Background
Atrioventricular node reentrant tachycardia (AVNRT) is a form of reentrant rhythm within the region of the atrioventricular (AV) node. Reentrant rhythms account for most episodes of supraventricular tachycardia (SVT) in children. A reentrant rhythm involves the presence of two distinct pathways, a zone of slow conduction and unidirectional block in one limb, allowing an electrical impulse to travel down the second limb and reenter the blocked pathway from the other direction. Reentrant rhythms can usually be initiated and terminated by pacing or premature beats. During AVNRT, the circuit typically involves both a fast and a slow pathway within the region of the AV node, which allows the impulses to proceed down the His-Purkinje system to the ventricles while simultaneously proceeding in a retrograde fashion to depolarize the atria and reenter the node.
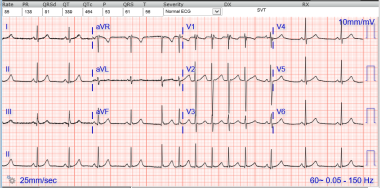 Atrioventricular Node Reentry Supraventricular Tachycardia. Nonsustained atrioventricular node reentry tachycardia (AVNRT). This electrocardiogram is from a 10-year-old who is in sinus rhythm until a junction escape beat initiates a 5-beat run of supraventricular tachycardia. The heart rate is quite slow at 130 beats per minute, likely due to his resting state (higher vagal tone) and treatment with the beta-blocker atenolol. Note the pseudo R' waves in lead V1. These deflections represent retrograde atrial activation. Some patients may also exhibit pseudo S waves in the inferior leads. The R' waves are lost when the tachycardia ends, demonstrating that the R' wave is not associated with ventricular depolarization. The terminal QRS has no R' wave, indicating that the tachycardia terminated in the retrograde limb of the circuit (fast AV nodal pathway).
Atrioventricular Node Reentry Supraventricular Tachycardia. Nonsustained atrioventricular node reentry tachycardia (AVNRT). This electrocardiogram is from a 10-year-old who is in sinus rhythm until a junction escape beat initiates a 5-beat run of supraventricular tachycardia. The heart rate is quite slow at 130 beats per minute, likely due to his resting state (higher vagal tone) and treatment with the beta-blocker atenolol. Note the pseudo R' waves in lead V1. These deflections represent retrograde atrial activation. Some patients may also exhibit pseudo S waves in the inferior leads. The R' waves are lost when the tachycardia ends, demonstrating that the R' wave is not associated with ventricular depolarization. The terminal QRS has no R' wave, indicating that the tachycardia terminated in the retrograde limb of the circuit (fast AV nodal pathway).
Pathophysiology
Two or more functionally and (usually) anatomically distinct pathways have been described connecting the atria to the atrioventricular (AV) node; they are known as the fast and the slow pathways and have different electrophysiologic (EP) characteristics. The fast pathway crosses the tendon of Todaro superiorly and is identified by its relatively shorter conduction time and longer effective refractory period (ERP). The slow pathway(s) approach the compact AV node from inferiorly and have a relatively longer conduction time and an ERP that typically is short when compared to the fast pathway ERP. The different EP characteristics of the fast and slow pathway(s) can be observed during EP studies as evidence of dual AV nodal physiology. However, dual AV nodal physiology is a common finding during EP studies [1] ; it is not synonymous with AV node reentrant tachycardia (AVNRT) because the incidental finding of dual AV nodal physiology does not predict AVNRT in children and adolescents after successful accessory pathway ablation. [2]
The two forms of AVNRT that are usually described are the typical form (ie, slow-fast) and the atypical form (ie, fast-slow or slow-slow), referring to the characteristic of antegrade-retrograde conduction during tachyarrhythmia. In the typical form, which represents 90% of clinical AVNRT episodes, the conduction moves in antegrade direction through the slow pathway from the atrium to the compact AVN and in retrograde direction through the fast pathway. In an atypical form, the conduction moves antegradely in the fast pathway and retrogradely in the slow pathway, resulting in a long RP interval. A third form also has been identified in which the conduction appears to be antegrade and retrograde through two discrete slow pathways. [3] Multiple atypical AVNRT circuits using rightward and leftward inferior extensions of the AV node have been described. [4] In such models, these extensions participate in the tachycardia by connections to the left atrium. [5]
Conduction during sinus rhythm usually occurs over the fast pathway, resulting in a normal PR interval. A premature atrial beat may cause a unidirectional block in the fast pathway (because of its longer ERP) but conduct via the slow pathway. The slow pathway has a longer conduction time than the fast pathway, providing a delay of the impulse; therefore, when it reaches the distal end of the fast pathway (which has by that time recovered from refractoriness), the impulse is conducted retrograde via the fast pathway. After traversing a short portion of the low septal right atrium, it then reenters the slow pathway again, creating a circus movement tachycardia.
