal link remains more obscure in Hodgkin lymphoma and nasopharyngeal carcinoma, in which the EBV genome is found, but the question of etiology is less established. In the case of HIV, malignancies such as CNS lymphoma and leiomyosarcoma are correlated but are probably the result of HIV-induced immunosuppression. [136]
-
Gross nephrectomy specimen shows a Wilms tumor pushing the normal renal parenchyma to the side.