The natural history of AVNRT in children is unknown, but some infants appear to exhibit spontaneous resolution. The substrate for atrioventricular tachycardia is not fully understood, but cell-to-cell interactions may play a role. [3]
Etiology
The incidence of atrioventricular node reentrant tachycardia (AVNRT) appears to be increased in the setting of congenital heart disease. In addition, related conditions, such as twin AV node (AV node-to-node reentry) with a Mönckeberg sling, may occur in the setting of complex congenital heart disease. Finally, dual AV nodal physiology may be a bystander to accessory pathways, and accessory pathways, including Mahaim fibers, may be bystanders to AVNRT.
One report detailed evidence that AVNRT may have a familial inheritance in some cases, which is suggestive of a genetic mechanism. [6]
Epidemiology
United States data
Atrioventricular node reentrant tachycardia (AVNRT) is the most common cause of paroxysmal supraventricular tachycardia (PSVT). Approximately 89,000 new cases are reported each year, and 570,000 persons with PSVT live in the United States.
International
PSVT has a prevalence of 2.25 per 1000 population and an incidence of 35 per 100,000 person-years.
Sex- and age-related demographics
Prevalence of AVNRT is more common in females than in males, particularly in adults.
AVNRT is considered less common in newborns and increases in prevalence throughout childhood. However, some reports suggest that AVNRT may be underrecognized in infancy. [7] AVNRT is the predominant mechanism (accounting for 40-50% of cases) of SVT in adults. [8]
Prognosis
The diagnosis of atrioventricular node reentrant tachycardia (AVNRT) is associated with unpredictable occurrences that pose a nuisance and interfere with quality of life more than they are life threatening.
Morbidity/mortality
Episodes of supraventricular tachycardia (SVT) caused by any mechanism, including AVNRT, have a minimal impact on mortality in children, although SVT may lead to some degree of morbidity. Rare cases of AVNRT in young infants may be associated with more significant morbidity and possible mortality. The presence of dual AV node physiology per se does not necessarily indicate morbidity. Discontinuous AV nodal conduction curves observed during an electrophysiologic study that suggest the presence of dual AV nodal pathways have been encountered in patients without SVT and occur in approximately 63% of children. However, the presence of dual AV node physiology with associated AVNRT is a common mechanism for SVT in children and adults. Thapar and Gillette's publication showed that dual AV node physiology was the mechanism in 46% of children who presented for evaluation of arrhythmias. [9]
Patients with dual antegrade conduction in the AV node generally have good long-term outcomes following catheter ablation. However, diagnosis and management may be challenging in the presence of autonomic tone-dependent changes in ante- vs retrograde conduction via the slow and/or fast pathway(s). [10]
Patient Education
Patients beyond infancy are usually informed that their condition, despite the severity of symptoms, is not significantly life threatening. Vagal maneuvers are taught, and the options of intermittent treatment (eg, vagal maneuvers, emergency department visits), long-term drug therapy, and slow pathway modification with radiofrequency or cryothermal energy are discussed.
For patient education resources, see Heart Health Center, as well as Supraventricular Tachycardia (SVT, PSVT), and SVT (Supraventricular Tachycardia) vs. Heart Attack.
-
Atrioventricular Node Reentry Supraventricular Tachycardia. Nonsustained atrioventricular node reentry tachycardia (AVNRT). This electrocardiogram is from a 10-year-old who is in sinus rhythm until a junction escape beat initiates a 5-beat run of supraventricular tachycardia. The heart rate is quite slow at 130 beats per minute, likely due to his resting state (higher vagal tone) and treatment with the beta-blocker atenolol. Note the pseudo R' waves in lead V1. These deflections represent retrograde atrial activation. Some patients may also exhibit pseudo S waves in the inferior leads. The R' waves are lost when the tachycardia ends, demonstrating that the R' wave is not associated with ventricular depolarization. The terminal QRS has no R' wave, indicating that the tachycardia terminated in the retrograde limb of the circuit (fast AV nodal pathway).
-
Atrioventricular Node Reentry Supraventricular Tachycardia. Low voltage bridge in atrioventricular node reentry tachycardia (AVNRT). The images are a three-dimensional electroanatomic voltage map of the right atrium in the left anterior oblique projection with caudal angulation. The purple regions represent areas of high ("normal") atrial electrogram voltage, whereas gray and red regions have lower amplitude signals. The red region projecting from the tricuspid annulus (cutout) posteriorly toward the coronary sinus (thin purple cylinder) is a potential target for slow pathway ablation. The white spherical images are locations where cryotherapy of lesions were performed. The lesion highlighted in yellow represents the location of the successful slow pathway ablation. The others are "insurance" lesions.







